Introduction
Herpes esophagitis is a well-known and described entity that usually occurs in patients with severe immunosuppression. This disease is also described in immunocompetent patients, only much less frequently: this group represents 4% of affected people1. These patients usually present with predisposing factors such as alcohol use, eosinophilic esophagitis, malnutrition, or esophageal diseases associated with acid-peptic disease2. This article presents a case of herpetic esophagitis in a young patient without any previous comorbidity or known risk factors.
Case description
We present the case of a 17-year-old male patient with no known history. He consulted the emergency room due to a 4-day history of substernal pain with ill-defined characteristics that did not radiate and was associated with dysphagia for solids and liquids that caused total intolerance to the oral route. The condition was accompanied by a fever measured at 38.4 °C and dysuria. The patient denied any history of repeated bacterial or viral infections and, in general, any recurrent infections. He also did not report risky sexual behavior.
His vital signs on admission were blood pressure: 90/60 mm Hg, heart rate: 117 beats per minute (bpm), respiratory rate: 18 breaths per minute (rpm), oxygen saturation: 97%, and inspired fraction of oxygen: 21%. The physical examination revealed ulcerated oropharyngeal lesions and abdominal pain on both sides associated with bilateral positive fist-percussion.
The admission paraclinic tests showed creatinine: 1.31 mg/dL, urea nitrogen: 18 mg/dL, C-reactive protein: 4.81 mg/dL, hemoglobin: 16.4 mg/dL, hematocrit: 47.6%, leukocytes: 10,000/mm3, neutrophils: 7,100/mm3, lymphocytes: 1,200/mm3, platelets: 222,000/mm3, enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV): negative, treponemal test: negative, cytochemical urine with gram-positive cocci and renal ultrasound with changes due to right pyelonephritis.
Dysphagia/odynophagia was studied with upper gastrointestinal endoscopy, which revealed severe ulcerated esophagitis, with a circumferential ulcer in the entire distal third and several triangular ulcers that ascended to the middle third, accompanied by cottony plaques in the proximal third that were hardly removed with washing (Figure 1). Given the findings, an infectious origin of the esophagitis was suspected, and biopsies were taken, showing an ulcerated mucosa with foci of necrosis, numerous neutrophils, cellular debris, lymphoplasmocytes, hemorrhage, and abundant multinucleated giant cells. Immunohistochemistry for herpes type I had strongly positive staining in the multinucleated giant cells (Figure 2).
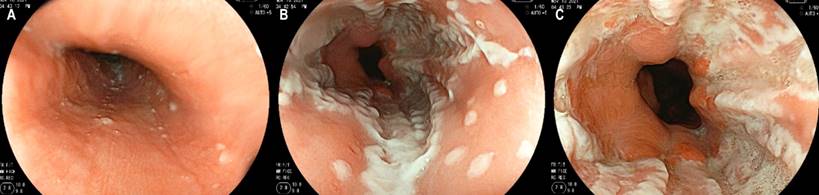
Figure 1 Upper endoscopy of the patient with herpetic esophagitis, lesions in different stages of evolution, from isolated vesicles to erosions and confluent ulcers. A. Proximal esophagus. B. Middle esophagus. C. Distal esophagus. Authors’ archives.
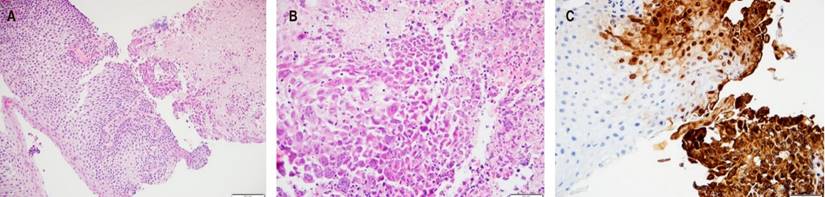
Figure 2 Biopsy of ulcers seen in Figure 1. A. Hematoxylin and eosin 200x. B. Hematoxylin and eosin 400x. C. Immunohistochemistry of herpes simplex virus type 1, 200x. Authors’ archives.
