Introduction
Alcoholic hepatitis is an acute inflammation of the liver secondary to alcohol use in hepatotoxic amounts and whose pathophysiology is influenced by various risk factors. On average, it affects people in the fourth and fifth decades of life, mainly males; however, in recent years, an increase in the incidence of alcoholic hepatitis has been described in women and young patients of both sexes, aged between 15 and 44 years1.
This pathology is associated with drinking more than 50 grams of ethanol per day less than four weeks prior in a patient with chronic alcohol use for more than six months. It may affect patients without underlying pathologies or with chronic liver diseases, from steatosis to liver cirrhosis, and cause acute liver failure and acute-on-chronic liver failure (ACLF), both with bleak prognoses1,2.
The diagnosis of alcoholic hepatitis is defined by criteria based on an adequate anamnesis, comprehensive and exhaustive physical examination, and compatible serological and imaging tests. Nonetheless, the final diagnosis is histopathological through liver biopsy3.
Budd-Chiari syndrome is a rare, heterogeneous, and potentially lethal entity characterized by thrombosis in the suprahepatic veins (right, middle, or left), which involves their course and the possibility of affecting the inferior vena cava (IVC)4. Timely diagnosis is essential, for which venous Doppler ultrasound is the first line diagnostic test5; however, magnetic resonance angiography has shown higher sensitivity (93%) and an area under the curve of 90.8%, compared to 88.4% and 86.6% for computed tomography angiography and venous Doppler ultrasound, respectively6.
There is a similar identity, called pseudo-Budd-Chiari syndrome, which was first described in 1977 and is poorly known and studied. There is a paucity of scientific studies addressing it, and its pathophysiology needs to be clarified. Diagnosis is difficult due to its remarkable similarity to Budd-Chiari syndrome, both clinically and by imaging studies, so invasive diagnostic methods such as liver biopsy must be used7.
Recently, the latest Baveno VII consensus considers Budd-Chiari syndrome as secondary when the mechanism of action of suprahepatic venous obstruction is associated with extrinsic compression, for example, by benign or malignant tumors or other entities that involve the liver parenchyma and are adjacent to the territory of the suprahepatic veins. Moreover, Budd-Chiari syndrome is considered primary in cases where its pathophysiology is purely related to suprahepatic vein thrombosis, as initially known8.
Case presentation
We present the case of a 51-year-old overweight male patient, a heavy transport driver, with a history of alcohol use for more than 20 years (> 60 g/day). After an episode of excessive alcohol use (> 360 g in ten hours), he was sick for 15 days and presented with jaundice in the sclerae and skin with notable progression, abdominal distension associated with pain in the right hypochondrium, and the subsequent appearance of edema in the lower limbs. The examination revealed hepatosplenomegaly painful on palpation, large-volume ascites, edema of the lower limbs (+++/+++), jaundice of the skin, and sclera (+++/+++). Neurologically, the patient was lucid and oriented in time, space, and person.
The tests taken on the patient on admission are shown in Table 1. The ascites fluid study was not pathological concerning infectious processes. The serum-ascites albumin gradient (SAAG) had a value of 2.11. Ascitic fluid, urine, and blood cultures were negative.
Table 1 Admission laboratory analysis
| TB | 12.59 |
| DB | 7.53 |
| AP | 595 |
| GGTP | 817 |
| GOT | 159 |
| GPT | 74 |
| Total protein and albumin | TP: 5.93; Alb: 2.9; globulins: 2.9 |
| Leukocytes | L: 19,200; S: 88%; B: 2% |
| Hemoglobin | 8.9 g/dL |
| Platelets | 406,000 |
| PT-INR/PPT | 1.4-16/46 |
| Peripheral blood smear | White series: neutrophilia, reactive lymphocytes 2% Red series: normochromic normocytic Platelet series: some giant platelets |
| Coombs (R and L) | Negative |
| Creatinine/Urea | 0.68 mg/dL/15 |
| CRP | 65 |
| PCT | 0.4 |
| AFP | 8.3 |
| Anti-HCV | Not reactive |
| HBs-Ac | Not reactive |
| HB-Ac core | Not reactive |
| HBsAg | Not reactive |
| Ascitic fluid study | 101 cells/mm3; mononuclear: 88%; Alb: 0.79 g/dL; LDH: 55 U/L; protein: 1.5 g/dL |
B: band; AFP: alpha-fetoprotein; Alb: albumin; Anti-HCV: antibodies against the hepatitis C virus; DB: direct bilirubin; TB: total bilirubin; AP: alkaline phosphatase; GGTP: gamma-glutamyl transpeptidase; HBs-Ac: specific antibody directed against the hepatitis B virus surface antigen; HB-Ac core: total core antibody to hepatitis B virus; HBsAg: hepatitis B virus surface antigen; PT-INR: prothrombin time with international normalized ratio; L: leukocytes; CRP: C-reactive protein; PCT: procalcitonin; TP: total protein; S: segmented; GOT: aspartate aminotransferase; GPT: alanine aminotransferase; PTT: partial thromboplastin time. Source: Clinical Pathology Service, Víctor Lazarte Echegaray Hospital.
