Introduction
Severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) can cause mild respiratory infections to life-threatening severe cases; however, its clinical manifestation is diverse. While it mainly affects the respiratory system, it can also result in infrequent extrapulmonary manifestations associated with hypercoagulability states1.
Budd-Chiari syndrome (BCS) is defined as an obstruction of hepatic venous drainage, mainly caused by hypercoagulable states and the presence of neoplasms that alter the liver function or obstruct the vascular system2, and its incidence ranges from 2.0 to 2.2 per million inhabitants3. We present the clinical case of a patient diagnosed with subacute BCS of the middle subhepatic vein associated with thrombosis of the right ventricle (RV) with a recent coronavirus disease (2019) infection (COVID-19).
There are few reported cases of BCS associated with COVID-19 infection, and this article shows the heterogeneous spectrum of clinical manifestation and pathogenesis of COVID-19 when causing BCS.
Case report
This is the case of a 36-year-old woman with a history of childhood hepatitis of non-specific etiology and vitiligo since childhood, with no history of alcohol consumption. She attended the hospital due to a clinical picture of 15 days of evolution consisting of dyspnea on medium exertion, progressive deterioration of functional class (NYHA III/IV), chest pain associated with productive coughing, unquantified febrile spikes, adynamia, and general malaise.
On physical examination, her vital signs were as follows: blood pressure (BP): 115/70 mm Hg and heart rate (HR): 80 beats per minute (bpm). She was jaundiced, the vesicular murmur was decreased in both lung bases, and the abdomen was not tender on palpation and was distended. Hepatomegaly, dullness on percussion on both flanks, positive ascitic wave sign, and splenomegaly were noted. Bilateral fist percussion was positive, and she presented with grade II edema in the lower extremities, skin without superficial or deep lesions, and generalized jaundice. Initial laboratory testing revealed hyperbilirubinemia (15.27 mg/dL) at the expense of direct bilirubin (9.41 mg/dL), transaminitis (alanine aminotransferase [ALT]: 56 U/L, aspartate aminotransferase [AST]: 79 U/L), normal partial thromboplastin time (PTT) (29.7 s) with daily monitoring (26.2 s), prolonged prothrombin time (PT) (20.5 s) with daily monitoring (13.2 s) and international normalized ratio (INR; 1.7), normal glycemia (78.4 mg/dL), hypoalbuminemia (2 g/dL), elevated alkaline phosphatase (3,478 U/L), normal amylase (24 U/ L), and elevated γ-glutamyl transferase (251 U/L).
Following the COVID-19 pandemic protocol, a nasopharyngeal swab was performed based on the polymerase chain reaction (PCR) technique, which was positive. Contrast-enhanced computed tomography (CT) of the abdomen revealed consolidations in the right lower lobe with pleural effusion, dilated right atrium, RV thrombosis, preserved intra- and extrahepatic bile duct, normal gallbladder, without lithiasis. BCS was detected by the absence of blood flow at the level of the outflow tract of the middle suprahepatic vein, portal hypertension, collateral circulation, hepatomegaly, splenomegaly, ascites, and lymph nodes, predominantly inguinal (Figure 1).
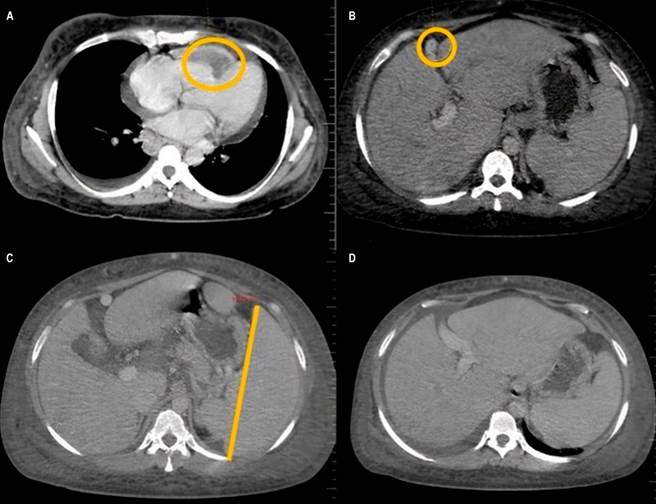
Figure 1 Contrasted CT revealing: A. Right atrial thrombosis; B. BCS detected by the absence of blood flow at the level of the outflow tract of the middle suprahepatic vein, hepatomegaly; C and D. Splenomegaly, ascites, and collateral circulation. Courtesy of the radiology department, Hospital Regional de la Orinoquia (HORO).
