Introduction
The primary method for managing both malignant and benign biliary obstructions is through the decompression of the bile duct via endoscopic retrograde cholangiopancreatography (ERCP) with stent placement. This approach is successful in a significant majority of cases, demonstrating a failure rate of only 5%-7%1. However, challenges arise when cannulation of the ampulla of Vater is rendered impossible due to anatomical alterations, such as those caused by neoplastic involvement. In recent years, endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as a viable alternative to the traditional percutaneous or surgical approaches2.
Endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) has been acknowledged as a secondary strategy for biliary drainage in instances where endoscopic retrograde cholangiopancreatography is unsuccessful or when duodenal cannulation is not feasible. It boasts a clinical success rate of up to 93% and reports a 30-day post-procedure morbidity rate of 18%, with the most frequent complication being the recurrent occlusion of the biliary stent. The mortality rate associated with this procedure stands at 5%3.
The option of percutaneous transhepatic biliary drainage (PTBD) is now considered a tertiary choice, given its potential morbidity rate of up to 33%. The adverse events associated with this method can include catheter dislodgement, recurrent infections, acute cholangitis, bleeding, bile leaks, pneumothorax, and aesthetic concerns due to the requirement for external drainage, all of which can significantly detract from the quality of life of the patients4,5. In our review of meta-analyses and systematic reviews, despite their inherent heterogeneity, a consistent conclusion is drawn across the board: EUS-BD is linked with a higher rate of clinical success, fewer post-procedure adverse events, and a reduced need for reinterventions when compared to PTBD1,6. This paper presents three case studies that highlight our experiences with performing hepaticogastrostomy in Colombia.
Case 1
We report the case of a 75-year-old female patient who experienced a fall from standing height and was subsequently admitted to the emergency department. There, she was diagnosed with a right hip fracture. Incidentally, radiological studies revealed a neoplasm located in the head of the pancreas. During her clinical review, she reported a significant weight loss of 10 kg over the past two months and exhibited symptoms including jaundice, acholia, and dark urine approximately one week prior to admission. Her medical history was notable for basal cell carcinoma, an anxiety-depressive disorder diagnosed 13 years ago, atrial fibrillation identified thee years ago, and treated melanoma. A biliopancreatic endoscopic ultrasound was conducted, revealing a neoplasm in the head of the pancreas measuring 22 x 24 mm with irregular borders, heterogeneous hypoechoic appearance, and no vascular involvement. However, the lesion compromised the distal third of the bile duct, 2 mm from the duct of Wirsung, accompanied by a bile duct dilation of 17 mm. A fine needle biopsy of the mass indicated cells with epithelial atypia suggestive of adenocarcinoma, characterized by variability in nuclear size, irregular contours, hyperchromatism, clumped chromatin, and loss of polarity.
Upon her admission, the patient presented with generalized jaundice, corroborated by laboratory findings including leukocyte count of 7200, neutrophils at 5200, lymphocytes at 1300, hemoglobin at 9.8, total bilirubin at 12.8, direct bilirubin at 7.8, aspartate aminotransferase (AST) at 89, alanine aminotransferase (ALT) at 77, and alkaline phosphatase at 473. Further diagnostic work-up with magnetic resonance imaging and tomography of the chest and abdomen corroborated the endoscopic ultrasound (UES) findings and identified multiple hepatic lesions suggestive of a metastatic pattern. Given the elevated bilirubin levels, an ERCP was attempted but failed due to a laterally displaced and deformed ampulla of Vater, which precluded bile duct access, and a duodenal wall with a neoplastic infiltrative appearance at the level of the second portion. The patient was informed about the necessity of percutaneous transhepatic biliary drainage and the placement of an external drainage guide. However, she adamantly refused this approach, expressing concerns that it would exacerbate her anxiety and depression. Consequently, a hepaticogastrostomy was proposed as an alternative, which the patient understood and accepted. The procedure was successfully performed, and notable improvements were observed, with bilirubin levels reducing to 5 mg/dL at 48 hours and further decreasing to 2 mg/dL by 72 hours post-procedure. The patient was subsequently discharged, reporting no pain, weakness, fever, or discomfort during her immediate and subsequent postoperative recovery.
Case 2
A 56-year-old female patient with a medical history of type 2 diabetes, hypertension, hypothyroidism, and gastroparesis presented with a three-year history of abdominal pain. The pain, predominantly located in the epigastrium, radiated to the dorsal region in a band-like pattern. The most recent episode was characterized by high intensity, accompanied by dark urine and generalized itching. Initial evaluation at another institution, through magnetic resonance cholangiopancreatography, revealed a lesion in the head of the pancreas causing biliary obstruction and pancreatic duct dilation. A plastic stent was placed for biliary drainage, after which the patient was referred to our center for hepatobiliary surgery evaluation.
