Introduction
Gastric cancer (GC) is a global health concern that, despite an overall decrease since 1975, still occurs more frequently in men and people over 65 years of age.1 As of 2020, it ranked fifth worldwide in incidence and fourth in mortality, with 768,793 cases.2 In Colombia, the incidence was 8214 cases (7.3%) in the same year, making it the primary cause of death from neoplastic diseases, with 6451 deaths (11.7%).2 This condition usually presents asymptomatically and is often diagnosed in Colombia at an advanced stage with limited treatment options.3
In Colombia, gastric cancer (GC) causes fewer years of life potentially lost than in other countries with similar incidence rates.4 Boyacá is considered a high-risk area, along with other regions like Nariño, with mortality rates of 13.38 and 15.72 deaths per 100,000 inhabitants, respectively, in 2014.5,6 As of 2021, both departments continued to have mortality rates above the national average of 5.26 deaths per 100,000.7
The burden of disease attributable to neoplasms during 2020 accounted for 0.75% of the total disability-adjusted life years (DALYs) worldwide, corresponding to 4,581,860 DALYs. Among neoplasms, GC contributed to 0.04% of the global burden of disease, representing 246,437 DALYs. In Colombia,8 the survival rate for GC during the 2010-2014 period was between 15.4% and 18.8%, significantly lower than the US average of 33.6% for a 5-year survival rate.9 In some municipalities such as Bucaramanga (Santander), the 5-year survival rate for GC is as low as 11%,10 highlighting the magnitude of the problem at the national level.
Previous studies have examined the burden of disease in Colombia, including those focused on GC.4,11,12 However, given the unique characteristics of the Altiplano Cundiboyacense, a high plateau in the Eastern Andes Mountain Range, and Tunja (Boyacá), the highest capital city in Colombia with 179,263 residents, there is a need to investigate the burden of disease associated with secondary disability to GC in this high-risk population. While this study will not determine the prevalence of Helicobacter pylori in the city, the American Institute for Cancer Research has identified other factors, such as dietary habits (including salting of foods and low fruit consumption) and high alcohol consumption, which are prevalent in the department of Boyacá,16 and may increase the risk of developing GC.14,15
It is worth noting that 95.6%13 of Tunja’s population resides in urban areas, and the city is situated at an altitude of 2775 meters above sea level.17 According to some studies,18,19 living at an altitude above 2000 meters could contribute to the development of GC.
This study aims to estimate the burden of GC in Tunja, Colombia, measured in DALYs, using prevalence data from the Ministry of Health and Social Protection and the methodology established by the World Health Organization (WHO).
Methodology
Type of Study
This is an exploratory ecological study on disease burden, which aims to estimate the potential years of life lost due to secondary disability to GC in Tunja, Boyacá, for the period from 2010 to 2019.
Source of Information
The study obtained information on GC mortality from the National Administrative Department of Statistics (DANE) and prevalence information from the Integrated Social Protection Information System (SISPRO) records. The Ministry of Health and Social Protection of Colombia centralizes the Individual Registry of Health Service Provision (RIPS), which is the main source of SISPRO.
Data from Tunja between 2010 to 2019 were collected to conduct the analysis, including GC-related International Classification of Diseases (ICD-10) codes from C160 to C169. These codes represent malignant tumors of various stomach parts, such as the cardia, gastric fundus, antrum pyloric, pylorus, and other regions not specified. We then identified patients with the main diagnosis codes for GC, categorized by sex, life cycle, report year, and residence in Tunja. To determine the prevalence of GC, the population denominator was obtained from DANE records,20 which were grouped by life cycles per year.
Data analysis
DALYs were calculated using the WHO methodology, which involves adding together the YLL (years of life lost to premature death) and YLD (years lived with disability) measures. YLL indicates mortality attributable to the disease, while YLD indicates disease morbidity. The collected data from DANE and SISPRO were then organized into spreadsheets in MS Excel 365 for analysis. For the YLD calculation, we considered the weight per disability provided by the 2010 burden of disease study.23,24 However, we opted to use the weight per disability suggested by the expert panel in a previous study4 due to its applicability to the region. This study calculated a weighted weight of 0.278 for the time lived with GC in Colombia. We used a life expectancy at birth of 82.4 years for both men and women, and the expectation for each age range without discount rate or adjustment for age was used according to the five-year period.23 Finally, we obtained the DALYs using the WHO staff25 to calculate the burden of disease.
Results
Based on the RIPS (Individual Health Service Provision Records) collected from 2010 to 2019, 583 patients with confirmed GC diagnosis were treated in Tunja, comprising 51.5% men and 48.5% women (Table 1).
Table 1 People treated with GC diagnosis by age group and sex in Tunja from 2010 to 2019
| Age | Female | Male | Total |
|---|---|---|---|
| 5-14 | 1 | 0 | 1 |
| 15-29 | 5 | 4 | 9 |
| 30-44 | 39 | 20 | 59 |
| 45-59 | 79 | 69 | 148 |
| 60-69 | 59 | 80 | 139 |
| 70-79 | 67 | 78 | 145 |
| 80+ | 33 | 49 | 82 |
| Total | 283 | 300 | 583 |
Source: Author’s own research, based on information obtained from the RIPS, centralized by the Ministry of Health and Social Protection.
