Introduction
Elevation of liver injury markers in patients with coronavirus disease 2019 (COVID-19) is frequent. Elevated transaminases have been described in up to 14%-53% of patients1. Different studies describe elevated transaminases as a marker of inflammation and liver injury2,3 related to increased disease severity and worse clinical outcomes.
A pattern of predominantly cholestatic liver damage is recognized, given by the elevation of bilirubin and alkaline phosphatase4. This new clinical entity, called post-COVID-19 cholangiopathy4,5, is more frequent in critically ill patients6,7 and is characterized by a severe lesion of the biliary tract. Various pathophysiological mechanisms are proposed, such as microthrombosis at the level of the bile ducts, sclerosing cholangitis in critically ill patients, and direct injury caused by the virus. The frequency of this entity seems to be higher in patients with severe cases of COVID-196,7.
The number of reported cases of post-COVID-19 cholangiopathy is meager, and there are no reports in Latin America. This article describes the demographic, clinical, imaging characteristics, natural history, outcomes, and therapies used in eight cases of post-COVID-19 cholangiopathy managed at a university hospital in Colombia.
Materials and methods
This is a series of cases of patients diagnosed with post-COVID-19 cholangiopathy evaluated by the gastroenterology and hepatology services of Hospital Universitario San Ignacio in Bogotá, Colombia, between April 2020 and February 2022. We included adult patients who documented a cholestatic lesion with alkaline phosphatase levels above three times the standard value and abnormalities of the biliary tract on magnetic resonance cholangiography related to active or recent severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) infection (within six months), confirmed by positive laboratory results (positive polymerase chain reaction [PCR] or positive antigen), and who were examined in the outpatient clinic of the gastroenterology and hepatology services.
The patients’ demographic data were analyzed, including their pathological history, liver biochemistry, COVID-19 severity at initial hospitalization, imaging findings, complications, and treatment used. The information was collected systematically based on the data from institutional electronic medical records. The recorded liver biochemistry values are the peak levels documented during medical care.
Categorical variables are reported as absolute and relative frequencies, and continuous variables as median and interquartile range or mean and standard deviation, depending on the data distribution. The Shapiro-Wilk test was used to test the assumption of normality. The analysis was performed using the Stata 16 statistical package.
Results
Eight patients were included. Table 1 summarizes the demographic and biochemical data, complications, and treatments received during the initial hospitalization.
Table 1 Demographic, biochemical characteristics, and complications during the initial hospitalization of the included patients
| Variable | n = 8 |
|---|---|
| Age, years, mean (SD) | 56.5 (9.2) |
| Male sex, n (%) | 5 (62.5%) |
| Latin American ethnicity, n (%) | 8 (100%) |
| Comorbidities, n (%) | |
| High blood pressure | 2 (25%) |
| Type 2 diabetes | 3 (37.5%) |
| Obesity | 2 (25%) |
| Cardiovascular disease | 1 (12.5%) |
| Previous liver disease | 0 (0%) |
| Dyslipidemia | 2 (25%) |
| Blood biochemistry*, mean (SD) | |
| AST | 124.75 (68.4) |
| ALT | 114.75 (62.1) |
| Alkaline phosphatase | 1646.12 (611.3) |
| Total bilirubin | 13.77 (9.9) |
| Complications in initial hospitalization, n (%) | |
| Multiple organ failure | 0 (0%) |
| Superinfection | 8 (100%) |
| Thrombosis | 3 (42.8%) |
| Treatment used, n (%) | |
| Corticosteroids | 8 (100%) |
| Anticoagulation | 3 (37.5%) |
| Propofol | 8 (100%) |
| Ketamine | 4 (50%) |
| Norepinephrine | 8 (100%) |
*Documented peak levels during care. ALT: alanine aminotransferase; AST: aspartate aminotransferase; SD: standard deviation. Table prepared by the authors.
All patients were diagnosed with pneumonia during hospitalization, required stay in the intensive care unit (ICU) and mechanical ventilation. The average length of stay in the ICU was 40.3 days, and the average time of orotracheal intubation and invasive mechanical ventilation was 20.3 days. The patients received different sedoanalgesia protocols, explained by the stay in three other institutions and periods; four patients (50%) received sedoanalgesia with ketamine and 8 (100%) with propofol.
All patients had bacterial superinfection that required antibiotic management, and gram-negative bacteria, including Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa, caused all these infections. Three (37.5%) patients had thromboembolic events (two with pulmonary thromboembolism and one with deep vein thrombosis) requiring anticoagulation therapy.
