Introduction
Cancer is one of the leading causes of death worldwide. In 2020, 10 million deaths were attributed to this disease, while in Colombia, it is among the first three causes of mortality. The types of cancer that cause the greatest number of deaths are lung, liver, stomach, colon, and breast. However, there are other types of cancer in rare locations that pose a diagnostic challenge and are mostly discovered late by a process of elimination or as an incidental or post-mortem finding1.
Among these rare neoplastic pathologies is primary adenocarcinoma of the duodenum, representing 0.3%-0.5% of all gastrointestinal tract carcinomas and 33%-45% of all small intestine carcinomas2. The difficulty in diagnosing small intestine tumors early can be explained by the rarity of this entity and the nonspecific and variable nature of the signs and symptoms that occur. Therefore, a delay in diagnosis is expected, which decreases the possibility of curative treatment and patient survival3,4.
This case report aims to describe the clinical-epidemiological characteristics of primary duodenal carcinoma with signet ring cells in an adult woman.
Case report
We present the case of a 57-year-old female patient with a history of high blood pressure, hysterectomy for carcinoma in situ of the cervix at age 47, resection of basal cell carcinoma on the face at age 51, and no harmful habits such as smoking or alcohol or psychoactive substance use, and without significant family history. She was admitted to the hospital for a 2-year history of intermittent abdominal pain in the right upper quadrant, with an intensity of 6/10 on the pain analog scale, which partially improved with common analgesics but was exacerbated with some foods and got worse in the last 2 months. It was associated with abdominal distention, changes in bowel habits, and unintentional weight loss of approximately 4 kg.
The patient had an initial diagnostic impression of irritable bowel syndrome, for which she received medical treatment and dietary changes without improvement. Given the persistence of the condition, a total abdominal ultrasound was performed, which showed a lesion at the level of the upper limit of the right and left lobes. An image measuring 7.45 x 4.99 cm was seen with irregular contours of mixed echogenicity bordering with the gallbladder, intra- and extrahepatic bile duct without dilation, gallbladder with poor filling, thickened walls of 0.66 cm, edematous and a hyperechoic image of 0.57 cm, which produces a solid posterior shadow cone corresponding to a stone. The rest of the examination was normal, with diagnostic impressions of cholelithiasis, cholecystitis, and liver abscess.
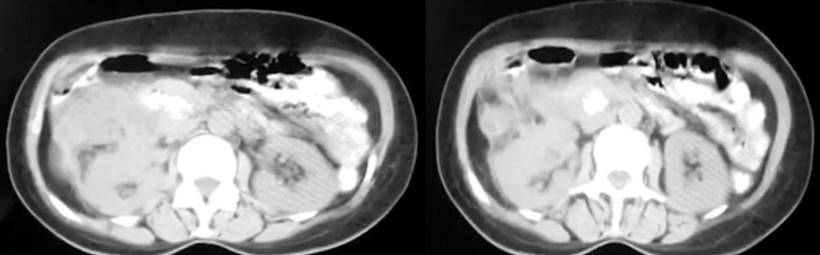
Upon admission, she was clinically stable, with pain on palpation in the right hypochondrium and, in the epigastrium, a mass of hard consistency with defined edges and immobile in the right hypochondrium could be palpated. A dynamic computed axial tomography (CT) of the liver was requested. Figure 1 shows a hypodense image at the lower edge of the right lobe towards segment V of the liver, which heterogeneously captured the intravenous iodinated contrast, possibly due to a solid neoplastic-type lesion in the liver parenchyma. However, it is impossible to characterize this lesion since the gallbladder appears small and has thick walls without showing a stone. The bile and extrahepatic ducts were found normal, and a small amount of fluid was noted in the hepatorenal space. Laboratory tests showed moderate microcytic and hypochromic anemia, hypoalbuminemia, and markedly elevated CA 19.9 antigen.
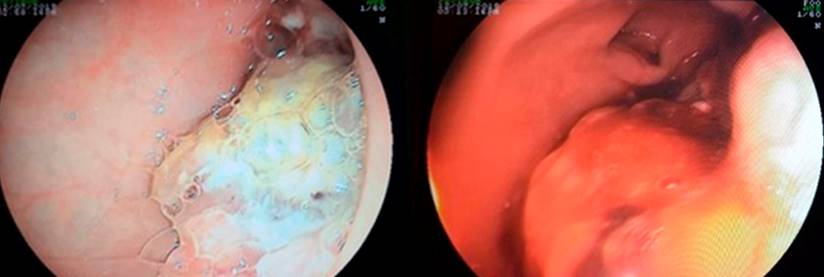
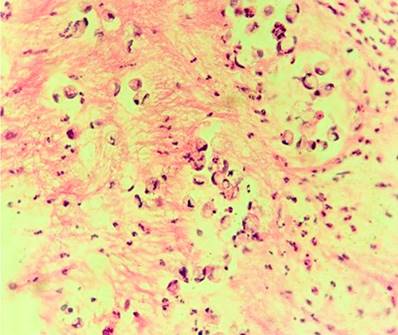
At this time, gallbladder cancer was suspected, so a liver biopsy and diagnostic laparoscopy were scheduled. During this procedure, a retroperitoneal mass was found, from which a biopsy was taken, and adhesions were observed in the gallbladder, omentum, and small and large intestine. An endoscopy of the upper GI tract was requested in the operating room (Figure 2), which revealed a bulbar exophytic lesion that occupied 30% of the circumference, non-obstructive, friable, and mamelonated. At the same time, the second duodenal portion was found to be normal. The biopsy report (Figure 3) showed findings compatible with diffuse, infiltrative, and ulcerated adenocarcinoma, while the biopsy of the retroperitoneal lesion showed fibroadipose tissue of the usual morphology free of tumor.
