Introduction
The measurement and quantification of the functionality of the esophagogastric junction (EGJ) allow the establishment of adequate competence of this barrier mechanism. They can provide valuable information on conditions or pathologies in which it can be altered, such as gastroesophageal reflux disease (GERD)1,2, postoperative states of myotomy in patients with achalasia, postoperative states of anti-reflux surgery, among others.
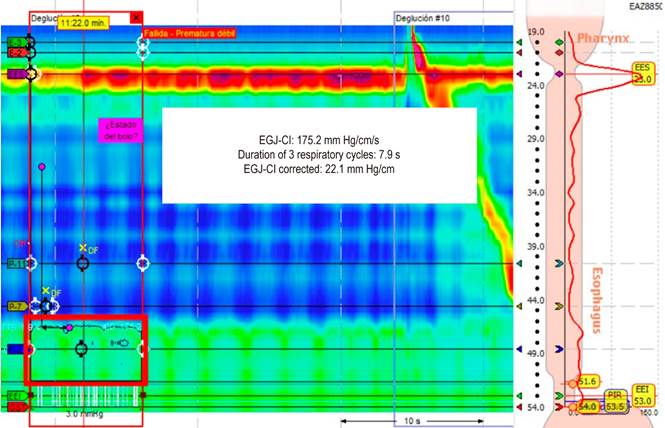
The Lyon Consensus proposes two parameters of esophageal high-resolution manometry (HRM) to observe the EGJ’s function: the anatomical morphology of the EGJ and contractile vigor3,4. The morphology of the EGJ is defined by the relationship between the lower esophageal sphincter (LES) and the crura of the diaphragm (CD). Three types of EGJ morphology are proposed: Type 1 when the LES and CD are superimposed, Type 2 when the LES and CD are separated by less than 2 cm, and Type 3 when the separation is greater than 2 cm3-5. The contractile vigor of the EGJ or esophagogastric junction contractile integral (EGJ-CI) is calculated using a similar method to that of the distal contractile integral (DCI). The DCI frame is placed over the EGJ to include three respiratory cycles; the average value recorded in mm Hg/cm/s is divided by the duration of the three respiratory cycles to obtain the EGJ-CI in mm Hg/cm (Figure 1)3,6.
Authors’ archives.
Figure 1 The distal contractile integral frame (red frame) is placed over the EGJ to include three respiratory cycles; the value recorded in mm Hg/cm/s is divided by the duration of the three respiratory cycles to obtain the EGJ-CI in mm Hg/cm.
The study by Nicodeme et al. evaluated the severity of gastroesophageal reflux defined by pH impedance variables such as acid exposure time (AET), the number of reflux episodes in 24 hours, and a symptomatic index greater than 50%. They found that a greater EGJ-CI in the HRM was associated with fewer reflux episodes6.
Although different GERD phenotypes have been described based on clinical, pH impedance, and endoscopic parameters, such as acid, non-acid, erosive, and non-erosive reflux, it has not been possible to define factors that can predict these phenotypes. Specifically, it has not been determined whether the assessment of the EGJ competence, especially the EGJ-CI, could be helpful in this context. Defining it would be clinically relevant since the treatment and prognosis of each phenotype differs significantly7.
The present study aims to describe the function of the EGJ, including anatomical morphology and EGJ-CI in various GERD phenotypes, using pH-impedance testing and upper GI tract endoscopy as the gold standard.
Materials and methods
We conducted an analytical observational study, which included patients with a diagnosis of GERD confirmed by pH impedance or endoscopic findings that were taken for esophageal manometry in the gastroenterology unit of the Hospital Universitario San Ignacio, a referral hospital in Bogotá (Colombia), between June 2019 and June 2021. Patients over 18 with simultaneous HRM, pH-impedance testing, and upper GI endoscopy were included. Patients with incomplete manometries for any reason, a history of upper GI surgery (total or partial gastrectomy), esophageal interventions, achalasia, outflow tract obstruction, Jackhammer, and hypercontractile esophagus, as well as patients who did not meet the GERD criteria, were excluded. The Hospital Universitario San Ignacio and the Pontificia Universidad Javeriana ethics committee approved the study under code FM-CIE-1992-21/246/2021.
