Introduction
Achieving an optimal colonoscopy necessitates adhering to quality criteria, among which proper preparation stands paramount. A variety of preparation methods incorporating different pharmacological products, dietary plans, and timings have been explored. In the realm of educational strategies, modalities such as videos, clips, or apps have emerged as cost-effective and user-friendly tools for disseminating health-related knowledge.
Conventionally, colonoscopy preparation instructions are printed and handed to patients during their medical consultations, with instances where these guidelines are delivered by nursing or secretarial staff. Although straightforward, this approach has been associated with a 10% to 30% incidence of inadequately prepared patients.
This study aims to assess whether supplementing printed colonoscopy preparation instructions with an educational video can enhance preparation quality as gauged by the Boston scale and, consequently, improve the detection of colon adenomas. Such research is pioneering within the Colombian context.
Colonoscopy stands as the cornerstone for colon cancer prevention and diagnosis1. Its efficacy, efficiency, and effectiveness pivot on thorough preparation, making the patient’s comprehension of preparation instructions crucial. Conversely, inadequate preparation can lead to increased time consumption, the need for repeat colonoscopies, missed lesion detection, and heightened complication risks2, thereby escalating healthcare costs and burdening the health system’s economy3-5. Factors contributing to insufficient preparation, as identified in literature, include the patient’s low socioeconomic status, limited education, chronic constipation, antidepressant use, male gender, afternoon colonoscopy appointments, and improper preparation consumption6. Often, such inadequacies are attributed to the patient’s poor understanding of the preparation process and suboptimal guidance from healthcare personnel.
Pedagogical videos, a facet of audiovisual education, fall under the broader umbrella of e-health. Unlike traditional educational strategies such as illustrations and text, videos offer a unidirectional approach that potentially enhances understanding by combining visual imagery with narration. These can be disseminated via computers, smartphones, or hosted on widely accessible internet platforms like YouTube, offering patients easy access7-9.
While the use of these devices as a tool for improving colonoscopy preparation is on the rise, the body of literature on their utility remains relatively sparse. Research has shown that educational videos can enhance the understanding of the colonoscopy preparation process, thereby improving its quality10,11. Furthermore, other studies have indicated a reduction in the necessity for repeat colonoscopies due to inadequate preparation, as well as a notable increase in patient satisfaction12. However, a more recent investigation focusing on an educational video about dietary restrictions did not observe any improvement in preparation quality when compared to a control group receiving standard education13. These findings suggest that educational or instructional videos are cost-effective, risk-free, repeatable, intuitive, and understandable for patients. Nonetheless, a conclusive verdict has yet to be reached. Challenges such as difficulties in accessing internet videos have been noted, and it has been proposed that younger patients may engage more frequently and easily with video content than older patients, who might find access and availability more challenging compared to printed materials. Another study employing the Boston scale across four groups demonstrated that participants receiving both written and visual instructions achieved significantly better outcomes than those who were provided with only one form of instruction14.
In conclusion, while evidence supports the notion that educational videos can enhance the quality of colonoscopy preparation, further research is warranted to solidify this claim, allowing for the acquisition of more objective knowledge and the formulation of clearer recommendations.
To this end, a 9-minute educational video was crafted to elucidate the nature of colonoscopy, including its indications, utility, benefits, and risks, with a particular emphasis on the preparation process as delineated by clear instructions tailored to the timing of the procedure. This video was made available on the universal platform YouTube, accessible via the following link: https://www.youtube.com/watch?v=P-9-0WwRgqo.
Materials and methods
Participants were enlisted from two gastroenterology specialty clinics renowned for conducting outpatient consultations and scheduling patients for colonoscopies, which are carried out in the digestive endoscopy units of the clinics on an outpatient basis. The sample size and selection criteria were determined using EPIDAT 4.2, focusing on patients older than 18 years, with an indication for colonoscopy, who had not undergone the procedure in the past five years. Exclusion criteria included patients with prior surgeries affecting the colon or those contraindicated for conventional colonoscopy preparation.
The sample size was calculated to ensure a 95% confidence interval (CI) and a 90% power, resulting in a minimum required population of 22 patients per group.
Instrument Measures
The Boston score15, a numerical scale ranging from 0 to 9, assesses the quality of intestinal preparation following the endoscopist’s cleaning maneuvers. It is defined as follows:
0: The colon segment is unprepared, with its mucosa obscured by solid feces that cannot be cleansed.
1: Partial visibility of the mucosa in the colon segment is achieved, though other areas remain poorly visible due to the presence of residual fecal staining or opaque liquid.
2: Minimal residual staining, with small fecal fragments or opaque liquid present, yet the mucosa of the colon segment is predominantly visible.