Immunohistochemistry of an endoscopic biopsy of the duodenal lesion was performed, which reported involvement of mucinous carcinoma with signet ring cells and reactivity in the problem cells to CKAE1/AE3, CK20, and CDX-2. The patient was referred to oncology for neoadjuvant treatment; a T3N0M0 staging was performed. It was determined that since it is a rare pathology, there are no defined schemes for metastasis or neoadjuvant therapy, suggesting that a surgical procedure be performed as soon as possible.
At a medical meeting, the oncological gastrointestinal surgery service decided to perform a pancreaticoduodenectomy. However, given the poor nutritional status and hypoalbuminemia, it was decided to provide nutritional support, which was unsuccessful. During that time, there was deterioration in the patient. In a new evaluation, it was found that the size of the tumor now occupied 50% of the circumference involving the first and second portion of the duodenum and extended through the retroperitoneal region through the gastrocolic ligament, with firm adhesions to the liver at the greater curvature and the hepatic and colon angle, in addition to a progression of descent albumin at 1.7 g/dL and weight loss of 17 kg. At this point, it was considered an unresectable tumor, so the medical board decided not to perform curative surgical treatment because the risks were greater than the benefits of surgery. She died 2 months later as a result of abdominal sepsis that produced septic shock 8 months after diagnosis.
Discussion
Malignant duodenal tumors are a rare disease, reflected in the small number of cases reported worldwide5-11. Its infrequency may be justified by possible defense mechanisms of this portion of the small intestine, the speed with which the bolus passes through the duodenum, the secretions that reduce the exposure time of the mucosa and epithelium to different carcinogens, and the relative duodenal sterility, among other protective factors of the intestinal wall3.
The factors that increase the risk of suffering from the disease have not been clarified; some authors have proposed the relationship between the appearance of adenocarcinoma and a previous adenoma, following the evolution already described in colorectal cancer5,6. Adenocarcinoma is most frequently located in the second portion of the duodenum, followed by the third and fourth portions. However, in the case described, the tumor lesion was found in the first portion3-5.
The case presented is an adult woman, although, in the reported literature, this disease is more common in men between 50 and 60 years old5-8. In turn, two of the patients who were part of the series of cases reported by Marcos et al. had a history of cervical cancer, as in our case. Still, it is not possible to establish a causal relationship8.
The small number of patients in the case series in the literature limits the establishment of diagnostic criteria, taking into account that the predominant symptoms are nonspecific and variable, and the typical triad is hyporexia, vomiting, and weight loss. Other symptoms are abdominal pain, obstruction, jaundice when located in the periampullary region, gastrointestinal bleeding, and perforation2,6,9. Ortiz et al. described a condition consisting of nausea, postprandial fullness, and vomiting10. Moreno-Loaiza described weight loss and bleeding as the most frequent symptoms11. In the case presented in this study, the patient presented with symptoms of abdominal pain, nausea, hyporexia, and weight loss, which coincides with the conditions described by Ramia et al.5, Peño Muñoz et al.6, and Chung et al.2. On the other hand, signet ring cells in the duodenal bulb are not a common finding and their presence could be explained as heterotopic gastric mucosa. Authors have proposed that it could be due to metaplasia upon exposure to intraluminal hydrochloric acid, which can be a hypothesis about the pathophysiology of this entity6,8,12.
The diagnosis is made by directly observing the lesion through esophagogastroduodenoscopy, biopsy, and immunohistochemistry studies. Thus, early performance of upper GI tract endoscopy is of utmost importance in patients with clinical symptoms of abdominal pain, weight loss, and abdominal mass. Surgical treatment is the only curative therapeutic option successful when an early diagnosis is made10. There is insufficient evidence about the usefulness of chemotherapy as a treatment for this type of neoplasia. However, the choice in most cases described so far has been 5-fluorouracil due to its known effectiveness in colon and gastric cancer5.
Conclusion
Duodenal carcinoma is a diagnostic challenge due to its rarity and the nonspecific and variable nature of its clinical manifestations. It is advisable to consider this entity in patients with nausea, emesis, abdominal pain, and weight loss symptoms and confirm the diagnosis by performing upper GI tract endoscopy, histological study, and immunohistochemistry. Late discovery of the disease decreases the possibility of curative treatment and patient survival. This article is a reference framework for future research, improvement in clinician decision-making, and knowledge of the academic community.











 texto em
texto em