Introduction
Primary anorectal melanoma (PAM) is a rare pathology that represents less than 1% of all colorectal tumors1. The primary gastrointestinal mucosal location is the third most common after the skin and retina and mainly affects women between the fifth and sixth decade of life2. At the anorectal level, the lesion can appear anywhere melanocytes are found (perianal region, transitional zone, or rectal mucosa)3. The most frequently described clinical manifestations are rectal bleeding, the sensation of mass, and alterations in defecation. It is not uncommon for these lesions to be confused with complicated hemorrhoidal disease, which delays the diagnosis and negatively impacts the prognosis4.
Clinical case
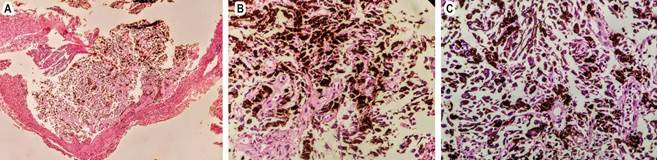
A 56-year-old woman with a history of rectal bleeding and hematochezia was referred with a diagnosis of thrombosed internal hemorrhoids. During the gastroenterology evaluation, a rectal examination and anoscopy were performed, identifying an indurated violaceous mass that protruded through the anal canal. The colonoscopy revealed a 3-cm violaceous polypoid lesion with ulcerated foci and stigmata of recent bleeding (Figure 1). In the thoracoabdominal computed tomography (CT), no lesions suspicious of metastasis or lymph node involvement were found. Subsequently, a transanal surgical resection of the lesion was performed, and the pathology was reported as a semi-pedunculated polypoid formation covered by grayish mucosa, limited to the submucosa without vascular or perineural invasion. Histology describes a malignant cell tumor with hyperchromatic pleomorphic nuclei with nucleolus, abundant brown pigment in their cytoplasm, and extensive superficial ulceration (Figure 2). Finally, the patient was assessed by dermatology and ophthalmology, who found no skin or ocular lesions suggestive of melanoma. The patient continues to be followed up by gastroenterology and oncology; there is no evidence of local or imaging recurrence.
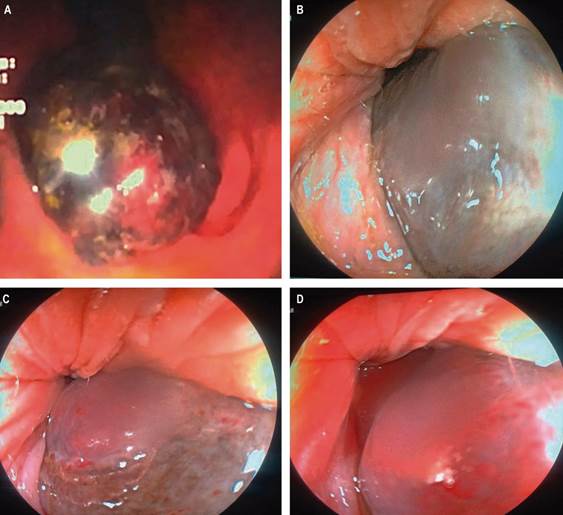
Source: Case photos, authors’ archive.
Figure 1 Colonoscopy imaging. A. In retroflexion, a hyperpigmented polyploid-looking lesion involving the distal rectum is observed. B, C, and D. A polyploid-looking lesion is observed that protrudes through the anal canal.
Discussion
PAM was first described in 1857 by Moore; it is a rare pathology, with an incidence of 1.7 cases per million inhabitants5. Mucosal melanoma (MM) represents the third most common site of primary melanomas after the skin and eyes, and the incidence varies depending on its location6 (Table 1). Compared to cutaneous melanoma (CM), primary gastrointestinal melanoma is sporadic; its most frequent location is the anorectum (more than 50%), followed by the stomach, small intestine, and colon. Rectal location is more frequent than anal7. Countries with a high incidence of CM have similar incidence rates of MM compared to other geographic regions8. It is more common in women than men (2:1 ratio), and the average age at diagnosis is 54.5 years9, coinciding with the case presented. Overall survival is poor and ranges between 10% and 20% at five years, probably because of late diagnosis10. Most cases arise from the mucocutaneous junction; however, they can also arise from the skin of the anal verge, the transitional epithelium of the anal canal, or the rectal mucosa11.
Table 1 Epidemiology of primary mucosal melanoma
| Primary mucosal melanoma | Cases/million/year |
|---|---|
| Conjunctival | 0.5/million/year |
| Sinonasal | 0.5/million/year |
| Anorectal | 0.4/million/year |
| Oral | 0.2/million/year |
Taken and modified from Micu E. J Eur Acad Dermatol Venereol. 2011;25(12):1444-9.