3: The entire mucosa of the colon segment is clearly visible, free from any residual staining, fecal fragments, or opaque liquid15.
Each region of the colon is assigned a segment score from 0 to 3, with these segment scores aggregating to a total score ranging from 0 to 9. Thus, a score of 9 represents an impeccably clean colon, while a score of 0 indicates a colon that is inadequately prepared15.
Procedure
Randomization and Masking
The study took place from December 2018 to March 2019. Eligible patients, after meeting the inclusion criteria, were briefed on the research details. Upon agreement, they signed an informed consent form. Subsequently, they were directed to the clinic’s administrative assistant to schedule their colonoscopy appointment. The assistant then provided a sealed envelope, which was marked with either an even or odd number following a pre-established randomization table, containing their assigned preparation instructions.
For the even-numbered group, the sealed envelope included printed instructions alongside the URLs for instructional videos, accompanied by detailed guidance on how to access these resources via computers or smartphones through Google or YouTube. Conversely, the control group received a sealed envelope containing only the printed instructions, remaining unaware of any video’s existence.
Colon Preparation
The study employed a commercial low-volume preparation consisting of two commercial bottles of sodium sulfate, magnesium sulfate, and potassium sulfate; each containing 176 mL of the solution. All participants received identical quantities and printed instructions tailored to their scheduled procedure time. Following best practice recommendations, participants were advised to commence an exclusive clear liquid diet 24 hours prior to their procedure. Morning appointments required the consumption of the first bottle between 9 and 10 AM the day preceding the procedure, and the second bottle between 9 and 11 PM that evening. Following each bottle, patients were instructed to drink an additional two 250 mL glasses of water. Emphasis was placed on liquid fasting (as solid food intake was prohibited 24 hours before the exam) starting 6 hours before the examination, in line with the anesthesiology team’s recommendations for sedation16.
For afternoon appointments, a clear liquid diet was prescribed starting 24 hours prior, with the first bottle to be taken between 8 PM and 10 PM the night before, and the second bottle between 6 AM and 7 AM on the day of the examination. A 6-hour liquid fast was also mandated before the procedure.
Colonoscopy
On their scheduled date, patients arrived at the designated endoscopy unit with their received preparation and signed the informed consent for the colonoscopy. An anesthesiologist administered sedation to all patients. The colonoscopy findings and the Boston score for preparation were documented in the colonoscopy’s final report.
Intervention
The implemented intervention was the viewing of an instructional video, conceptualized and produced by the study’s principal researcher. The video outlined the essentials of colonoscopy, including its benefits, indications, risks, and detailed dietary and preparation instructions. Running for nine minutes, the video was made available on YouTube for easy access. Released several months prior to the study, it was part of initial pilot tests to assess viewing accessibility. Despite mentioning both high and low volume preparations, specific instructions were provided for the consumption of the study’s chosen solution containing sodium sulfate, magnesium sulfate, and potassium sulfate.
The video can be accessed at the following URL: https://www.youtube.com/watch?v=P-9-0WwRgqo.
Outcomes
The primary aim of this study was to evaluate the quality of colonoscopy preparation using the Boston score. A secondary aim focused on the adenoma detection rate within the colon. The methodology encompassed several steps:
The initial patient consultation took place at the principal author’s gastroenterology clinic.
Eligibility was determined by satisfying the inclusion criteria and excluding any patients based on the exclusion criteria identified through clinical history review.
Patients were briefed on the study’s objectives and procedures verbally.
Upon agreement, participants signed an informed consent form.
Essential data such as weight, age, sex, and the indication for the colonoscopy were recorded in an MS Excel database.
Participants were then directed to the administrative office to receive their scheduled appointment and a sealed envelope containing their assigned preparation instructions. This envelope was allocated based on randomization to either receive written instructions complemented by video directions or written instructions alone.
The colonoscopy was performed on the assigned date under sedation, managed by an anesthesiologist, followed by a report detailing any polyps found for further histopathological analysis.
A follow-up consultation was conducted to ascertain if the participant had viewed the video, with the administrative office confirming the randomization details, envelope allocation, colonoscopy report, and histopathological findings.
Statistical Analysis
The statistical analysis and figures were performed using EPIDAT 4.2 software. A goodness-of-fit test, specifically the Shapiro-Francia test, was employed to assess distribution type and homoscedasticity, evaluating equality of variances through Levene’s test. Further inferential analysis compared the mean Boston scores between two independent populations, utilizing the Student’s t-test due to the presence of homoscedasticity and a normal distribution pattern.
An additional inferential analysis compared independent proportions, focusing on the presence of adenomatous polyps between the groups.
Results
The study included 142 patients, divided into 73 in the video group and 69 in the control group, comprising 92 females (64.8%) and 50 males (35.2%). Age ranged from a minimum of 30 years to a maximum of 84 years.