Upon her admission, a biliopancreatic endoscopic ultrasound was conducted with biopsy sampling. Pathology confirmed the presence of adenocarcinoma, leading to the initiation of neoadjuvant chemotherapy and radiotherapy. One month following treatment initiation, the patient was admitted via emergency services due to a resurgence of right hypochondrial abdominal pain that radiated to the lumbar region, marked by increased intensity, dark urine, pale stools, and hand itching. A subsequent magnetic resonance cholangiopancreatography demonstrated a posterior solid-component pancreatic lesion, which resulted in amputation of the bile and main pancreatic ducts and significant dilation of the intra- and extrahepatic biliary pathways, likely due to stent dysfunction. Laboratory analyses revealed elevated liver enzymes and bilirubin levels (AST: 47, ALT: 328, alkaline phosphatase: 414, total bilirubin: 4.87, direct bilirubin: 3.6). A follow-up ERCP allowed for the removal of the initial plastic stent and placement of a self-expanding metal stent, leading to improved laboratory results the subsequent day. An abdominal MRI indicated a 30% reduction in lesion size compared to prior imaging, prompting patient discharge.
The patient presented again one month later with symptoms indicative of biliary obstruction and episodes of fever. During this visit, ERCP revealed biliary stent migration, necessitating the placement of a new self-expanding metal biliary stent. Post-procedure, the patient showed favorable progress and was discharged. Seven months later, a planned right hepatic lesion ablation was successfully executed by an interventional radiologist. The patient was scheduled for a follow-up ERCP two months later for stent exchange. However, this ERCP was unsuccessful due to an inability to navigate the duodenum to the second portion because of stenosis. The patient was advised a soft diet and subsequently discharged.
Shortly thereafter, the patient was admitted with a new onset of biliary and intestinal obstruction. Surgical evaluation led to the decision to perform a gastrojejunostomy, which was executed a week later. Post-operatively, the patient demonstrated clinical improvement and a reduction in liver enzymes, warranting discharge. However, two months later, the patient returned with biliary obstruction. An attempt at endoscopic biliary diversion was thwarted by ascitic fluid, which hindered proper visualization. Following a paracentesis, the procedure was rescheduled, and a successful hepaticogastrostomy was performed three days later, leading to symptom relief, a decrease in liver enzymes, and patient discharge.
Over the subsequent month, the patient made several visits to the emergency department due to pain, abdominal distension from ascites, and fever episodes related to febrile neutropenia, but without evidence of biliary obstruction. Unfortunately, the patient succumbed to the natural progression of her tumor four months later.
Case 3
A 73-year-old female patient presented with a one-week history of pain that originated in the left flank. Initially moderate in intensity, the pain progressively intensified and later radiated to the epigastrium and dorsally in a band-like fashion. The patient also reported dark urine and subjective weight loss over the past six months, with no episodes of nausea, vomiting, pale stools, fever, or other symptoms. A diagnosis of obstructive biliary syndrome was established following the identification of a mass in the head of the pancreas via abdominal angiotomography. This mass was consistent with neoplastic characteristics, displaying necrotic points and causing dilation of the biliary tract with involvement of the portal vein and superior mesenteric artery. Management commenced with piperacillin-tazobactam and analgesia, resulting in the patient’s stable discharge.
The patient’s medical history was notable for type 2 diabetes mellitus not requiring insulin, hypothyroidism, hypertension, and recurrent urinary tract infections secondary to urolithiasis. She had also experienced multiple episodes of acute pancreatitis, the most recent of which occurred six years prior and was managed with ERCP and pancreatic stent placement. A pancreatic pseudocyst had developed as a complication of pancreatitis. Additionally, she had undergone a laparoscopic cholecystectomy 30 years previously.
Upon this admission, the patient was hemodynamically stable and anicteric, exhibiting no signs of peritoneal irritation. Laboratory findings included leukocytes at 10,200, with 84% (8,600) neutrophils and 6.4% (600) lymphocytes, 6.4% (10.2) hemoglobin, hematocrit at 30%, platelets at 343,000, erythrocyte sedimentation rate at 122, sodium at 135.49, potassium at 3.13, creatinine at 0.50, AST at 76, ALT at 44, total bilirubin at 8.8, direct bilirubin at 5.11, indirect bilirubin at 3.69, alkaline phosphatase at 1193, and lipase at 7.4. Further investigation through total abdominal ultrasound revealed a large mass with neoplastic appearance affecting the head of the pancreas, causing local compressive effects with secondary dilation of the intra- and extrahepatic biliary tract, warranting further characterization by contrast-enhanced magnetic resonance imaging.
Subsequent ERCP and biliopancreatic ultrasound identified an impassable duodenal stenosis, obstructing progression to the second portion of the duodenum, with the duodenal mucosa presenting an infiltrative neoplastic appearance. Despite the failed ERCP due to duodenal obstruction, the patient’s general condition improved during her hospital stay, with total bilirubin levels decreasing to 2.08 and alkaline phosphatase to 464. A successful hepaticogastrostomy guided by biliopancreatic ultrasonography was then performed.
Post-procedure, the patient’s hepatic profile continued to improve, with total bilirubin reaching 2, direct bilirubin at 0.94, and alkaline phosphatase at 298. She tolerated oral intake, experienced normal bowel transit, and reported no abdominal pain, facilitating her discharge.
