Introduction
Behcet’s disease (BD), first described by Hulusi Behçet in 1937,1 is a chronic inflammatory disease of unknown origin that affects multiple systems and primarily involves blood vessels of different calibers.2 The disease is more common in countries located along the ancient Silk Road, in the Mediterranean region, and in the Middle and Far East, particularly in Turkey, Saudi Arabia, Iraq, Israel, China, and Japan, with a prevalence range of 7.2 to 420 cases per 100,000 inhabitants.3
According to the International Chapel Hill Consensus Conference, BD is classified as a vasculitis of variable vessels with an unknown etiology.4 However, immunological mechanisms have been identified in its pathogenesis, which are linked to an increase in the activation of peripheral blood γ/δ T lymphocytes, the rise of Th1 cytokines, including interleukin (IL)-12, IL-18, interferon-gamma (IFN-γ), the presence of autoantibodies, circulating immune complexes, hypercoagulability, and activation of the vascular endothelium. Additionally, genetic mechanisms are involved through the presence of HLA-B*51 molecules and alterations in the aminopeptidase 1 enzyme of the endoplasmic reticulum and the receptors of IL-23 and IL-10.5-7
Behcet’s disease presents with a variable clinical phenotype, with the most common phenotypes being mucocutaneous, with aphthous lesions on the skin, in the oral and genital mucosa (60%-90%), ocular in the form of panuveitis (45%-90%), and musculoskeletal expressed as mono- or oligoarthritis of large joints (11.6%-93%).8 Gastrointestinal involvement occurs less frequently (8%-34%), with diverse clinical manifestations ranging from nonspecific symptoms such as abdominal pain, nausea, diarrhea, and digestive tract bleeding to complications such as ulcers, perforation, fistulas, abscesses, and intestinal ischemia.9
We present a case report of a 28-year-old woman with a history of BD who experienced gastrointestinal tract hemorrhage due to ulcerated vascular lesions in the intestinal mucosa. This case is particularly interesting because BD is less common in the Western hemisphere and typically involves a lower proportion of gastrointestinal manifestations.
Clinical case
A 28-year-old woman presented to the emergency department with a 48-hour history of four episodes of melenic stools, nausea, and mild diffuse abdominal pain. She also had ulcers in her oral mucosa for the past 15 days. The patient had a relevant medical history of Behcet’s disease (2013), with secondary intestinal obstruction and perforation, and underwent two intestinal segment resections with colostomy and ileostomy at 13 and 19 years of age. She was treated for four years with azathioprine and colchicine, which were discontinued a year ago due to the resolution of symptoms. The patient had no other significant medical history. Paraclinical data is included in Table 1.
Table 1 Results of admission laboratory tests
| Laboratories | Result | Reference values |
|---|---|---|
| Blood picture | ||
| - Leukocytes | 8,5 x 10^3/μL | 4,5-10 x 10^3/μL |
| - Red blood cell count | 3,8 x 10^6/μL | 4,2-5,4 x 10^6/μL |
| - Hemoglobin | 11,2 g/dL | 12,5-16 g/dL |
| - Hematocrit | 31,9% | 37-47% |
| - Mean corpuscular volume | 83,2 fL | 79-101 fL |
| - Mean corpuscular hemoglobin | 29,1 pg | 29-35 pg |
| - EDR | 13,2% | 11%-16% |
| - Platelets | 281,8 x 10^3/μL | 150 -450 x 10^3/μL |
| Electrolytes | ||
| - Potassium | 3,4 mmol/L | 3,5-5,1 mmol/L |
| - Sodium | 137 mmol/L | 136-146 mmol/L |
| - Chlorine | 105 mmol/dL | 101-109 mmol/L |
| - Magnesium | 2,0 mg/dL | 1,9-2,5 mg/dL |
| Renal function | ||
| - Creatinine | 0,89 mg/dL | 0,55-1,02 mg/dL |
| - Urea nitrogen | 18,6 mg/dL | 7-25 mg/dL |
| Liver function | ||
| - AST | 26 U/L | 0-35 U/L |
| - ALT | 21 U/L | 0-35 U/L |
| Acute phase reactants | ||
| - CRP | 0,16 mg/dL | 0-0,5 mg/dL |
| - ESR | 21 mm/h | 0-20 mm/h |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP: C-reactive protein; EDR: erythrocyte distribution range; ESR: erythrocyte sedimentation rate. Source: Authors’ own research.