A chest CT confirmed the consolidation process and pericardial effusion (thickness: 7 mm). The transthoracic echocardiogram revealed a dilated right ventricle and two thrombi of equal echogenicity, one occupying most of the free wall and the other rounded, oscillating and protruding through the tricuspid valve (Figure 2), so anticoagulation with low molecular weight heparin (LMWH: 1 mg/kg/day) and diuretics was started.
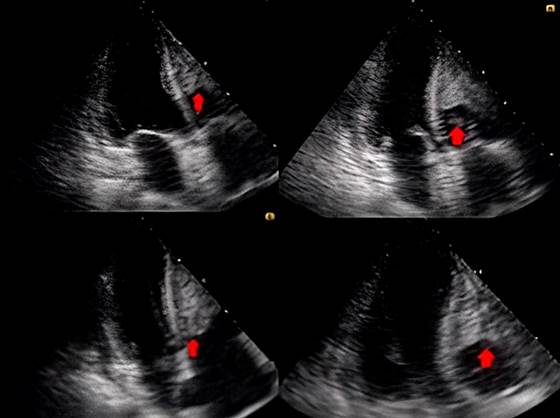
Figure 2 Transthoracic echocardiogram showing a thrombus covering most of the free wall of the right ventricle with another image of the same echogenicity, rounded, 1.6 x 1.6 cm, which oscillated and even protruded through the tricuspid valve. Courtesy of the radiology department, HORO.
The patient had mild to moderate ascites, but the clinician considered her a candidate for the invasive procedure with paracentesis. She was diagnosed with pneumonia of unclear etiology, post-COVID-19 respiratory distress syndrome, and subacute BCS of the middle suprahepatic vein associated with right ventricular thrombosis. During hospitalization, the patient clinically deteriorated due to temperature rises of up to 38.9 °C, arterial hypotension, and ventilatory failure. She required endotracheal intubation, vasopressor support, and a broad-spectrum antibiotic regimen; however, three hours later, she passed away.
The clinical characteristics of this patient are the typical manifestations of BCS. Since we did not notice associated clinical, paraclinical, and imaging findings that could be inferred from another diagnostic probability, we believe it was highly related to an infectious process caused by the SARS-CoV-2 virus.
Discussion
SARS-CoV-2 infection continues to have significant clinical manifestations. Most cases present with mild symptoms that do not affect the quality of life. In rare cases, there may be hypercoagulability states caused by alterations in Virchow’s triad and changes in serum levels of coagulation factors that put the patient at risk of ischemic pathologies such as cerebrovascular disease (5.7%), acute coronary syndrome (6%-7%), venous thromboembolic disease (deep vein thrombosis: 5.4%; pulmonary thromboembolism: 29%), and vasculitis, respectively4-6.
Within the study of the pathophysiology of BCS, the presence of thrombophilia and alterations in the patient’s coagulation is deemed an essential factor; therefore, it is most often related to neoplastic pathologies due to the hypercoagulable state that they can cause7.
Taking into account the differential diagnoses that may be associated with BCS, those considered in this clinical case are liver cirrhosis, myeloproliferative disorders (polycythemia vera, essential thrombocythemia, or coagulation disorders), carcinoma (hepatocellular, adrenal, and renal), leiomyosarcoma and space-occupying lesions of the liver such as liver cysts and sarcomas. In addition, we inquired about the administration of oral contraceptives, which were discarded based on the questioning and the diagnostic aids described7,8.
No clinical associations were found suggesting other history in the clinical case. The patient did not have alterations according to the age group, such as autoimmune diseases. She had a history of vitiligo since childhood, but there was no evidence of clinical reactivity, and she did not meet the criteria to indicate an autoimmune profile either. The main factor that predominated was a recent history of SARS-CoV-2 infection, which could explain the pathophysiological changes at the hematological level and the alterations in the vascular endothelium produced by COVID-19. We consider that the patient developed subacute BCS secondary to SARS-CoV-2 infection9.
We conducted a literature review of published cases of these two clinical entities. We found few case reports10-14, so we believe these findings are significant because we describe the diverse spectrum of the pathogenesis of COVID-19 and the heterogeneity in the clinical manifestation, as was this case of subacute BCS.











 texto en
texto en 