For the population aged over 30 years, the estimated 10-year prevalence of GC was 7.6 per 1000 men and 6.1 per 1000 women (Table 2).
Table 2 Prevalence of GC per 1000 inhabitants in men and women by life cycle f in Tunja from 2010 to 2019
| Life Cycle | Men | Women | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Population | Cases | Prevalence | Population | Cases | Prevalence | Población | Cases | Prevalence | |
| 5-14 | 137 625 | 0 | 0 | 137 625 | 1 | 0.007 | 275 250 | 1 | 0.003 |
| 15-29 | 260 514 | 4 | 0.015 | 260 514 | 5 | 0.019 | 521 028 | 9 | 0.017 |
| 30-44 | 214 729 | 20 | 0.093 | 214 729 | 39 | 0.181 | 429 458 | 59 | 0.137 |
| 45-59 | 166 670 | 69 | 0.414 | 166 670 | 79 | 0.474 | 333 340 | 148 | 0.444 |
| 60-69 | 62 729 | 80 | 1.276 | 62 729 | 59 | 0.940 | 125 458 | 139 | 1.108 |
| 70-79 | 29 287 | 78 | 2.666 | 29 287 | 67 | 2.290 | 58 574 | 145 | 2.478 |
| 80+ | 15 275 | 49 | 3.213 | 15 275 | 33 | 2.162 | 30 550 | 82 | 2.687 |
| Total | 886 829 | 300 | 7.678 | 886 829 | 283 | 6.076 | 1 773 658 | 583 | 6.877 |
Source: Author’s own research, based on information obtained from the RIPS, centralized by the Ministry of Health and Social Protection.
Over the course of the decade under study, 79% of the GC diagnoses occurred in individuals between the ages of 45 and 79.
As for the estimated incidence (Table 3), cases increased during the life cycles of individuals aged 60 to 79. A total of 249 deaths were identified across six age groups: 15 to 29, 30 to 44, 45 to 59, 60 to 69, 70 to 79, and 80 or older. We calculated the YLL per 1000 inhabitants for these deaths using this data.
Table 3 Estimated incidence per 1000 inhabitants between 2010 and 2019 of GC in men and women per life cycle in Tunja
| Incidence | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|
| 15-29 | 0.000 | - | 0.046 | - | - | 0.045 | - | - | 0.043 | - |
| 30-44 | 0.000 | 0.065 | 0.063 | - | 0.179 | 0.117 | - | - | 0.055 | 0.054 |
| 45-59 | 0.000 | 0.001 | 0.367 | 0.179 | 0.436 | - | 0.083 | 0.728 | 0.079 | 0.386 |
| 60-69 | - | 0.002 | - | 1.239 | 0.940 | 2.232 | - | 1.019 | 1.364 | 1.107 |
| 70-79 | 0.005 | 3.521 | - | - | 2.615 | - | - | 0.002 | 1.412 | 2.660 |
| > 80 | 3.130 | 0.006 | - | 4.819 | 2.326 | 1.124 | 0.002 | 5.371 | 6.309 | - |
Source: Author’s own research, based on information obtained from the RIPS, centralized by the Ministry of Health and Social Protection.
We calculated the number of years of life lost due to premature death caused by GC and found that men had a higher frequency of years lost compared to women (Figure 1).
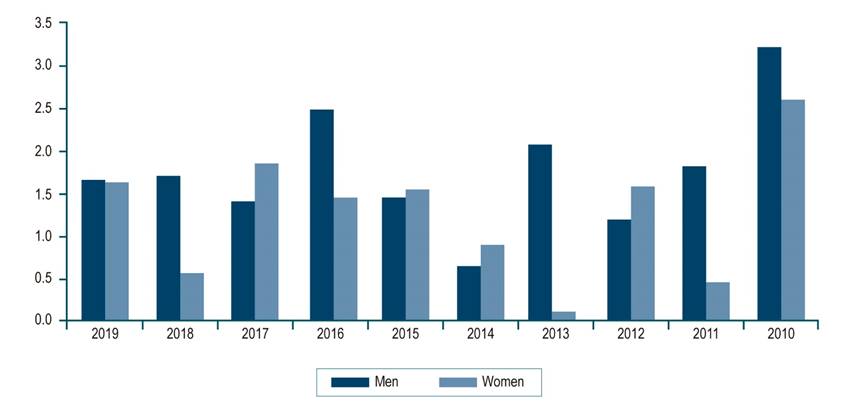
Figure 1 Years of life lost due to premature death secondary to GC according to sex in Tunja between 2010 and 2019 (per 1000 inhabitants). Source: Author’s own research.