The average time from documentation of SARS-CoV-2 infection to diagnosis of cholangiopathy was 133 days, with the shortest period being 85 and the longest being 256 days. All patients had alterations in the bile ducts, detected in endoscopic retrograde cholangiopancreatography (ERCP) results. Eight patients presented with dilatation of the intrahepatic bile duct, and seven had dilation of the extrahepatic bile duct. In four, there was evidence of a beaded appearance of the intrahepatic bile duct. Six (75%) patients had an extraction of unusual black material, and seven (87.5%) had recurrent episodes of cholangitis. Moreover, five patients had acute cholecystitis/choledocholithiasis preceded by the diagnosis of post-COVID-19 cholangiopathy.
Only one patient (12.5%) had a resolution of objective post-COVID-19 cholangiopathy findings, showed by a normal magnetic resonance cholangiography at follow-up. The remaining seven patients presented with worsening cholestasis and required multiple ERCPs for cholangitis management with stent replacement. Treatment with cholestyramine and ursodeoxycholic acid was indicated for three patients without improvement; they were referred to the liver transplant service due to the severity of their symptoms. Still, none had undergone transplantation at the time of the last follow-up. Six months after diagnosis, no patient had died, and three were in pre-hepatic transplant consultation.
Figure 1 shows one patient’s ERCP and magnetic resonance cholangiography. Figure 2 displays the extraction of the bile cast from another patient.
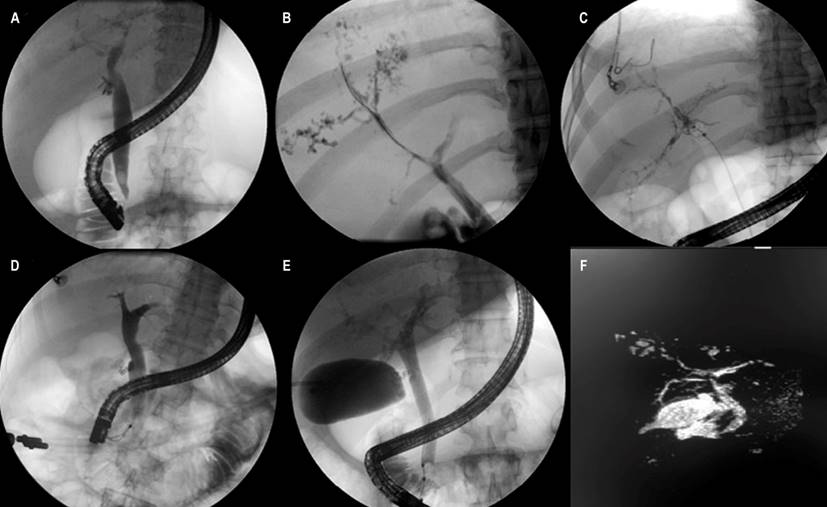
Figure 1 Imaging findings in post-COVID-19 cholangiopathy. A. Extrahepatic bile duct dilation on ERCP. B. Beaded bile duct of intrahepatic bile ducts on ERCP. C. Beaded bile duct in intrahepatic bile ducts on ERCP. D. Extrahepatic bile duct dilation on ERCP. E. Extrahepatic bile duct dilation on ERCP with beaded intrahepatic bile ducts. F. Extrahepatic bile duct dilation on magnetic resonance cholangiography. Source: Patient case series, Hospital Universitario San Ignacio.
Discussion
Cholangiopathy in critically ill patients is characterized by a cholestatic pattern secondary to liver injury from multiple pathologies8, especially sepsis, trauma, and high-grade burns. Persistent damage occurs at the liver level once the underlying pathology has been resolved9. The literature proposes that one of the causes of cholangiopathy in critically ill patients is bile duct ischemia secondary to hypovolemia and hypoxia, aggravated by the everyday use of vasoconstrictor drug therapy10. Likewise, susceptibility to ischemia of the biliary tree is presented as a pathophysiological cause of this entity, explained by its unique supply of arterial blood11.
Post-COVID-19 cholangiopathy, as a new entity, has been reported by different authors, who have proposed differentiating the cholestatic pattern from the hepatocellular injury pattern described in moderate to severe COVID-19 infections5. However, there is insufficient information to determine whether this cholangiopathy corresponds to that previously reported in critically ill patients or is a separate pathology.
Our study reveals several characteristics that can contribute to understanding the pathophysiology of this disease. A significant proportion of the patients had comorbidities typically associated with more severe illness from COVID-19, such as high blood pressure (HBP) and type 2 diabetes mellitus (DM2), which could suggest susceptibility in these cases. New studies will be required to assess whether there is a genuine causal relationship.