The patient underwent an upper GI endoscopy, which revealed mild portal hypertensive gastropathy and the absence of esophageal or gastric varices; the colonoscopy showed only medium-sized congestive internal hemorrhoids without other lesions. Abdominal ultrasound confirmed hepatosplenomegaly and determined the presence of abundant free fluid in the abdominal cavity. A Doppler ultrasound of the portal vein and suprahepatic veins was performed, revealing the left suprahepatic vein of 8.4 mm and visible flow, the middle filiform suprahepatic vein of 4 mm with a visible flow, and the right suprahepatic vein of 9.4 mm with no flow. These results suggest probable thrombosis related to probable Budd-Chiari syndrome.
Therefore, we decided to perform a venous magnetic resonance angiography. It showed thinning of the right suprahepatic vein with an irregularly thinned caliber of up to 3 mm, compatible with probable thrombosis and absence of signal emptiness proximal to the IVC; thin, threadlike courses of the left suprahepatic vein and the proximal portion of the middle suprahepatic vein, suggesting probable partial thrombosis; the portal vein of 13 mm, without signs of thrombosis. The radiological report of the venous magnetic resonance angiography found the portal vein with a preserved course and a thinning of the suprahepatic veins, suggesting a probable Budd-Chiari syndrome (Figures 1 and 2).

Figure 1 Thinning of the suprahepatic veins (MRI). Source: Radiology Service, Víctor Lazarte Echegaray Hospital.

Figure 2 Thinning of the suprahepatic veins and portal vein of preserved caliber (MRI). Source: Radiology Service, Víctor Lazarte Echegaray Hospital.
Ultrasound-guided percutaneous liver biopsy was performed. The sample consisted of 15 portal triads. The histopathological report found liver parenchyma characterized by hepatocyte edema, Mallory-Denk bodies, acidophilic (apoptotic) bodies located predominantly in zone 3, associated with mixed inflammation (moderate portal inflammation and moderate interface hepatitis), necrosis in a 2-4 foci/10x patch, macrovesicular steatosis in 60%, diffuse fibrosis with the formation of centrilobular portal-vein bridges, without signs of cholestasis or congestion signs in the sinusoidal microvasculature. These findings are compatible with diagnosing non-cirrhotic alcoholic steatohepatitis with an Ishak fibrosis score of 3 (Figures 3, 4 y 5). Thus, the absence of definitive histopathological criteria for Budd-Chiari syndrome was confirmed. Maddrey’s discriminant function (32.6 points), Model for End-Stage Liver Disease (MELD) (21 points), and Glasgow Alcoholic Hepatitis Score (GAHS) (8.7 points) were calculated, arriving at a diagnosis of severe alcoholic hepatitis.
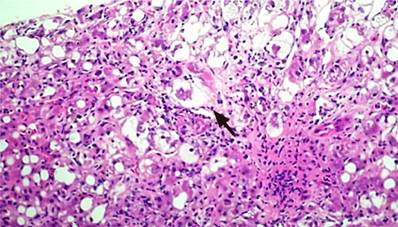
Figure 3 Macrovesicular steatosis and hepatocyte edema. Mallory-Denk body (arrow). Source: Pathology Service, Víctor Lazarte Echegaray Hospital.
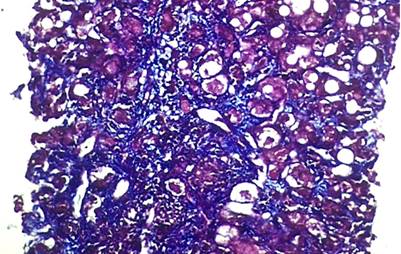
Figure 4 Masson’s trichrome stain: bridging fibrosis. Source: Pathology Service, Víctor Lazarte Echegaray Hospital.
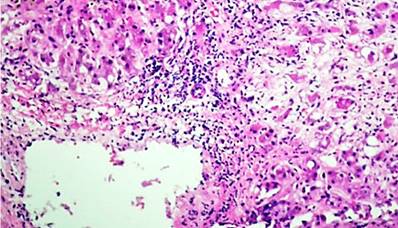
Figure 5 Inflammatory infiltrate, macrovesicular steatosis. Source: Pathology Service, Víctor Lazarte Echegaray Hospital.