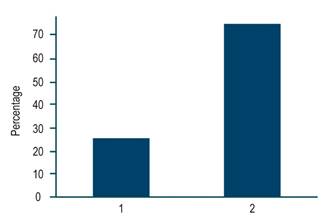
Overall, patients achieved a mean Boston score of 7.5 (standard deviation [SD]: 1.32), with a median score of 7.5. The video group exhibited an average Boston score of 8.16 (SD: 1.6), while the non-video group had an average of -6.75 (SD: -1.2). When analyzed using EPIDAT 4.2 software, an inference-based comparison with the means of two independent populations yielded a highly significant difference of (p -0.0001; t: 4.6) (Figure 1).
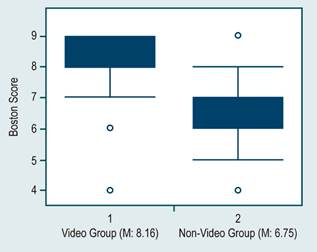
Author’s own research.
Figure 1 Superior Quality of Colonoscopy Preparation in the Video Group Compared to the Non-Video Group (p < 0.00001).
The average comparison computation was conducted for Boston scores within each segment separately, resulting in the following outcomes: right colon (2.6 versus 1.9; p < 0.001), transverse colon (2.7 versus 2.3; p < 0.0001), and left colon (2.8 versus 2.5; p < 0.0001). A notably significant difference was observed across each segment individually.
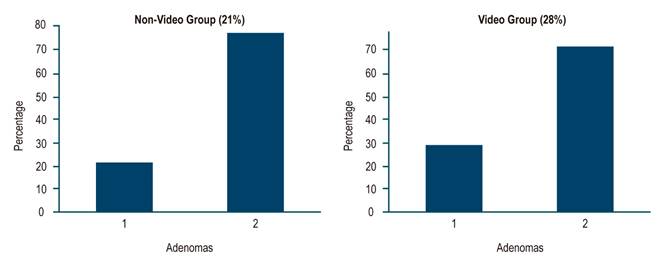
Regarding polyp detection analysis based on video visualization, the findings were as follows: the adenomatous polyp detection rate for the overall group stood at 26% (36/106) (Figure 2).
Within the video-watching cohort, adenomatous polyps were identified in 28% (21/73), while in the non-video-watching group, they were detected in 21% (15/69) of cases (Figure 3). An inference analysis of population proportions, conducted using EPIDAT 4.2, revealed no statistically significant difference, with a p-value of 0.33.
Discussion
The recent years have witnessed a remarkable surge in the advancement of information and communication technologies, a trend that has seen broad adoption across general education, academia, and learning. In medicine, these technological tools are increasingly employed to achieve similar educational outcomes. The critical role of adequate colonoscopy preparation for the early detection of lesions is well established; thus, the impetus for this study was to ascertain whether supplementing printed instructions with an educational video could enhance the quality of colonoscopy preparation.
This study identified a highly significant increase in the mean Boston score for the group of patients who had access to the video. These results are notable as they underscore the efficacy of electronic resources in improving comprehension of colonoscopy preparation, likely owing to several factors:
Enhanced understanding of the importance and benefits of colonoscopy provided by the video content;
Increased time dedicated to patient consultation, which is often brief, allowing for the clarification of any uncertainties regarding the colonoscopy and its preparation process;
The ability to replay the video, which may bolster information retention;
The incorporation of auditory learning to complement visual information.
The study’s secondary aim examined potential disparities in adenoma detection rates; however, no differences were observed. This outcome may indicate an actual absence of variance or it might suggest the need for a larger sample size for more definitive results. One possible limitation of the study is that the patient population was predominantly from the upper-middle to high socioeconomic stratum, likely with better access to internet technologies, which could imply that the findings may not be universally applicable. Nonetheless, literature suggests that technological health tools can improve preparation quality across all socioeconomic levels.
A review of the scientific literature identified several existing articles on the subject, prompting a comparison of this study with prior findings across four distinct aspects. The first pertains to the use of objective scales for assessing intestinal preparation quality, crucial for accurate evaluation of the colonic mucosa and for ensuring neoplastic lesions or their precursors are not overlooked. Moreover, optimal preparation minimizes procedural time and reduces the likelihood of necessitating a repeat colonoscopy due to inadequate initial preparation. Various professional societies, including the American Society for Gastrointestinal Endoscopy (ASGE), endorse the inclusion of preparation quality in the procedural report as a quality metric. Previously, subjective descriptors such as “good”, “fair”, and “poor” were used, which did not distinguish between different colonic segments. Consequently, this study utilized the Boston preparation scale, which methodically assesses the three colon segments (ascending, transverse, and descending) as elucidated earlier15.