Solar radiation is the stimulus that causes the changes necessary for malignant transformation in the case of CM; in the case of anal melanoma, the causes are unknown. Melanin synthesis is the primary function of melanocytes; their role in mucosal areas is mainly characterized by antioxidant and adjuvant activity in the local immune response12.
Malignant transformation in anorectal areas may be related to environmental and genetic factors, oxidative stress, immunosuppression, or viral infections13, and human immunodeficiency virus (HIV) infection is considered an associated risk factor14. Another hypothesis is hormonal, possibly due to the participation of estrogens in the pathogenesis of melanoma, increasing the number of melanocytes and their melanin content15. These lesions may be an incidental finding during an endoscopic study or the result of histological analysis of a rectal polyp or hemorrhoidectomy16.
Nodal involvement is found in approximately 60% of patients at diagnosis and distant metastases in 30% of cases17. The diagnosis should be suspected when observing a pigmented lesion in the anal canal, although 10% to 30% of these neoplasms are amelanotic18. An exhaustive search should be performed to identify malignant skin lesions with the potential to develop GI tract metastases to differentiate and clarify the diagnosis of the primary lesion19.
The clinical manifestations can be very varied; the most frequent symptoms of this neoplasia are rectal bleeding, proctalgia, pruritus, tenesmus, sensation of anal mass, or alteration of intestinal habit; the lesion can protrude through the anal sphincter either during defecation or with the Valsalva maneuver, becoming a reason for consultation20. In a recent series, only 0.8% of patients manifested bleeding symptoms21. Regarding the endoscopic findings, the manifestation may be a melanotic polypoid lesion, as occurred in this case, or a mass that simulates colorectal cancer22. Histologically, the melanin pigment is characteristic, although immunohistochemistry with positivity for HMB-45 and S-100 protein is much more specific23.
Treatment
Surgery is the most effective treatment for PAM if proper staging is performed. Contrast-enhanced magnetic resonance imaging (MRI) of the abdomen and pelvis allows us to clarify the degree of invasion24. PAM has an aggressive behavior; most patients have metastases at the time of diagnosis, mainly to the lungs25. Local resection (LR) has greater immediate benefits for the patient, such as early recovery, shorter hospital stays, and minimal impact on intestinal function. Abdominoperineal resection (APR) offers better disease-free survival and greater locoregional control26. Neither of these two techniques is a definitive cure; APR has given fewer recurrences than LR (29% versus 58%)27. The role of lymphadenectomy in surgical treatment is controversial26. Bilateral inguinal lymphadenectomy in patients with PAM without palpable lymph nodes increases the risk of complications without improvement in survival28. Control of local primary disease can be achieved with adjuvant radiotherapy after surgical resection29. Non-surgical treatment of PAM includes the administration of chemotherapy and radiotherapy. Moozar et al. evaluated the usefulness of radiotherapy for palliative purposes in a series of patients with PAM, noting an improvement in survival (16 months versus five months) compared to patients who underwent surgery alone30.
Regarding systemic therapies, there is currently no consensus on the most appropriate treatment for this type of melanoma. Some protocols, previously aimed at patients with CM, have been studied in the context of MM, including PAM31. A multicenter case-control study evaluating the effect of a four-drug combination known as the Dartmouth regimen (dacarbazine, cisplatin, carmustine, and tamoxifen) versus dacarbazine found a better response rate (19% vs. 10%)32. Singhal et al. reported on the efficacy of taxanes and showed a median overall survival of 11 months33.
Follow-up
There is no clarity regarding how follow-up should be performed after treatment of melanoma with primary rectal involvement. Its approach is based on the extrapolation of patients with CM34. A retrospective study that included 81 patients described the most frequent locations of metastases, regardless of the primary site of the disease, and reported extension to the liver (57%), lungs (41%), lymph nodes (38%), soft tissues (22%), bone (12%), and the central nervous system (7%). With these data, the best follow-up option likely includes brain, chest, and abdominopelvic CT. Regarding endoscopic follow-up, the surveillance intervals are not defined; some referral centers recommend following closely (every three months) during the first year and then a colonoscopy every six months35.
Conclusion
PAM is a rare malignant neoplasm that poses a diagnostic challenge. This tumor is characterized by aggressive behavior due to biological differences in the melanocytes in this anatomical area compared to other locations. Factors such as inadequate discernment of endoscopic findings, which are confused with benign pathologies such as hemorrhoidal disease, provide a poor short-term prognosis. Due to its low incidence, few studies report what the best therapeutic and surveillance strategy is; most data are extrapolations from CM. The survival of patients depends on the stage at the time of diagnosis. In this case, the patient underwent local resection and was referred to the oncology service. Therefore, it is deemed essential that gastroenterologists become familiar with this type of lesion, which will allow a timely diagnosis and adequate treatment.











 text in
text in