Introduction
Portal hypertensive biliopathy is a condition that encompasses structural and functional anomalies of the biliary tract (intra- and extrahepatic), gallbladder, and cystic duct in patients with portal hypertension.1 Bile duct changes are commonly observed in extrahepatic portal vein obstruction (EHPVO) due to normal bile duct compression by cavernous portal vein transformation.2 Several terms have been used to describe this condition, such as portal biliopathy, portal cavernoma-associated cholangiopathy, or cholangiopathy associated with portal hypertension. However, the most widely accepted term is currently portal hypertensive biliopathy.1 The bile duct involvement results from external compression from the enlarged venous plexuses that form in an attempt to decompress the portal vein obstruction caused by thrombosis.3 The first cases linking EHPVO and cholestasis were reported in the 1950s,4 and even today, the prevalence of this condition is not well established as its symptoms are rare (5%-15%).5
Clinical case
A 48-year-old man with a history of portal thrombosis and cavernous degeneration of the portal and portal hypertension presented to the emergency department after experiencing one week of jaundice, choluria, and generalized pruritus linked to asthenia and adynamia. The patient’s medical history included portal thrombosis with cavernous degeneration and secondary portal hypertension for one year without primary or secondary thrombophilia, and a previous variceal gastrointestinal hemorrhage treated with ligation. On admission, the patient was in regular general condition with normal vital signs and no alteration of consciousness. Physical examination revealed generalized jaundice skin and a protruding abdomen due to an abundant adipose panicle without abdominal pain or visceromegaly. Laboratory tests performed on admission (Table 1) showed hyperbilirubinemia, primarily from direct bilirubin, as well as elevated transaminases and cholestasis tests.
Table 1 Laboratory tests during hospitalization in the HPTU
| Study | Income | Control |
|---|---|---|
| Hemoglobin | 15.4 g/dL | 13.2 g/dL |
| Hematocrit | 45% | 41% |
| Leukocytes | 7400/mm3 | 5410/mm3 |
| Platelets | 147 000/mm3 | 144 000/mm3 |
| Creatinine | 1.09 g/dL | 1.02 g/dL |
| Urea nitrogen | 9 mg/dL | |
| AST | 177 U/L | 29 U/L |
| ALT | 325 U/L | 34 U/L |
| Total bilirubin | 6.54 mg/dL | 1.07 mg/dL |
| Direct bilirubin | 3.72 mg/dL | 0.57 mg/dL |
| Alkaline phosphatase | 406 U/L | 128 U/L |
| GGT | 403 U/L | 67 U/L |
| Chlorine | 103 mmol/L | |
| Potassium | 4.19 mmol/L | |
| Sodium | 135 mmol/L | |
| Calcium | 9.4 mg/dL | |
| Albumin | 4.3 g/dL | |
| INR | 1.1 | |
| CRP | 2.64 mg/dL | |
| Hepatitis C antibodies | Non-reactive | |
| Surface antigen for hepatitis B | Non-reactive | |
| IgM antibodies for hepatitis A | Non-reactive | |
| Tumor markers | Negative |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; GGT: gamma-glutamyl transferase; IgM: immunoglobulin M; INR: international normalized index; CRP: C-reactive protein. Source: Authors’ own research.
Due to cholestatic hepatitis syndrome and a history of chronic portal thrombosis, the patient underwent a contrast-enhanced computerized axial tomography (CT) scan of the abdomen. The results showed signs of chronic liver disease with chronic portal thrombosis, cavernous transformation, multiple venous collaterals, and splenomegaly (Figure 1). In addition, the scan revealed central bile duct dilation with a normal diameter common bile duct, which was further characterized by a magnetic resonance cholangiopancreatography (MRCP). The MRCP revealed an acute thrombosis of one of the collaterals in the hepatic hilum, causing central dilation and an excess of soft tissue with a nodular appearance restricting diffusion. These findings produced a mass effect in the distal common bile duct and were interpreted as a tumor-like cavernoma (Figure 2).
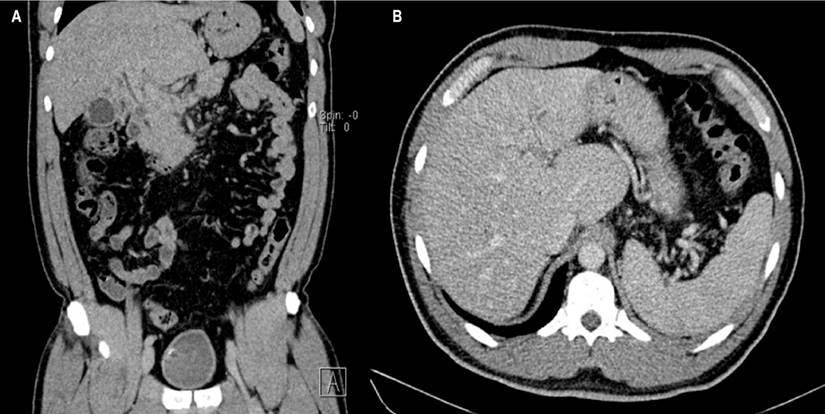
Figure 1 A. CT scan of the abdomen contrasted with findings of chronic liver disease and multiple venous collaterals. B. Findings of liver disease (nodularity of liver lobes) and splenomegaly. Source: Authors’ archive.
