Introduction
Percutaneous endoscopic gastrostomy (PEG) is a method to guarantee nutrition for patients with dysphagia of different etiologies and risk of broncho-aspiration, among others. Since its introduction by Gauderer and Ponsky in 19801, it has become one of the most used methods for this purpose. In the United States, nearly 250,000 procedures are performed yearly2. Still, despite their safety and technical ease, complications can occur in 0.4% to 22.5%3, which, depending on their severity, can be classified as major and minor (Table 1 and Video 1).
Table 1 Complications of percutaneous endoscopic gastrostomy3
| Major complications | Minor complications |
|---|---|
| Necrotizing fasciitis | Skin infection |
| Buried bumper syndrome | Peristomal leakage |
| Colocutaneous fistula | Pneumoperitoneum |
| Gastrocolic fistula | Ileus |
| Gastric perforation | Bleeding |
| Massive broncho-aspiration | Tube site ulceration |
| Blockage due to food sediment | |
| Tube deterioration | |
| Gastric outlet obstruction |
Taken from: Itkin M, et al. Gastroenterology. 2011;141(2):742-765.

Source: Unidad de Gastroenterología y Ecoendoscopia UGEC (2019, August 25th). Gastrostomía [video]. YouTube. https://n9.cl/fam1h
Video 1 Video of the main complications of endoscopic gastrostomy.
One of the most feared complications of gastrostomy is buried bumper syndrome (BBS), whose incidence is 1% (0.3%-2.4%)3. It is characterized by the following triad: inability to insert the tube, loss of permeability, and leakage through the tube’s stoma4, and occurs when the internal end of the gastrostomy migrates toward the stomach wall, even to the point of coming out of it. Therapy depends on migration related to the muscularis propria. In turn, BBS can cause other complications such as bleeding, perforation, peritonitis, and intra-abdominal or wall abscesses5.
From the pathophysiological point of view, BBS occurs due to an increase in pressure between the internal and external fixation of the gastrostomy, resulting in ischemia and necrosis of the tissue, then inflammation and fibrosis, and finally, the displacement of the external fixation and thus the BBS5. The main risk factors depend on the tube, the procedure, care with the device, and the patient (Figure 1).
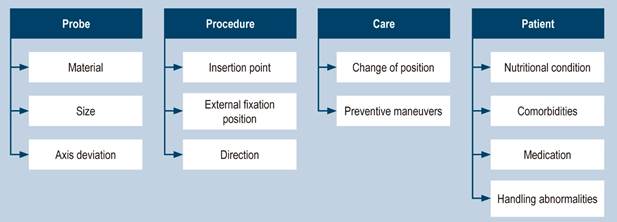
Figure 1 Risk factors for BBS5. Taken from: Schwartz HI et al. PEG feeding tube migration impaction in the abdominal wall. Gastrointest Endosc. 1989;35(2):134.
From a diagnostic perspective, once the characteristic triad is suspected, an endoscopy of the upper GI tract and imaging should be performed to assess the relationship of the external fixation with the gastric wall. Then, the best available therapy, which can be medical, endoscopic, or surgical, will be given (Table 2)1.
Table 2 BBS severity classification6
| Grade | Clinical | Endoscopic | Radiological | Treatment |
|---|---|---|---|---|
| 0 | Movable | Normal | No | Prevention |
| 1 | Movable | Ulcer around the disc | No | Prevention |
| 2 | Fixed | >50% of the disk is visible | No | Endoscopy |
| 3 | Fixed | 100% covered | Disc inside the stomach | Endoscopy, dissection |
| 4 | Fixed/Blocked | 100% covered | Disc outside the stomach | Endoscopy, dissection |
| 5 | Subcutaneous disc | 100% covered | No | Surgery/Extraction |
Taken from: McClave SA, et al. Gastrointest Endosc Clin N Am. 2007;17(4):731-746.
Below is a series of clinical cases illustrating serious complications after endoscopic gastrostomy7,8. We must be aware of such complications and evaluate the patient well before deciding whether the procedure is indicated, together with the patient and their family.