Empirical antibiotic treatment was started with piperacillin/tazobactam for pyelonephritis and intravenous acyclovir for esophagitis. After 72 hours, there was significant symptomatic improvement and tolerance to the oral route, so the patient was discharged with oral acyclovir to complete 10 days in total with this drug. The patient was followed up at home, and symptoms were wholly improved with the resolution of the oropharyngeal lesions.
Discussion
A case of a patient with this herpes esophagitis concomitant with pyelonephritis was presented. This last entity occurs in 1.15% of people under 18 years of age3, regardless of whether they have immunosuppression. It has an annual rate of 3-4 cases per 10,000 men, irrespective of their immunological status4. The patient had no history of repeated viral or bacterial infections, much less in sites suggestive of primary immunodeficiency, such as the sinopulmonary tract and mucosal surfaces5, nor past infections caused by encapsulated germs or enteric pathogens suggestive of humoral immunodeficiency6,7. Therefore, given that he had a negative HIV test in the absence of risky sexual behavior and that herpetic esophagitis can occur in people without immunodeficiencies8,9, without the need for further studies, it was considered that he was an immunocompetent patient.
Although the herpes simplex virus (HSV) affects up to 90% of the general population10, HSV esophagitis in immunocompetent patients is rare. In patients without immunodeficiency, literature reviews report few cases of a predominance of infection in males (70% versus 30%). This ratio is lost in patients over 4011. The average age at infection is 28 to 35 years9,11. Esophagitis caused by HSV type 1 is more common than that caused by HSV type 22,9.
In immunosuppressed patients, the most common cause is the reactivation of a latent infection, while in immunocompetent patients, it occurs more frequently during primary infections10. However, a literature review showed that the disease associated with the reactivation of the condition is also prevalent in this population9.
The most common clinical manifestation in patients affected by herpetic esophagitis is accompanied by odynophagia or dysphagia12, symptoms that occur in 60% and 37.5% of cases9. Additionally, there may be fever in 51% of cases, chest pain in 46%, and viral prodrome in up to 26% of affected patients9. It is not uncommon to also find lip and oropharyngeal lesions; in a few cases, lesions have been described in the hands and feet11. Although gastrointestinal bleeding, Mallory-Weiss lesions, and esophageal perforation have been reported, they are rare complications of the disease9,10.
The diagnosis begins with clinical suspicion followed by endoscopic studies in which ulcers with raised edges are usually found that are predominant in the distal thirds of the esophagus. These raised edges may give the appearance of “volcano-like” ulcers, which macroscopically helps differentiate them from cytomegalovirus involvement, in which the systemic condition and digestive symptoms may be similar. However, the ulcers tend to be linear, longitudinal, and deeper1,11,13.
The distal esophagus is affected in more than 60% of cases, and the middle esophagus in up to 40%. Isolated middle and proximal third infections are much less frequent11. The final diagnosis is made through histopathological analysis of esophageal biopsies, in which ballooning degeneration of epithelial cells, multinucleated giant cells, Cowdry type A inclusions, and immunohistochemical staining for viruses are found10. Moreover, molecular biology studies are also helpful14,15. When conventional histopathological analysis is associated with polymerase chain reaction, a diagnostic yield of up to 90% can be achieved9. The serological diagnosis of primary infection is made with the positivization of antibodies or a four-fold increase in immunoglobulin G (IgG) between the acute disease stage and recovery 10.
Patients with herpetic esophagitis have a good prognosis. The condition is self-limiting in all cases described. No clinical trials or high-quality evidence supports its management, especially antiviral therapy versus placebo. However, a shorter duration of symptoms has been reported with acyclovir16, findings that are also extrapolated from its beneficial use in genital HSV infections17. The treatment time in the reports is 7-14 days9.
So, it can be noted that, in our case, the patient had a typical clinical picture of HSV-1 infection in the esophagus. The dysphagia led to a digestive endoscopy being performed, whose findings of non-typical esophagitis due to reflux, with suspicion of an infectious origin, motivated the taking of biopsies that finally confirmed the diagnosis. Optimal management could be provided with which his symptoms were resolved and associated complications were avoided.











 texto en
texto en 



