Introduction
Gallbladder adenomyomatosis in the pediatric population represents a seldom-encountered condition. It is benign and acquired, with its etiology remaining elusive1. The condition is primarily characterized by either localized or diffuse epithelial proliferation, leading to mucosal invagination through an enlarged muscular layer. This process creates intramural diverticula or sinuous paths2, known as Rokitansky-Aschoff sinuses1. Despite its identification, much about adenomyomatosis, including its pathogenesis, associated risk factors, and surgical indications-particularly within a pediatric context-remains poorly understood2. In adults, it is detected in as many as 5% of cholecystectomy cases, yet the pediatric literature documents it far less frequently3.
Case presentation
We report the case of a 15-year-old female patient, weighing 42.5 kg with a height of 141 cm, resulting in a body mass index (BMI) of 21.4 kg/m2. She was admitted with a primary diagnosis of congenital scoliosis, specifically a hemivertebra at T11-12 level causing secondary spinal compression, and butterfly vertebrae spanning T5 to L3. The patient underwent a two-stage surgical procedure for the resection of the T11-12 hemivertebra and spinal instrumentation from T5 to L3. Following the second surgical intervention, she experienced nausea, abdominal pain and distension, and diarrheal bowel movements without the presence of mucus or blood, accompanied by reduced intestinal sounds.
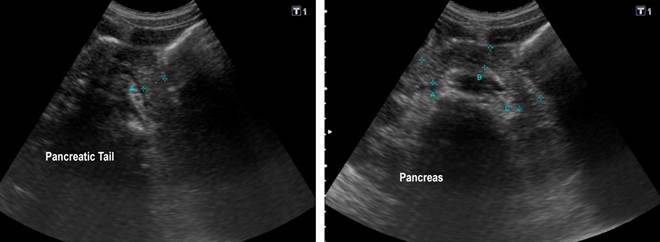
An abdominal ultrasound revealed focal thickening of the gallbladder walls, perivesicular fluid, ascites, and focal thickening of the pancreatic tail measuring up to 22 mm in diameter (Figure 1). Laboratory tests showed elevated levels of aspartate aminotransferase (AST) at 235 U/L, alanine aminotransferase (ALT) at 93 U/L, serum amylase at 104 U/L, γ-glutamyl transpeptidase (GGT) at 96 U/L, lipase at 813.4 U/L, and C-reactive protein (CRP) at 84.5 mg/dL, prompting the initiation of treatment for acute pancreatitis.
Source: Patient’s medical records.
Figure 1 Total Abdominal Ultrasound. The image reveals a localized thickening of the walls in the body and neck regions, accompanied by perivesicular fluid accumulation. The pancreas exhibits a focal thickening of the sac, measuring up to 22 mm in diameter.
Despite treatment, the patient’s condition did not improve, with continued severe abdominal pain and clinical deterioration. A contrast-enhanced abdominal CT scan was performed, identifying changes consistent with gallbladder adenomyomatosis, accompanied by perivesicular fluid and intestinal ileus (Figure 2). Given the worsening of her gallbladder’s condition, surgical intervention was deemed necessary. A laparoscopic examination revealed a gallbladder with thickened walls containing purulent material, identified as pyocholecyst, which was adhered to the duodenum.

Source: Patient’s medical records.
Figure 2 Contrast-Enhanced Computed Tomography (CT) Scan of the Abdomen. The arrow denotes the continued presence of findings indicative of gallbladder adenomyomatosis, accompanied by a mild increase in the anteroposterior diameter of the pancreatic tail and preserved peripancreatic fat with perivesicular augmentation.
Histopathological examination of the gallbladder wall disclosed extensive mucosal necrosis, severe transmural polymorphonuclear inflammatory infiltrates, Rokitansky-Aschoff sinuses, and muscular hypertrophy, with necrotic material found within the lumen. The patient experienced no postoperative complications, demonstrated significant improvement, and was subsequently discharged from the institution.
Discussion
Gallbladder adenomyomatosis, known by various names historically, is currently the accepted term for this condition, first identified by Jutras and colleagues in 19603. This disease represents an anatomoclinical challenge4, with its precise diagnosis proving to be exceptionally difficult. It is a relatively rare gallbladder pathology in children, associated with cholecystitis and cholelithiasis3,5. To date, adenomyomatosis remains a markedly uncommon ailment, with unknown pathogenesis and unclear surgical indications, especially within the pediatric demographic. In the adult population, it is detected in 5% of cholecystectomy specimens3,6. As of 2020, merely ten cases have been documented in children3.
Adenomyomatosis is characterized by epithelial proliferation alongside muscular layer hypertrophy, leading to the creation of fistulous tracts known as Rokitansky-Aschoff sinuses3,6. The adenomyomas formed are benign leiomyomatous growths, distinguished by proliferation of the superficial epithelium and its invagination deep into the muscular layer4. The condition exhibits a predilection for females over males, with a ratio of 3:1, aligning with the demographic details of our adolescent patient1,7.
