Introduction
Paraduodenal hernia (PH) is an alteration that is part of congenital hernias. It is a rare condition, usually diagnosed during surgery.1
There are multiple types of congenital internal hernias. In order of frequency of appearance, there are the PH, pericecal, foramen Winslow, transmesenteric, perivesical, and omental hernias.1 Internal hernias cause 1% of intestinal obstructions; within these, PH contributes 53%. It is more frequent in men than women, with an incidence of 3 to 1.
Despite its congenital nature, the complications that lead to its diagnosis occur between the third and fourth decades of life.2 The risk of developing intestinal obstruction or perforation is 50% over a lifetime, with a mortality of 20% to 50%.3-5 PH can be left-sided (75%) or right-sided (25%) and occur due to alterations in bowel rotation or poor fusion of mesenteric folds during embryogenesis.1,3
Presentation of the case
This is a 29-year-old male patient with no medical or surgical history. He was admitted to the emergency department due to a 24-hour clinical profile of abdominal pain of sudden onset, colic type, located in the mesogastrium and left flank, accompanied by abdominal distension and emesis, radiating to the left paravertebral region and the left iliac fossa. Physical examination documented sinus tachycardia, distended abdomen, and pronounced deep palpation pain in the left hemiabdomen, with no signs of peritoneal irritation. Paraclinical studies showed leukocytosis (15,000 cells/μL), neutrophilia (12,750 cells/μL), and elevated C-reactive protein (16 mg/dL). Initially, it was suspected to be urolithiasis with obstructive effect. The patient underwent a simple computerized tomography urogram (uroCT), which showed a conglomerate of intestinal loops located towards the left hemiabdomen with diffuse intestinal edema and scarce fluid between the loops (Figure 1).

Figure 1 UroCT shows an axial and coronal section, respectively. The arrows point to the conglomerate of intestinal loops in the left hemiabdomen. Source: Authors’ archive.
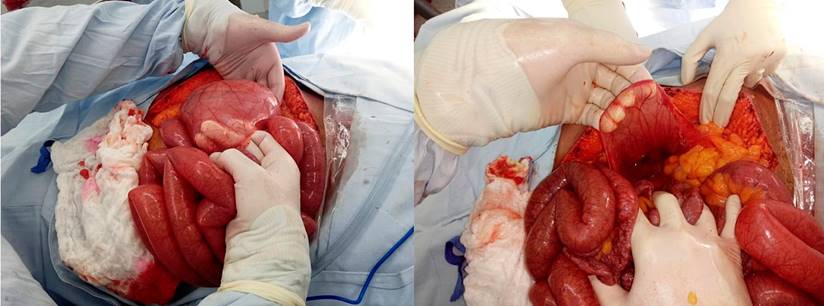
They requested an assessment by our general surgery group. At the time of assessment, we found signs of peritoneal irritation in the patient, so he was scheduled immediately for surgery. Initially, he underwent a laparoscopic approach that showed great distension of the intestinal loops, so we decided to convert to open surgery, and we performed a median supra- and infraumbilical laparotomy. When we explored the abdominal cavity, we detected a left PH containing 2 meters of proximal small intestine within the hernial sac, proximal dilation to the site of obstruction, and the hiatus of entry to the sac with ischemia of the entire segment of the involved intestine. We proceeded to section the peritoneal fibrotic tissue capsule and reduced the content, restoring arterial flow and recovering the involved segment’s viability. Subsequently, the capsule and the hernial sac were resected entirely. Finally, we verified that there was no hiatus in the abdominal cavity to avoid the risk of recurrence (Figures 2, 3, and 4). The patient evolved without eventualities and was discharged on the fourth postoperative day.

Figure 2 Laparotomy shows the hernial sac created by the retroperitoneal peritoneum of the Landzert fossa. Source: Authors’ archive.