Treatment based on corticosteroids was started: prednisone 40 mg/day orally with a planned schedule of 28 days and N-acetylcysteine 100 mg/kg/day for five days intravenously; anticoagulants were not administered. The Lille score was determined on the seventh day to control the response to corticosteroid-based treatment, which revealed a value of 0.08 (less than 0.45). Consequently, we decided to continue with the 28-day corticosteroid regimen.
After 28 days of completing the regimen, the follow-up analysis showed an improvement (Table 2) parallel to a good clinical evolution. The patient was discharged after 33 days of hospital stay in his baseline status as an independent person (carrying out his daily and personal care activities without help) with optimal functional status.
Discussion
The diagnosis of alcoholic hepatitis has three scenarios: probable, possible, and definitive alcoholic hepatitis. The probable one is based on the fulfillment of diagnostic criteria such as recent appearance or worsening of jaundice with or without ascites, with or without encephalopathy, associated with alcohol use in hepatotoxic doses (greater than 50 g/day) in less than four weeks prior by a person who uses alcohol chronically for more than six months. These criteria are accompanied by serological findings such as total bilirubin greater than 3 mg/dL, GOT and GPT greater than 50 IU/L and less than 400 IU/L, AST/ALT ratio greater than 2, GGTP greater than 100 U/L, serum albumin less than 3g/dL, INR greater than 1.5, leukocytosis greater than 12,000 associated with neutrophilia, variable degrees of anemia, or thrombocytopenia in cases of cirrhosis. The above excludes potentially confounding factors of the presumptive diagnosis1,3.
Possible alcoholic hepatitis is identified when the indicated criteria are met but with potentially confounding factors, as in the present case: the possibility of Budd-Chiari syndrome concomitant with alcoholic hepatitis.
Finally, definitive alcoholic hepatitis is identified by confirmatory liver histopathological findings such as infiltration of inflammatory cells at the portal and periportal levels, with certain degrees of fibrosis, macro or microvesicular steatosis with ballooning of hepatocytes, megamitochondria, and Mallory-Denk bodies as pathognomonic findings of alcoholic hepatitis.
The entity known as pseudo-Budd-Chiari syndrome was first described in 19777. Unlike Budd-Chiari syndrome, characterized by suprahepatic vein thrombosis, this syndrome has similar clinical and imaging findings. However, biopsies or autopsies fail to demonstrate suprahepatic vein thrombosis or histopathological findings compatible with the syndrome7.
In a study conducted in 2002, Janssen et al. described three cases of patients with decompensated alcoholic liver disease who had venous Doppler ultrasounds with a decreased flow in the suprahepatic veins but direct angiographies without thrombi in their lumen. Lastly, these patients underwent a liver biopsy without congestive histopathological findings due to a probable Budd-Chiari syndrome related to the initial diagnosis9.
Similar results were found by Robles-Medranda et al. in the study they conducted in 2006, based on the pseudo-Budd-Chiari syndrome associated with alcoholic steatohepatitis and liver cirrhosis. They concluded that the imaging of a decreased flow near the suprahepatic veins, probably related to Budd-Chiari syndrome, was produced by an extrinsic compression of their lumen associated with an enlarged liver parenchyma resulting from a vast inflammatory pattern due to alcoholic steatohepatitis and not by intraluminal thrombi. Thus, anticoagulation was not considered within the prescribed therapy10.
Sheth et al., in a study conducted in 2014, reported a case of alcoholic steatohepatitis masked by probable Budd-Chiari syndrome. After the liver biopsy, they determined that the mechanical compression exerted by the liver parenchyma on the suprahepatic veins is associated with the vast inflammatory infiltrate based on neutrophils and other inflammatory cells. They highlight the potential reversibility of this condition with medical treatment based on the administration of corticosteroids without the need for anticoagulation11.
It should be noted that recently in the Baveno VII consensus, carried out in 2021 and published in 2022, this entity is considered a secondary Budd-Chiari syndrome because the mechanism of action of venous obstruction is associated with extrinsic compression, as mentioned above, which may occur, for example, due to a benign or malignant tumor. Nevertheless, we can extrapolate this designation to cases in which extrinsic compression occurs due to, for example, severely inflamed liver parenchyma, as in cases of severe alcoholic hepatitis8.
Conclusion
In the case presented, severe alcoholic hepatitis is associated with imaging characteristics suggestive of Budd-Chiari syndrome, which creates confusion in the diagnosis and subsequent management of the patient. Reaching the diagnosis of secondary Budd-Chiari syndrome requires access to more complex or invasive methods, such as liver biopsy in cases like the present one. Therefore, more scientific evidence is needed to differentiate between both entities promptly and clarify on a scientific basis the best diagnostic and therapeutic course of action for these patients.











 text in
text in 