Case 1
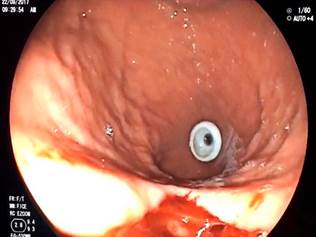
A 54-year-old female patient with a history of an extensive hemorrhagic stroke and severe compromise in the swallowing pattern without a good response to rehabilitation underwent a PEG. Ten days later, a call was received from the treatment group due to an obstruction to the nutrition passage of the gastrostomy. Due to suspicion of BBS, we decided to perform an endoscopy, which showed the internal disc occluded by gastric tissue in more than 50% (Figure 2). An attempt was made to recover the foreign body with forceps unsuccessfully. So, a tube was cut before the external retention disc, and the guidewire was advanced through it. It was retrieved with a handle and attached to the gastrostomy tube, which was pulled using the push-pull technique. Once it came out through the abdominal wall, the tube was recovered, and the fistula was left patent with the new tube in a suitable position.
Case 2
A 44-year-old female patient with a history of severe head trauma and severe swallowing disorder required a PEG. She was received through interconsultation for not having adequate mobility of the tube and a peristomal leak. We decided to take her to an endoscopy, showing an absence of the internal disc in the gastric cavity. Finally, she was diagnosed with Type 3 BBS (Figure 3). We performed a precut dissection in which the affected internal disc was found in the gastric wall. Once freed, it was successfully extracted.
Case 3
A 65-year-old male patient with sequelae of post-cardiac arrest hypoxic-ischemic encephalopathy required PEG due to a severe swallowing disorder. The attending group requested an evaluation (15 days after the gastrostomy) due to liquid stools with the same characteristics as the nutrition each time it was administered through a tube. He underwent an endoscopy, and the internal disc was not found. Given the clinical picture, displacement of the internal disc outside the stomach (gastrocolic fistula) was suspected (Figure 4). A total colonoscopy was performed, finding the internal retention disc of the gastrostomy at the transverse colon level. We decided to remove the tube and leave him under observation for seven days, after which total closure of the fistula was observed on endoscopic follow-up.
Case 4
A 74-year-old male patient with sequelae of an ischemic stroke required endoscopic gastrostomy. Once the tube was pulled toward the wall and the external retention disc was fixed, an endoscopy was performed to assess the position, finding a severe tear of the gastric mucosa toward the greater curvature (Figure 5); no overt perforation was observed endoscopically. The patient did not have an acute abdomen on physical examination, so the gastrostomy was fixed and left under observation. A new endoscopy was performed seven days later, noting that the tear had healed.
Case 5
A 50-year-old male patient with sequelae of an ischemic stroke underwent PEG for a swallowing disorder. Seventy-two hours after the procedure, edema and erythema were found in the peristomal area, rapidly progressing to the rest of the abdominal wall, forming fasciitis (Figure 6). A soft tissue ultrasound was performed without finding wall collections but fascia inflammation. With the diagnosis of surgical site infection, the tube was removed, and parenteral antibiotic therapy was started. The nasogastric nutrition tube was advanced to ensure enteral nutrition. Once the infection resolved, a new gastrostomy was performed without complications.
Conclusions
Endoscopic gastrostomy is a therapeutic procedure performed regularly in clinical practice, given the high incidence of diseases that result in swallowing disorders or oral tolerance. However, the frequent use of this procedure does not exempt it from mild or complex complications, such as those shown in this work.
Infection, bleeding, and diverse types of BBS are the most common complications. These depend on multiple factors, which must be controlled to prevent their occurrence. Once suspected, the physical examination is vital, and the tube seeks to assess the triad of BBS: absence of mobility, parastomal leak, and obstruction to fluid passage. The assessment must be complemented with an endoscopy and, if necessary, a radiological study to classify the complication and plan the best possible treatment, ranging from observation to endoscopic or surgical management.











 texto en
texto en