Figure 3 Surgeon’s finger passes through the hiatus of the Landzert fossa, where intestinal loops come out. Source: Authors’ archive.
Discussion
Embryologically, the intestine has been divided into foregut, midgut, and hindgut. PH occurs when there is an alteration in any part of the midgut formation, defined as all intestinal portions irrigated by the superior mesenteric artery (SMA), including the distal duodenum, jejunum, ileum, ascending colon, and proximal transverse colon.3 Consequently, the embryonic development of the midgut is divided into two portions: prearterial and postarterial. The prearterial portion extends from the distal duodenum to the omphalomesenteric duct, while the postarterial portion begins distal to the omphalomesenteric duct to the proximal transverse colon. During the fifth week of gestation, the midgut is carried into the yolk sac, then rotates 90° counterclockwise on the axis of the SMA and returns to the abdominal cavity in the tenth week of gestation. At that time, said cavity is large enough to house this intestinal segment. The prearterial portion is on the right of the SMA, and the post-arterial portion is on the left. It presents a second rotation of 180° counterclockwise for a total of 270° and, finally, reaches its anatomical position. If this does not happen, a phenomenon of poor intestinal turnover occurs.6
PH occurs when there is some failure in the rotation of the prearterial portion of the small intestine when interposing in the fusion of the colon (postarterial) with the retroperitoneum, which creates the fosses where the hernia occurs: the Landzert fossa to the left of the SMA, with 75% frequency, and the Waldeyer fossa on the right side, with a 25% frequency.3,7,8
Concerning the clinical presentation, symptoms begin between the third and fourth decades of life (38.5 years of age on average).9 50% of patients present mild cramping abdominal pain, chronic, mainly postprandial, and exacerbated by Valsalva maneuvers with periods of complete remission. It can produce recurrent episodes of nausea, vomiting, chronic malabsorption, and weight loss. These symptoms usually change in characteristics or improve with changes in position. Patients present mild manifestations such as dyspepsia when the hernia is small and shrinks spontaneously. The other 50% of cases present acute abdomen due to sudden intestinal obstruction that can produce massive ischemia of the small intestine, especially when more than 40% of the intestine is involved.1,3-5
Physical examination showed no typical clinical signs: less than 20% of patients have a left upper quadrant mass with pain that varies according to the degree of incarceration and intestinal ischemia. In the reported case, the clinical presentation was complete intestinal obstruction with no prior symptoms.
Many PH cases are diagnosed incidentally on imaging, laparotomy, or autopsy.2,5,9 Simple radiographic studies are not very specific, showing signs of intestinal obstruction with a conglomeration of intestinal loops towards the left side of the upper abdomen.3 Contrasting studies such as tomography document a mass of regular, smooth edges with loops of small intestine encapsulated in the upper hemiabdomen, described as Donnelly’s border. Additionally, anomalies can be seen in the mesenteric vessels consisting of their congestion, crowding, twisting, and stretching.4,5,10
If the PH is left-sided, we can observe a group of intestinal loops delimited by the pancreas, stomach, and ascending portion of the duodenum, to the left of the ligament of Treitz, behind the pancreatic tail, which displaces the inferior mesenteric vein to the left or between the transverse colon and the left adrenal gland. When the PH is right-sided, the accumulation of loops is located inferolateral to the descending portion of the duodenum, and we can observe an afferent loop of the jejunum and an efferent loop of the jejunum or ileus through the entrance hole of the Waldeyer’s fossa.3,5 The sensitivity and specificity of tomography are approximately 63% and 76%, respectively.11 Diagnostic laparoscopy can be very useful in cases where the diagnosis cannot be verified with images.2
The treatment of these patients must comply with the fundamental principles of reducing the herniated intestine, verifying its viability, and repairing the hernial defect.9 Surgery is always indicated, even in asymptomatic patients with incidental diagnosis, since PH has a 50% risk of incarceration throughout life.6 Special care should be taken when opening the anterior sac since important vessels usually pass through it. In the case of a left-sided PH, it can pass the inferior mesenteric vein and the inferior mesenteric artery or the ascending branch of the left colic. In the case of a right-sided one, it can pass the middle colic artery with its right branch and the superior mesenteric vessels.3,8
In a left-sided PH, it is ideal to simply reduce the hernial contents and close the Landzert fossa with a non-absorbable suture. However, there are cases where it is impossible to perform it due to the pressure exerted by the intestines on the edge of the defect, so a herniotomy is necessary to release the intestine. At this point, the vascular care mentioned above is fundamental.3 In our case, manual reduction of the hernial contents was not possible, and it was necessary to perform an anterior herniotomy with ligation of the inferior mesenteric vein to avoid uncontrolled bleeding. In this way, the ischemic intestine could be released, and secondary transmural necrosis could be avoided. The laparoscopic approach is safe and effective when performed electively. However, we decided to perform an open technique due to the patient’s condition.
Conclusions
Congenital hernias are rare. Within this group, the PH is the most common; in turn, the left-sided PH is the one with the greatest frequency of appearance. Knowing this condition is essential to suspect it and be able to diagnose it. Depending on the patient’s condition, treatment is always surgical, either open or laparoscopic.











 text in
text in