The patient underwent an esophagogastroduodenoscopy which showed erythematous antral gastropathy, and a total colonoscopy revealed the presence of a 10 mm ulcer with regular edges and fibrin at 3 cm from the colon anastomosis, a 12 mm ulcer with regular edges and fibrin at 5 cm proximal, and two ulcers of 4 and 7 mm in size with characteristics similar to the proximal 10 cm, for which biopsies of the center and the edge were performed. Additionally, a few aphthoid lesions were observed in the distal ileum, which is indicative of ulcerated ileitis with normal colon anastomosis (Figure 1). The biopsy of ileal mucosal fragments did not accurately represent the ulcers. However, it showed marked edema of the lamina propria, angiectasias associated with mononuclear and polymorphonuclear infiltrate that focally erode the superficial epithelium, and fragments with fibrinoleukocyte material, which suggested nonspecific inflammatory changes (Figure 2).
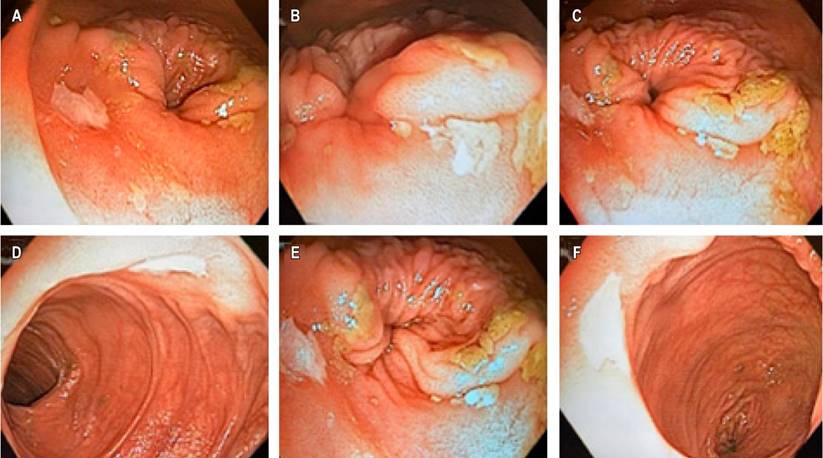
Figure 1 Total colonoscopy with findings of ulcerated ileitis. A-F. Well-defined ulcers with regular and slightly erythematous edges, with a fibrin background of the dimensions described in the clinical case. Source: Authors’ archive.
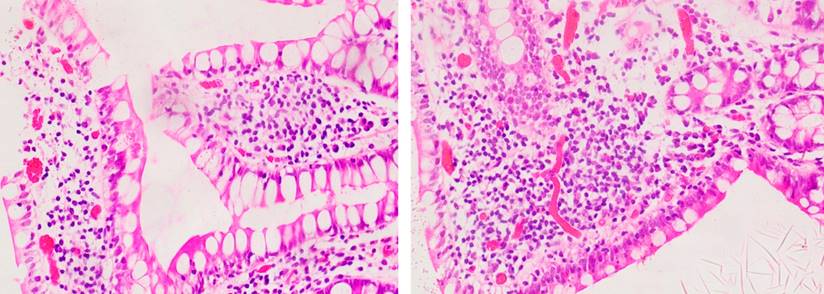
Figure 2 Histopathological findings of ulcer samples in the distal ileum. Findings of edema of the lamina propria and angiectasias associated with mononuclear and polymorphonuclear infiltrate eroding the distal epithelium. Courtesy of Edna Margarita Martínez Ortiz, Pathologist.
After the endoscopic studies, the patient was started on immunomodulatory treatment with azathioprine 50 mg orally (PO) every eight hours and prednisolone 1 mg/kg/day PO (60 mg/day). Nine months after hospital discharge, the patient had a satisfactory clinical course.
Discussion
The clinical case presents a patient with Behçet’s disease (BD) and gastrointestinal manifestations secondary to ulcerated ileitis. This information is particularly relevant in the medical field due to the limited published literature and the low incidence of the disease in Latin America, including Colombia,10,11 where only 523 cases of BD were identified and registered in the Comprehensive Information System for Social Protection (SISPRO) of the Ministry of Health and Social Protection from 2012 to 2016, resulting in a prevalence of 1.1 cases per 100,000 inhabitants. The disease is more prevalent among women aged 45-49 years and in the regions of Antioquia, Cundinamarca, and Bolívar.11 The patient’s clinical case is consistent with the findings of the aforementioned study, as she is a female patient from one of the regions with the highest reported cases of BD during a specific period from 2012 to 2016.
In countries where BD is prevalent, the clinical manifestations of the disease have been well characterized. For instance, in Egypt, a study on 223 patients found that mucocutaneous (84.5%) and musculoskeletal (15.9%)12 symptoms were the most common clinical phenotypes. Similarly, a study on 489 patients in China identified mucocutaneous lesions as the most frequent manifestation, while gastrointestinal ulcers were more common in patients over 40. (13 In contrast, the patient in this clinical case experienced recurrent gastrointestinal tract lesions since adolescence, which was the predominant clinical manifestation.