The endoscopic procedures (esophagogastroduodenoscopy) were performed by gastroenterologists attached to the Hospital Universitario San Ignacio. The manometry and pH-impedance studies were conducted by duly trained nursing staff, and gastroenterology fellows analyzed them under the supervision and approval of certified gastroenterologist members of the digestive physiology group. The manometries were analyzed according to the parameters of the Chicago Classification v4.0 and the pH-impedance tests according to the guidelines of the Lyon Consensus15,16. Demographic data and the results of the different tests were obtained from the records systematically filled out in the unit and collected using a standardized form.
Non-acid reflux was defined as more than 27 reflux episodes when the patient came without treatment and more than 44 reflux episodes if the patient came with treatment. Acid reflux was determined as AET > 6%, or, in patients with AET in the gray zone (between 4% and 6%), as a number of acid refluxes greater than 80, a DeeMester score greater than 14.7, a post-reflux swallow-induced peristaltic wave index greater than 61% and the mean nocturnal baseline impedance less than 2,292 ohms. Non-erosive reflux was defined as those patients with routine endoscopy, and erosive reflux as the presence of Grade C and D esophagitis according to the Los Angeles Classification, Barrett’s esophagus, or peptic stricture16.
The EGJ-CI measurement used the DCI frame placed over the EGJ to include three respiratory cycles. The value recorded in mm Hg/cm/s is divided by the duration of the three respiratory cycles to obtain the EGJ-CI in mm Hg/cm (Figure 1).
Continuous variables were described using measures of central tendency and dispersion. A Shapiro-Wilk test was used to define whether the normality criterion in the data distribution was met. If met, the mean and standard deviation were described; otherwise, the median and interquartile range. Categorical variables were defined with absolute numbers and percentages. The groups generated according to the erosive, non-erosive, acid, and non-acid phenotypes were compared using a t-test or a Mann-Whitney U test. A Stata 16 statistical package was used for the analysis.
Results
Seventy-two patients were included, with a mean age of 54.9 years (standard deviation [SD]: 14.1) and a predominance of the female sex (63%). Regurgitation and heartburn were the most frequent symptoms (66%), followed by cough and belching, with a frequency of 31% and 11%, respectively. The indication for performing pH-impedance testing in order of frequency was GERD, presurgery, typical symptoms, atypical symptoms, and patients with chest pain and dysphagia (Table 1). Of the patients included in the study, 34.7% did not receive any PPI, and 2% received alginate as a treatment strategy for GERD. The most frequently used PPI was esomeprazole, with 26%, followed by lansoprazole, dexlansoprazole, and pantoprazole (Table 1).
Table 1 Clinical characteristics and treatment received by the included patients
SD: standard deviation; n = number. Prepared by the authors.
The comparison of manometric variables between patients with and without acid reflux and those with and without non-acid reflux is presented in Table 2; the mean LES pressure, the end-inspiratory LES pressure, the median IRP (integrated relaxation pressure), DCI, and EGJ-CI had no statistically significant differences between the groups.