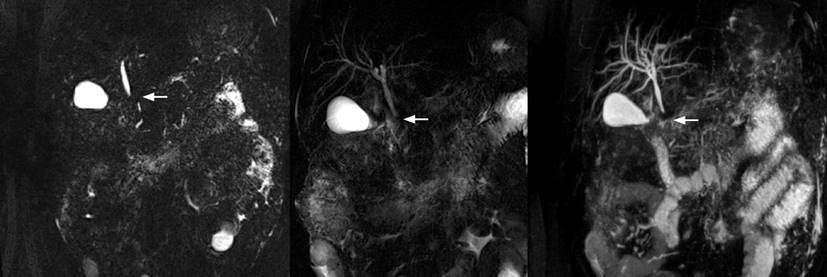
Figure 2 Stenosis in the distal common bile duct, with extrinsic compression image. Source: Source: Authors’ archive.
Subsequently, an endoscopic retrograde cholangiopancreatography (ERCP) was performed to bypass the bile duct and initiate enoxaparin anticoagulation at a dose of 1 mg/kg every twelve hours to resolve the acute thrombosis. During ERCP, stenosis was observed in the distal common bile duct of extrinsic appearance, while the proximal and middle bile ducts measured 6 mm in normal diameter. To treat this condition, a limited sphincterotomy and placement of a plastic stent measuring 10 French (Fr) x 7 centimeters (cm) were performed, resulting in abundant dark bile drainage (Figure 3). The patient had a good clinical evolution and did not present any complications after the procedure. Therefore, he was discharged with analgesic management, anticoagulation with low molecular weight heparins (LMWH), and ursodeoxycholic acid (UDCA).
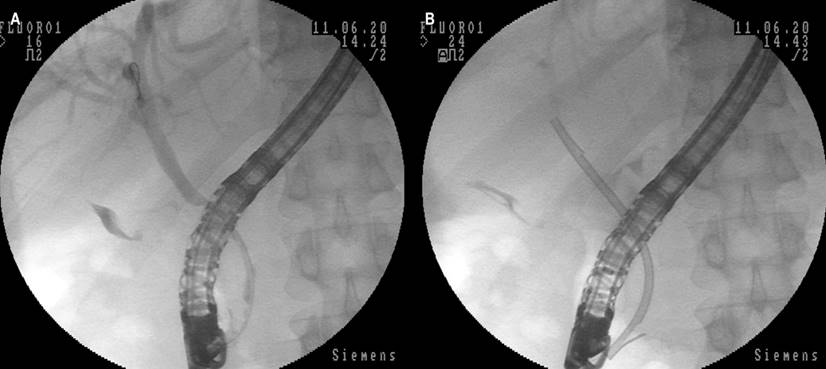
Figure 3 Images of ERCP. A. Decrease in diameter of the distal common bile duct with an appearance that impresses by extrinsic compression. B. Placement of plastic biliary stent, with evident elimination of the contrast medium of the bile duct. Source: Authors’ archive.
One month after being discharged from the hospital, the patient attended an outpatient hepatology follow-up appointment. He reported no signs of jaundice, choluria, or acholia but mentioned occasional mild abdominal pain. The physical examination was unremarkable, except for palpable splenomegaly, 4 cm from the left rib cage. His paraclinical tests were within normal limits.