Furthermore, a study conducted in Colombia on 20 patients diagnosed with BD, with an average age of 40.6 ± 8.2 years, documented that the most common clinical presentations were recurrent oral ulcers (95%), genital ulcers (75%), and skin infections (60%), with 40% of patients presenting gastrointestinal manifestations.14 Based on the gastrointestinal involvement described in the clinical case and the previously reported higher proportion of gastrointestinal manifestations in Colombian patients, it is suggested that further research be conducted to clinically and epidemiologically characterize BD cases in the country and evaluate the frequency of complications related to gastrointestinal involvement.
In regard to the subject, the involvement of the gastrointestinal tract in BD can vary based on its location. Esophageal involvement is rare and is typically demonstrated through ulcers, stenosis, and perforation. Ulcers in the stomach and duodenum may occur. However, complications such as perforation, gastrointestinal bleeding, fistulas, stenosis, and abscesses are more frequent in the jejunum, ileum, and colon.
In patients with BD, the terminal ileum and ileocecal region are commonly affected portions of the intestine.15-17 Moreover, intestinal lymphangiectasias leading to protein-losing enteropathy have been reported.18 In this clinical case, the patient experienced digestive tract hemorrhage resulting from ulcerated ileitis and a history of previous intestinal perforations that required surgery. This supports existing evidence indicating that digestive tract involvement is associated with a more severe clinical presentation and greater morbidity in patients with BD.
There are no pathognomonic symptoms or specific biomarkers for diagnosing BD, which is why various classification systems are utilized. The most commonly used system is the international criteria for BD, proposed by the international BD study group, which includes eye lesions, oral and genital ulcers, skin lesions, neurological and vascular manifestations, and a positive pathergy test (appearance of papules or pustules in epidermal areas that have had microtraumas).19,20 In this clinical case, the patient was diagnosed with BD in 2013, with a predominance of oral ulcers according to the diagnostic criteria and a predominance of gastrointestinal manifestations. Therefore, given that BD is a multisystemic condition, in the presence of a patient with recurrent ulcerated lesions and gastrointestinal manifestations, it is important to prioritize endoscopic studies to assess vascular lesions caused by this disease.
The patient’s endoscopic findings were consistent with ulcerated ileitis, making distinguishing between BD and Crohn’s disease difficult. To differentiate between the two, endoscopic criteria have been proposed, such as the presence of limited ulcers with a round or oval shape, focal distribution (single or multiple), absence of aphthous lesions, or a paved appearance, which are compatible with BD.21 In this case, the oval ulcerated lesions with regular edges focused on the distal ileum found in the patient are representative of BD.
The histopathological features of BD in the gastrointestinal tract include mononuclear infiltrates and perivascular mast cells, neutrophilic vasculitis, and acute and chronic inflammatory changes in the submucosa.15 Despite the absence of clear evidence of ulcers in the histopathological report of the biopsies obtained during endoscopy, the edema of the lamina propria, along with mononuclear and polymorphonuclear infiltrates, may suggest the inflammatory changes that BD triggers in the gastrointestinal tract.
The pharmacological treatment of gastrointestinal involvement in BD varies depending on the severity of the clinical presentation. For mild cases, monotherapy with 5-aminosalicylate derivatives is recommended. In cases of moderate to severe severity, systemic corticosteroids are the first line of treatment. However, due to the side effects associated with high doses of corticosteroids, azathioprine has recently become relevant in managing such cases. In patients with severe gastrointestinal manifestations that do not respond to azathioprine, tumor necrosis factor inhibitors (infliximab or adalimumab) are preferred as third-line management.22,23
In this particular case, the patient had moderate-severe gastrointestinal involvement, as evidenced by the recurrence of her clinical profile and previous history of intestinal obstruction and perforation. As a result, treatment with corticosteroids and azathioprine was resumed, which resulted in an adequate clinical response.
Conclusions
BD is a rare condition in the Colombian population, and as it affects multiple systems, an interdisciplinary assessment is necessary to evaluate the involvement of various organs. Additionally, endoscopic studies are crucial for the early identification of vascular lesions that can lead to severe complications such as obstruction, perforation, and gastrointestinal bleeding. Timely initiation of immunomodulatory therapy can prevent such complications.
Additionally, BD should be considered among the differential diagnoses of inflammatory bowel diseases, considering the established diagnostic criteria and the differentiation of endoscopic findings inherent to this pathology.
This clinical case report serves as a starting point for future research in Colombia. Further studies should focus on the clinical and epidemiological characterization of BD cases, the determination of its incidence and prevalence in the Colombian population, and the identification of associated factors.











 text in
text in 