Table 2 Comparison of manometric variables in patients with or without acid and non-acid reflux
| Manometric variable | Acid reflux | Non-acid reflux | ||||
|---|---|---|---|---|---|---|
| Positive, n = 59 | Negative, n = 13 | p-value | Positive, n = 34 | Negative, n = 38 | p-value | |
| Mean LES pressure (mm Hg), median (IQR) | 10,4 (3,6 -21,9) | 13,1 (11,6 -23,8) | 0,08 | 12,1 (8,5-23,8) | 10,1 (3,6 -15) | 0,11 |
| End-inspiratory LES pressure (mm Hg), median (IQR) | 9,6 (5,9-15,4) | 9,4 (5,9-12,9) | 0,75 | 8,4 (5,2 -13,3) | 9,85 (6,2 -15,4) | 0,53 |
| Median IRP (IQR) | 3,9 (2,0-6,7) | 4,4 (1,4-6,2) | 0,80 | 4,3 (1,4-6,2) | 3,9 (2,1-7,3) | 0,48 |
| DCI mm Hg, median (IQR) | 1551 (910 -2412) | 1476 (774-1862) | 0,53 | 1660 (1021-2134) | 1389 (783-2320) | 0,52 |
| EGJ-CI, median (IQR) | 21 (14-44) | 15 (11-28) | 0,24 | 20,5 (12,7-30,0) | 20 (14-44) | 0,80 |
| EGJ type, n (%) | ||||||
| I | 8 (13,50) | 2 (15, 38) | 0,82 | 6 (17,65) | 4 (10,53) | 0,04 |
| II | 21 (35,59) | 6 (46, 15) | 17(50,00) | 10 (26,32) | ||
| IIIa | 16 (27,12) | 2 (15,38) | 4 (11,7) | 14 (36,84) | ||
| IIIb | 14 (23,73) | 3 (23,08) | 7 (20,59) | 10 (26,32) | ||
DCI: distal contractile integral; IQR: interquartile range; IRP: integrated relaxation pressure; LES: lower esophageal sphincter. Prepared by the authors.
The type of EGJ was different between patients with a positive versus negative pH impedance study for non-acid reflux (p = 0.04), with a more considerable proportion of patients with Type IIIa or IIIb EGJ among patients without that type of reflux (63.1% versus 31.3%). Among patients with acid reflux, no statistically significant differences were found in the variables studied (Table 2).
Lower end-inspiratory LES pressure was detected in patients with erosive reflux than those with non-erosive reflux (median: 6.1 vs. 11.9; p < 0.01). There was a similar when evaluating the EGJ-CI (median: 15.1 vs. 23, p = 0.04). The proportion of patients with Type IIIa and IIIb EGJ was higher in patients with erosive reflux (83.3% vs. 37.1%; p < 0.01) (Table 3).
Table 3 Comparison of manometric variables between erosive reflux and non-erosive reflux
| Manometric variable | Erosive reflux | ||
|---|---|---|---|
| Positive, n = 18 | Negative, n = 54 | p-value | |
| Mean LES pressure (mm Hg), median (IQR) | 9,9 (4,0-11,6) | 11,5 (5,0 -23,8) | 0,09 |
| End-inspiratory LES pressure (mm Hg), median (IQR) | 6,1 (2,8-7,5) | 11,9 (6,6-17,4) | < 0,01 |
| Median IRP (IQR) | 3,75 (2,3-6,6) | 4,3 (2,8-6,3) | 0,94 |
| DCI (mm Hg), median (IQR) | 1549 (783-2007) | 1546 (991-2241) | 0,41 |
| EGJ-CI, median (IQR) | 15,1 (7-25) | 23 (14-42,0) | 0,04 |
| EGJ type, n (%) | |||
| I | 2,0 (11,1) | 8,0 (14,8) | < 0,01 |
| II | 1,0 (5,6) | 26,0 (48,2) | |
| IIIa | 9,0 (50,0) | 9,0 (16,7) | |
| IIIb | 6,0 (33,3) | 11,0 (20,4) | |
DCI: distal contractility integral; IQR: interquartile range; IRP: integrated relaxation pressure; LES: lower esophageal sphincter. Prepared by the authors.
Discussion
The present study described the function of the EGJ in the different reflux phenotypes (acid, non-acid, erosive, and non-erosive) and found that Type IIIa and IIIb EGJs were more frequent in patients with erosive esophagitis and less common among patients with non-acid reflux. Additionally, EGJ-CI is significantly lower in patients with erosive reflux.