The disease can induce changes in the metaplastic epithelium (including intestinal and pyloric metaplasia), inflammation, and fibrosis. While these alterations are not deemed potentially premalignant, the development of dysplasia, in situ, or invasive carcinoma within adenomyomatosis epithelium can occur, potentially progressing to carcinoma. This progression is thought to be more closely associated with lithiasis, chronic inflammation, and metaplastic changes rather than with adenomyomatosis itself, highlighting the recognized link between lithiasis and gallbladder cancer8.
Adenomyomatosis can manifest in the gallbladder through four principal patterns: localized, segmental, annular, and diffuse5, all of which spare the serosa1. The most common is the localized pattern, typically presenting as focal thickening most often affecting the gallbladder fundus region5. This pattern may also feature an umbilicated nodule in the fundus, referred to as an adenomioma9. Conversely, diffuse adenomyomatosis typically affects the gallbladder body, characterized by a total circumferential thickening of the wall, resembling an “hourglass”. In our case, ultrasound imaging revealed concentric wall thickening up to 5 mm towards the gallbladder neck.
Clinically, adenomyomatosis symptoms, when present, often mimic those of cholelithiasis, such as colic pain, or result from main bile duct obstruction; in some instances, the presentation may resemble acute pancreatitis4. Our patient experienced a significant elevation in lipase (1408 U/L) and amylase (307 U/L) levels, with subsequent improvement following cholecystectomy. Generally, the pediatric population predominantly presents with acute, nonspecific, and recurrent abdominal pain, occasionally accompanied by vomiting and fever3. These symptoms, specifically acute, nonspecific abdominal pain and nausea, were observed in our patient.
In numerous instances, the diagnosis of gallbladder adenomyomatosis is incidentally made through an ultrasound or abdominal computed tomography (CT) scan, originally intended to explore other medical conditions3. The hallmark findings typically include either focal or diffuse thickening of the gallbladder wall, the presence of small intramural diverticula that may encapsulate bile within small, multiple, and anechoic cystic spaces, and intramural echogenic foci when containing cholesterol collections or biliary sludge. These foci may or may not be associated with acoustic shadowing, or exhibit reverberation or twinkling artifacts on color Doppler ultrasound1. In the case we present, imaging revealed focal thickening of the gallbladder wall and the pancreas tail, associated with perivesicular fluid as notable findings.
Moreover, magnetic resonance imaging (MRI) studies highlight that Rokitansky-Aschoff sinuses manifest as a “pearl necklace” sign-multiple round spaces with hyperintense signals in T2-weighted sequences, demonstrating a 92% specificity for gallbladder adenomyomatosis10. Typically, ultrasound and MRI provide sufficient diagnostic clarity for most patients; however, a definitive diagnosis necessitates histopathological examination of the specimen. This analysis commonly details the gallbladder segmented into various parts by septa made of columnar epithelium, connective tissue, and smooth muscle fibers11. It further notes mucosal invagination extending through the subepithelial fibromuscular tissue, the presence of Rokitansky-Aschoff sinuses, and occasionally, associated smooth muscle hyperplasia. The detection of smooth muscle tissue underpins the congenital nature of this condition. Inside the Rokitansky-Aschoff sinuses, one might find thick bile, mucus, and calculi, inducing inflammatory, fibrotic, and metaplastic changes (including intestinal and pyloric gland metaplasia)1. On ultrasound, these may appear as echo-poor intramural cystic structures; containing sludge, they turn echogenic, potentially generating distal acoustic shadowing or ring-down (“comet tail”) artifacts2,12. While these findings are not inherently abnormal, they are typically linked with adenomyomatosis and cholecystitis1.
Surgical intervention is not deemed necessary for asymptomatic patients. However, symptomatic individuals may warrant a cholecystectomy, preferably performed laparoscopically11. Despite the absence of reported cases of carcinoma in pediatric patients with gallbladder adenomyomatosis in the current literature, cholecystectomy remains a viable option for those exhibiting symptoms, though the optimal timing for such a procedure remains unclear3.
Gallbladder adenomyomatosis is notably rare, especially in the pediatric population. Its diagnosis fundamentally relies on the identification of Rokitansky-Aschoff sinuses, with ultrasound serving as the diagnostic tool of choice13. The advancement of imaging techniques, combined with physician expertise, has led to an increase in the detection of this condition, suggesting that reports and diagnoses of adenomyomatosis may continue to rise. Although the pathogenesis of adenomyomatosis remains incompletely understood, it is associated with gallstones and chronic inflammatory diseases4.











 text in
text in 