Using the average reported disease survival rates for Colombia, the total DALYs were calculated by considering cases from each age group.10 Over the 2010-2019 period, the population of Tunja lost 34.2 DALYs per 1000 individuals as a result of GC, with a rate of 1.7/1000 inhabitants. Disability losses accounted for 10.9% of DALYs. The age group with the highest DALYs was 45-59 years, contributing to 34% of the total, followed by the 60-69 age group with 27.4% (Table 4).
Table 4 Distribution of YLL, YLD, and DALY by GC in Tunja, according to year (rates per 1000 inhabitants)
| Year | YLL | YLD | DALY | |||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| 2019 | 1.7 | 1.64 | 0.3 | -0.01 | 2.0 | 1.6 |
| 2018 | 1.7 | 0.59 | 0.3 | 0.42 | 2.0 | 1.0 |
| 2017 | 1.4 | 1.86 | -0.1 | 0.11 | 1.3 | 2.0 |
| 2016 | 2.5 | 1.46 | 0.3 | -0.16 | 2.8 | 1.3 |
| 2015 | 1.5 | 1.56 | 0.2 | 0.28 | 1.7 | 1.8 |
| 2014 | 0.6 | 0.91 | 0.2 | 0.03 | 0.9 | 0.9 |
| 2013 | 2.1 | 0.13 | -0.1 | -0.06 | 1.9 | 0.1 |
| 2012 | 1.2 | 1.60 | 0.5 | 0.36 | 1.7 | 2.0 |
| 2011 | 1.8 | 0.45 | 0.2 | 0.22 | 2.1 | 0.7 |
| 2010 | 3.2 | 2.61 | 0.6 | 0.10 | 3.8 | 2.7 |
| Total | 17.7 | 12.8 | 2.4 | 1.3 | 20.1 | 14.1 |
Source: Author’s own research.
Discussion
GC is a significant contributor to morbidity and mortality rates in many parts of the world, with Asia and Central and South America experiencing the highest incidence and mortality rates. It is projected that there will be an 80% increase in its epidemiological behavior worldwide by 2030.1,26 In Colombia, it was the leading cause of death from neoplasms in 20202 and the third most common cancer in terms of incidence.27 Despite this, screening and early detection plans have been limited, particularly when compared to other prioritized cancers like cervical, breast, or prostate cancer. Moreover, screening plans have been further restricted due to the global impact of the severe acute respiratory syndrome coronavirus pandemic type 2 (SARS-CoV-2).28 Therefore, this study aims to describe the burden of GC disease in Tunja over a decade based on official records, contributing to similar studies with comparable characteristics, as it is a high-land Colombian city with risk factors16,29 typical of other municipalities with high or comparable mortality rates from GC.
Neoplasms are ranked as the second-highest cause of disease burden worldwide,30 with variations in prevalence depending on geographic location. For example, in Korea, the estimated DALY for GC between 2000-2020 was 445/100,000,24 while in nearby Mexico, it was 80/100,000 for men and 85.7/100,000 for women31 from 2010 to 2014. In Colombia, the DALY was 172.7/100,000 in 20174 and 131.5/100,000 in 2006 in Santander.32 In our study, the rate was found to be 170/100,000 inhabitants, which is consistent with the last reported figures in the country.4 Sierra et al.26 have also reported Colombia and South America as areas with high incidence and mortality due to GC worldwide, and our results validate the burden of secondary disability caused by GC in our region.
The authors of this study originally hypothesized a higher DALY due to GC in Tunja, Boyacá; however, the results showed 34.2 years of life lost during the studied decade, with a predominance of age between 45 and 59 years and a life expectancy of 82.4 years according to WHO and 77 years according to DANE.33 This is noteworthy since- even though 89.1% of DALY was due to YLL (data consistent with the literature worldwide)-33,34) the population described in this study is younger and predominantly female, which differs from that reported in other research at departmental,35 national,4 and global36 levels, and may correspond to an information bias due to the data obtained from official secondary sources (SISPRO), which depend on satisfactory completion or diagnosis by the physician according to ICD-10. Nonetheless, despite the possible under-registration of SISPRO, this study found a higher prevalence of GC than predicted by the Global Cancer Observatory (GLOBOCAN) in 2020 for Colombia, with 22.82 cases per 100,000 inhabitants.27
These results offer valuable quantitative evidence that can be utilized to establish, prioritize, and assess public policies aimed at preventing and diagnosing gastric tumors at an early stage. Therefore, we recommend that the methods used in cities with long-term population registries, such as Bucaramanga and Cali, be employed in the department of Boyacá and Tunja to estimate and carry out continuous and descriptive evaluations of the affected population.
Conclusions
Tunja exhibited incidences akin to those reported by Triana JJ et al., Amaya Lara et al., Arias Sosa et al., and Caicedo A et al. Nevertheless, the disease burden detected in this study was primarily attributed to years of life lost due to premature death (89.1%). This underscores the pressing need to focus on screening, early diagnosis, periodic follow-up, early initiation of treatment, and population registry creation to enhance patient prognosis.











 texto em
texto em 