In our study, the symptoms that most frequently occurred in the population with GERD were regurgitation and heartburn, and the highest proportion of patients were women. These results correlate with what was documented by Paramo et al. in a published study of the prevalence of symptoms of gastroesophageal reflux and associated factors in the Colombian population11.
The PPI most frequently prescribed in our population was esomeprazole, followed by lansoprazole and dexlansoprazole, molecules with proven effectiveness in managing GERD according to different published studies12.
When the manometric variables were evaluated in patients with and without acid reflux, we did not find significant differences in EGJ-CI, contrary to what was reported by Gor et al.13, who found an inverse correlation between EGJ-CI and gastroesophageal reflux determined by AET. No statistically significant differences were found in the mentioned manometric parameters when the analysis was performed for the non-acid reflux subgroup. This finding could be because all of the patients in that study did not receive antisecretory therapy, while our study included patients with and without antisecretory treatment.
When evaluating the manometric variables between erosive and non-erosive reflux, our results were similar to those by Hyoju Ham et al., who reported that EGJ-CI is significantly correlated with the morphology of the EGJ, establishing the presence of GERD when the morphology of the EGJ is altered. For example, a Type 3 EGJ was associated with a more significant number of reflux episodes, a finding also correlated with EGJ-CI alteration14. Furthermore, our study demonstrated that the EGJ-CI is significantly decreased in patients with erosive GERD compared to non-erosive GERD (p = 0.04), representing a greater impairment of the barrier mechanism in the EGJ. Finally, we documented a significant decrease in end-inspiratory LES pressure among patients with erosive GERD compared to patients with non-erosive GERD (p < 0.01). The above shows us that the EGJ-CI is a new manometric parameter altered in patients with erosive and non-erosive GERD, significantly correlated with the alteration of end-inspiratory LES pressure and Type 3 EGJ. These results suggest that alteration of EGJ-CI could predict erosive reflux in our population and allow us to understand how the impairment of the anti-reflux barrier in patients with erosive GERD is more significant than in those with non-erosive GERD.
Wang et al. established a normal cut-off point for EGJ-CI with a mean of 34.7 mm Hg and a range between 26.2 and 58.3 mm Hg15; these results are compatible with ours, given that in our population with erosive GERD, the EGJ-CI had a median of 15.1 with a range between 7 and 25 mm Hg, decreased compared to this cut-off point established for healthy patients. In patients with non-erosive GERD, a decrease in EGJ-IC was also documented concerning these cut-off points, suggesting a dysfunction of the EGJ barrier mechanism in these patients. A recent study published by Rogers et al., who evaluated the EGJ in healthy patients using the two manometric parameters described (EGJ type and EGJ-CI), established normal cut-off points for the EGJ-CI, very similar to those provided by Wang et al.16 and Jasper et al.17.
Tolone et al. explained that 50% of patients with decreased EGJ-CI present with GERD, and 14% have functional heartburn; data suggest that decreased EGJ-CI is associated with a longer AET, greater number of reflux episodes and esophageal mucosal damage documented on endoscopy18. These findings were duly noted in our population for patients with erosive and non-erosive GERD.
We can conclude that in the Colombian population, the EGJ-CI objectively evaluates the barrier mechanism of the EGJ since it is decreased in all patients with GERD. Furthermore, as shown in our study, it allowed a characterization of patients with erosive esophagitis, given that the EGJ-CI in this group was found to be significantly decreased, which was correlated with the decrease in end-inspiratory LES pressure and Type IIIa and IIIb EGJ.
Conclusion
In our population, decreased EGJ-CI was significantly correlated with erosive GERD, suggesting that a reduction in EGJ-CI values could predict this condition in patients with GERD. This result is appropriately related to the type of EGJ morphology, with Type III being the most frequent, and lower end-inspiratory LES pressure, allowing us to characterize this reflux phenotype better to guarantee an appropriate diagnostic and therapeutic approach.











 texto em
texto em 