Bacterial superinfection, exemplified by cholangitis and liver abscesses, was present in all our patients with post-COVID-19 cholangiopathy. The infection preceded the diagnosis of post-COVID-19 cholangiopathy, with documentation of gram-negative bacteria and high resistance patterns in many patients. In one of them, the condition became chronic to such a degree that it was considered incurable, so a multidisciplinary decision was made to continue broad-spectrum antibiotics indefinitely. Although sepsis is recognized as a predisposing factor for the development of cholangiopathy in critical patients9,12, new studies will be required to clarify its role in the development of post-COVID-19 cholangiopathy.
Our study identified gallstone disease in five of the eight patients as contributing to the pathology. It has been described that COVID-19 may be a risk factor for the development of choledocholithiasis in patients with cholelithiasis13; nonetheless, its role in severe disease has not been defined. We believe that the presence of cholelithiasis and choledocholithiasis in a seriously ill patient predisposes to the development of cholangitis, which would contribute to the cholestatic lesion described in patients with severe COVID-19.
The biological expression of angiotensin-converting enzyme 2 (ACE-2) receptors has been recognized as the cell entry receptor for the SARS-CoV-2 virus14, which explains the predilection of this pathogen for specific organs with high expression of these receptors. A study showed that ACE-2 receptors have increased expression in the bile ducts15, which is considered one of the leading causes of potential damage at the liver and biliary levels. Hypoxia contributes to cholestatic liver injury, in which most patients with cholangiopathy have severe lung disease or pathologies that compromise oxygenation and ventilation16.
It is striking that all of our cases occurred during 2021, even though we had many hospitalizations for COVID-19 at our institution in 2020. One possible explanation is the association of cholangiopathy with certain drugs. In our hospital, a change was made in the sedation protocols at the beginning of 2021, with which the use of ketamine, a drug that is extensively metabolized in the liver, was implemented more frequently. Ketamine has been associated with liver damage in multiple case series, initially in patients with recreational use of the drug and later also in patients with sedoanalgesia due to this drug17. A case report of two patients depicted post-COVID-19 cholangiopathy related to using ketamine18, with the extraction of black bile casts and unusual appearance12, which was consistently found in our study. The radiological findings were comparable to ketamine cholangiopathy, with biliary sepsis, intrahepatic and extrahepatic bile duct dilation, and biliary stricture19. Nevertheless, not all of our patients received ketamine before developing post-COVID-19 cholangiopathy. Propofol, used in all of our patients, has been related to the alteration of hepatobiliary transporters due to the release of cytokines, which increases the release of tumor necrosis factor-alpha (TNF-α) and interleukin (IL) 10, which has been associated with cholestasis11. However, this causality has only been seen with high doses of propofol (5-10 mg/kg/h), a quantity that none of our patients received. No studies assess the relationship between the use of ketamine and propofol and hepatobiliary injury in patients with COVID-19.
In our cases, only one patient did not have a recurrence of cholangitis and complications derived from post-COVID-19 cholangiopathy, with evidence of biliary lesion resolution on follow-up magnetic resonance cholangiography. The use of ursodeoxycholic acid and cholestyramine, drugs frequently used to manage cholestasis in different pathologies20, have not had beneficial effects in controlling recurrence.
As shown in our study, the severity and recurrence of the disease are characteristic in other case reports on post-COVID-19 cholangiopathy4,5,7. The prognosis of the disease appears to be ominous, as suggested by the fact that several of our patients have been referred for pre-liver transplant consultation. There needs to be more information on the success of this management and changes in the natural progress of the disease.
Our study expands the characterization of post-COVID-19 cholangiopathy in Latin American patients. Unlike other studies, there was no male preponderance, although the number of patients may limit these findings. To our knowledge, this series is the first to hint at a possible relationship between sepsis caused by gram-negative bacteria and the development of post-COVID-19 cholangiopathy. Likewise, the use of sedative drugs associated with liver disease, such as ketamine and propofol, is noteworthy.
Our study has limitations, and the main one is the number of patients, making it impossible to demonstrate the causality of the proposed factors; however, our data allow us to formulate hypotheses that can be formally tested in more extensive cohort studies.
Conclusions
Post-COVID-19 cholangiopathy is an emerging entity characterized by severe cholestatic liver injury associated with dilation of the intrahepatic and extrahepatic bile ducts, formation of bile casts, and recurrence of complications such as cholangitis. Our study proposes a possible relationship between the development of post-COVID-19 cholangiopathy with sepsis due to gram-negative bacteria and the use of sedoanalgesia. Complementary studies should evaluate this hypothesis.
Of importance is to evaluate in the future, with more extensive studies, the natural history of the disease, possible triggering factors, and prognoses to establish adequate management for patients with unfavorable long-term morbidity and mortality.











 texto en
texto en 