Concerning the second aspect, regarding the choice of medication for preparation, literature reveals various strategies and pharmacological agents utilized. While the current study does not aim to compare their effectiveness, it is essential to highlight prevailing recommendations based on diverse high-quality studies. These recommendations advocate for the adoption of split-dose regimens, regardless of the specific medication employed, administered as closely as feasible to the time of colonoscopy to facilitate safe sedation17,18.
Regarding the third aspect, concerning the use of educational, technological tools, several have been employed and evaluated. These educational strategies aim to enhance the quality of colon preparation and fall into three categories9,11,12,14,19-22:
The first includes instructive leaflets, visual aids featuring animations, and educational videos that simplify the preparation process23.
The second involves sending reminder text messages to patients’ phones to prompt preparation steps.
The third incorporates smartphone applications that aim to present preparation instructions in an easily digestible format.
For our investigation, we selected the first approach, deploying an educational video crafted by the lead researcher. This video addressed the most frequent inquiries patients present during medical consultations: the nature of a colonoscopy, its significance, the associated benefits, potential risks, and recommendations for optimal preparation.
The four aspect we must also examine is the parametric measures or designs employed across various studies in the literature, comparing our methodology with others regarding the aforementioned aspects.
A 2016 study featured in BMC Gastroenterol20 posed the question of whether an educational tool could enhance patient preparation for colonoscopy. Conducting a prospective randomized trial, it provided patients with periodic preparation instructions at a pre-colonoscopy visit. One group received additional educational intervention through a video the day before their procedure, while a control group did not. The video group demonstrated superior preparation. This study’s conclusion resonates with our own findings, asserting that educational videos are instrumental in facilitating proper colonoscopy preparation. However, it also notes differences such as using polyethylene glycol for preparation and utilizing the Ottawa score for outcome measurement.
Another expansive study published in the American Journal of Medicine12 in 2016 made an educational video publicly accessible online from 2010 to 2014. The study ensured patient engagement with the video through a unique code linked to their medical records. It included 2530 participants, with 1251 viewing the video and 1279 who did not. A multivariate analysis indicated a higher rate of adequate bowel preparation in the video group: 92% (84-96) versus 87% (76-93) (p < 0.01). The likelihood of requiring a repeat colonoscopy within three years was also less for video viewers: 3.3% compared to 6.6% who did not watch the video (p < 0.001). Though a cross-sectional descriptive study with a significant sample size, it intimates that providing educational videos for colonoscopy preparation not only augments the quality of preparation but might also decrease the frequency of repeat procedures over time.
An additional study from August 2018 in Medical Science Monitor24 detailed a prospective, randomized, controlled trial among outpatient colonoscopy patients. Randomly allocated into two groups (1:1 proportionally), one engaged with a preparatory video, while the control group did not. The research aimed to evaluate intestinal preparation quality using the Ottawa score and identify risk factors for inadequate preparation. Results indicated that the video group achieved better bowel preparation for colonoscopy (Ottawa < 6) than the control group (p < 0.001), with enhanced cleanliness in each colon segment. Identified risk factors for poor preparation included male gender, diabetes mellitus, and non-viewing of educational videos. Mirroring our study, this research underscores the importance of incorporating a technological tool such as an audiovisual video for preparation, differing from our approach in the application of the Ottawa preparation score.
Another study, published in Gastrointestinal Endoscopy in 201825, conducted a prospective, blinded, randomized controlled trial comparing various preparations, including polyethylene glycol with ascorbic acid and low-volume options such as sodium picosulfate with magnesium citrate. Participants were divided into two cohorts: one undergoing a smartphone reeducation strategy, comprising 139 individuals, and a control group with 144 individuals. The primary endpoint was assessed using the Boston Bowel Preparation Score (BBPS). Out of 283 subjects analyzed according to the protocol, the mean BBPS was higher in the smartphone reeducation group at 7.53 compared to 6.29, indicating that an alternative educational strategy to that used in our research can also be more user-friendly with the aid of a smartphone.
These investigations endorse the notion that leveraging technological education in colonoscopy preparation not only improves the quality of the preparation but also the colonoscopy’s efficiency, which is in line with our study’s outcomes. Nonetheless, there is a need for additional research to expand upon these findings, such as enlarging the sample size and undertaking multicenter studies that consider various population strata.
Conclusion
In summary, incorporating an educational video into conventional printed instructions markedly enhances the quality of colonoscopy preparation as measured by the Boston score, warranting its adoption as a routine technological strategy. Although an improvement in adenoma detection in the colon was observed with the addition of the video, this increase was not statistically significant, potentially due to an insufficient sample size. Thus, it is recommended that future research include larger, multicenter studies.











 texto em
texto em