Pathology results later revealed a fibrohistiocytic reaction, active chronic inflammation, and epithelial fragments without evidence of high-grade dysplasia or malignancy. A subsequent multidisciplinary meeting concluded the patient was suffering from chronic pancreatitis, for which she was provided medical management. Follow-up visits over the next eight months showed the patient continued to make good clinical progress.
Discussion
In the cases we presented (Table 1), each patient was female with an average age of 68 years. The pathologies involved tumors in the head of the pancreas, with associated bile duct involvement. One patient had chronic pancreatitis with a tumor that simulated an adenocarcinoma. In every case, stents were employed preemptively until cannulation of the ampulla of Vater could be accomplished. Notably, no complications occurred, and survival and follow-up were consistent across all cases for up to three months. Remarkably, the patient with chronic pancreatitis has not experienced any complications to date, suggesting good long-term stent maintenance-a promising indicator for future studies on stent durability.
Table 1 Patients with Tumors Located in the Head of the Pancreas with Bile Duct Involvement
| Age | Sex | Type of Pathology | Location | Type of Stenosis | Prior Stent | Complications | Survival at Three Months |
|---|---|---|---|---|---|---|---|
| 75 | Female | Adenocarcinoma | Head of the pancreas | Distal bile duct | Yes | No | Yes |
| 73 | Female | Solid pseudotumor in chronic pancreatitis | Head and uncinate process of the pancreas | Distal bile duct | Yes | No | Yes |
| 56 | Female | Adenocarcinoma | Head of the pancreas | Middle third of the bile duct and main pancreatic duct | Yes | No | Yes |
Author’s own research.
It is evident that the utilization of EUS-HGS primarily occurs among palliative care patients, deemed ineligible for prospective treatments and characterized by a limited life expectancy. In such cases, the preference for employing this technique is justified by its demonstrated enhancement of quality of life and its capacity to mitigate complications arising from percutaneous drainage6. Each of our patients underwent a comprehensive explanation of the procedure and were provided the option between PTBD and EUS-HGS. Without exception, they conveyed the psychological burden associated with bearing an external catheter, underscoring the significance of their perspective within the clinical realm of such patients, crucial for alleviating the psychological strain accompanying terminal cancer. In light of this consideration, we advocate for regarding patient opinion as a decisive factor favoring the adoption of this technique over alternatives. Moreover, we posit that, given current trends, all minimally invasive procedures and natural orifice techniques should supersede their conventional counterparts.
In all cases, we employed a GIOBOR stent, deemed optimal for the procedure due to its design features. Notably, it boasts a 70% covered section, effectively preventing bile leakage between the left hepatic duct and the stomach, while also exhibiting a flexible configuration adaptable to the curved trajectory from the stomach to the left hepatic duct, accommodating certain degrees of movement. Furthermore, its 30% uncovered section serves to avert obstruction of lateral branches in the left hepatic duct and migration into the stomach. Additionally, the stent incorporates an anti-migration widened end, strategically positioned beyond the stomach wall to forestall migration towards the left intrahepatic duct. These attributes are illustrated in Figures 1, 2, and 3 7.
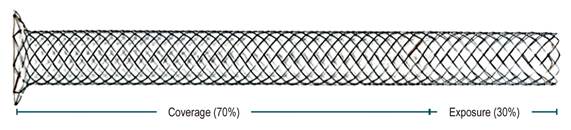
Source: TaeWoong Medical. [Internet]. Niti-S & ComVi Biliary Stent. User’s Manual.
Figure 1 Distribution of the percentage of coverage and exposure.
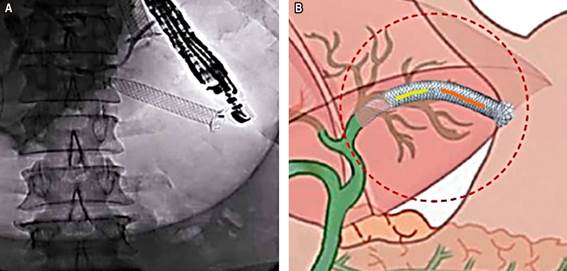
Source: Author’s File.
Figure 2 A. Fluoroscopic view showing the location of the hepaticogastrostomy stent. B. Illustration of the stent placement highlighting the angulation and adaptation of the GIOBOR stent.
Conclusion
EUS-HGS is asserted as the technique of choice subsequent to an unsuccessful ERCP and when anatomical alterations or cannulation challenges present. This approach is associated with lower complication rates and mortality in comparison to similar procedures. It benefits from the availability of a specialized stent designed for the specific anatomy addressed, and its placement is deemed to be at a reduced risk of tumor overgrowth relative to bile duct-level placement. Its apparent compatibility with gastrointestinal physiology is evidenced by the absence of complications or need for stent replacement across our series, extending up to eight months. The GIOBOR stent, given its described attributes, is advocated as the preferred option for this intervention.











 text in
text in 