Discussion
In the 1990s, it was discovered that between 80% and 100% of patients with extrahepatic portal vein obstruction (EHPVO) have concomitant portal hypertensive biliopathy (PHB), although most of them are asymptomatic.6,7 This condition is more common in patients with EHPVO secondary to liver cirrhosis or idiopathic portal hypertension.1 In terms of local epidemiology, Suárez et al. reported the first experience of a Colombian center in managing and treating PHB cases.3
PHB is closely related to the etiology of portal hypertension, which includes conditions such as liver cirrhosis, neoplasms, coagulopathies, myeloproliferative disorders, or congenital liver fibrosis.8) Although the pathogenesis of PHB is not entirely clear, it is well established that the venous plexuses of the bile ducts and gallbladder have a crucial role in the development of biliary obstruction.7
Portal hypertension slows portal blood flow, increasing the risk of portal vein thrombosis, which in turn causes the derivation of blood flow through portosystemic collaterals.8) These collateral veins develop a dense vascular pattern and fibrous stroma in the peripancreatic region along the occluded portal vein, forming a portal cavernoma that provides an alternative route for blood flow around the thrombosed segment of the portal vein.9
The initial description of biliary changes observed in patients with portal cavernoma was performed in ERCP, mostly in individuals with biliary manifestations.10 These descriptions were replicated and expanded with the increased use of MRCP.11 This was a fundamental change in the diagnosis of the condition since the latter is more reproducible and has fewer risks concerning ERCP. Abnormal findings include extrahepatic stenosis, intrahepatic biliary dilation, caliber irregularity, ductal ectasia, clefts, displacement, and ductal angulations.12 Currently, there is a standardized nomenclature proposed by the working group of the Indian Association for the Study of the Liver (INASL) (Table 2).10-12 The case described corresponds to extrinsic compressions/indentations (Figure 3), which were successfully resolved by ERCP and biliary stenting.
Table 2 Biliary findings corresponding to portal cavernoma-associated cholangiopathy
| Imaging findings | Description/concept |
|---|---|
| Extrinsic compressions/indentations | Smooth impressions with the nodular outline. The indentation is more than a quarter of the width of the bile duct. Impressions can be multiple. |
| Superficial impressions | Smooth, noncontiguous impressions in the bile duct, less than a quarter the diameter of the bile duct |
| Irregular ductal contour | Fine, irregular, and wavy contour of bile duct walls due to contiguous superficial clefts, less than a quarter the diameter of the duct |
| Stenosis | Decrease in the ductal lumen, referring to a “downstream” segment of the duct. Narrow bile duct segments should offer some resistance to the extraction balloon and should produce a waistline. Stenoses can be divided into mild, moderate, or severe depending on whether the stenotic segment is > or < two-thirds the diameter of the adjacent normal segment. |
| "Upstream" dilation | Proximal dilation can be similarly classified as “mild to moderate” or “severe”, depending on whether the dilated segment is between 1.5-2 and > 2 in diameter of the adjacent normal duct, respectively. |
| Bile duct angulation | An angle of < 145° between the proximal and distal bile duct is proposed. |
| Ductal ectasia | It is the dilated segment of the biliary tree without any obvious obstruction “downstream”. |
Modified from reference10.
The initial identification of biliary changes in patients with portal cavernoma was conducted through endoscopic retrograde cholangiopancreatography (ERCP), primarily in individuals with biliary manifestations.10 Subsequent observations of these changes were carried out through the increased utilization of magnetic resonance cholangiopancreatography (MRCP).11 The use of MRCP represented a significant improvement in diagnosing this condition due to its greater reproducibility and reduced risks compared to ERCP. The biliary changes associated with portal cavernoma include extrahepatic stenosis, intrahepatic biliary dilation, caliber irregularity, ductal ectasia, clefts, displacement, and ductal angulations.12 Currently, a standardized nomenclature has been proposed by the Indian Association for the Study of the Liver (INASL) working group (Table 2).10-12 The present case corresponds to extrinsic compressions/indentations (Figure 3), which were successfully resolved through ERCP and biliary stenting.
The treatment strategy for symptomatic portal cavernoma depends on the mechanism that generates the symptoms, such as stones, stenosis, or both.12 Biliary clearance/drainage and portosystemic shunt are the two main options available. The endoscopic approach includes sphincterotomy with gallstone removal (when present), dilation of stenosis with or without stent insertion, and biliary drainage. However, the treatment of biliary obstruction by portal cavernoma remains controversial due to the rarity of the condition. For Dumortier et al., the first step in managing biliary obstruction is through endoscopic management by ERCP, which effectively confirms the diagnosis and evaluates common bile duct patency.13 Inserting a stent after sphincterotomy and gallstone removal allows the drainage of the bile duct and prevents the risk of early infectious complications.13-15 Sphincterotomy alone is likely insufficient, based on the data observed by Perlemuter et al.,16 in which recurrent cholangitis and death associated with cholangitis occurred in two of three cases in this series. Exclusively endoscopic management could avoid surgical procedures with hemorrhagic potential. Portosystemic shunt is generally proposed to treat hemorrhagic complications associated with portal hypertension.17
Conclusion
Portal hypertensive biliopathy is a rare condition that should be considered in patients with a history of portal hypertension who present with jaundice. The imaging patterns of this condition vary depending on the extent and location of the affected venous territory. Magnetic resonance cholangiopancreatography and ERCP with sphincterotomy and stenting are the current diagnostic methods of choice, and they may also serve as the preferred therapeutic approach in symptomatic patients.











 text in
text in 



