Introduction
Choledochal cysts, also known as bile duct cysts, are congenital abnormalities characterized by the dilation of the intrahepatic or extrahepatic biliary ducts. They account for 1% of hepatic anomalies with estimated incidences ranging from 1 in 100,000 to 1 in 150,000 in Western populations and as frequent as 1 in 1,000 in certain Asian populations1,2, with a female predominance3. Although typically identified in childhood, accounting for approximately 25% of cases4, the incidence in adults is on the rise5,6.
The underlying cause of persistent choledochal cysts is unclear, but the most widely accepted hypothesis is that proposed by Babbit in 19697. This theory posits an anomalous junction of the pancreatic duct and the bile duct, which merge 1.5-4 cm distal to the sphincter of Oddi, forming a “common channel” that permits the reflux of pancreatic secretions into the biliary duct, a condition known as “pancreatobiliary reflux”. The resulting activation of pancreatic enzymes leads to inflammation and thickening of the bile duct walls, prompting dilation. This is supported by reports of elevated amylase in the bile in patients with this conditions compared to those without it8,9. Babbit’s theory accounts for 50%-80% of cases since not every patient with this long common channel develops a cyst; likewise, not every patient with a choledochal cyst has such a channel10. Alternative theories propose the absence of ganglion cells, dysfunction of the sphincter of Oddi, and a weakened bile duct wall11,12.
In 1959, Alonso-Lej13 categorized choledochal cysts; subsequently, Todani and colleagues14 revised this classification, which is now widely adopted. Five types of choledochal cysts are delineated based on location and morphology (Table 1)15. Clinical presentation varies according to age groups.
Table 1 Todani’s Classification of Choledochal Cysts and Their Frequency.
| Type | Description | Frequency |
|---|---|---|
| IB |
Isolated dilation of the extrahepatic bile duct IA: Cystic IB: Saccular IC: Fusiform |
80%-90% |
| II | Diverticulum | 2% |
| III | Choledochocele affecting the intraduodenal portion of the bile duct | 4%-5% |
|
IVA IVB |
Dilation of intra- and extrahepatic ducts IVA: Intra- and extrahepatic cysts IVB: Multiple extrahepatic cysts |
10% |
| IV | Saccular dilation limited to the intrahepatic biliary tree (Caroli’s disease) | Rare |
Author’s own research.
Prenatal ultrasound diagnoses have been made at an average gestational age of 20 weeks16,17. The classical triad of pain, right hypochondrial mass, and jaundice is primarily observed in children18. However, studies suggest that this triad’s prevalence is relatively low18-20. In adults, symptom presentation is typically vague and nonspecific, with abdominal pain being the most frequently reported symptom1,20. When more specific symptoms do occur, they tend to be associated with complications such as cholangitis and pancreatitis1,8,21. Laboratory parameters are not diagnostic, though findings may include hyperamylasemia, raised levels of direct and total bilirubin, aminotransferases, and alkaline phosphatase22,23.
Diagnosis of a bile duct cyst relies on identifying biliary dilation once other causes have been excluded, such as neoplasia or stones24. Ultrasound often serves as the initial imaging modality, proving highly effective in detecting cystic structures with a sensitivity rate between 71%-97%, particularly in pediatric cases2,11,23,25. Computed tomography is instrumental in illustrating the cyst’s continuity with the biliary tree, as well as assessing its relations and potential malignancy26. Endoscopic retrograde cholangiopancreatography (ERCP) has largely been superseded by magnetic resonance cholangiopancreatography (MRCP), which remains useful in diagnosing choledochoceles8,27,28. MRCP is lauded for its precise delineation of anatomical pathology, including abnormal pancreatobiliary junctions, and for detecting ductal stones and tumors, rendering it the gold standard without the associated risks of ERCP29,30.
Case presentation
We present the case of a 37-year-old female with a surgical history inclusive of hysterectomy and three prior hospitalizations for epigastric pain, which ultrasound assessments had interpreted as acid peptic disease. The patient sought consultation for epigastric pain radiating to the dorsolumbar region described as a burning sensation, rated 8/10 in intensity, accompanied by multiple episodes of food and bilious vomiting, oral intake intolerance, and choluria. Physical examination did not reveal signs indicative of an acute abdomen. Laboratory tests indicated positive C-reactive protein (CRP), with elevated total bilirubin at 3.16 mg/dL, direct bilirubin at 2.90 mg/dL, alkaline phosphatase at 175 U/L, alanine aminotransferase (ALT) at 300.7 U/L, aspartate aminotransferase (AST) at 248.2 U/L, and urinalysis displaying bilirubin at 1 mg/dL with no additional anomalies.
Subsequent abdominal ultrasound reported a gallbladder containing small calculi, with normal-caliber intra- and extrahepatic bile ducts and a common bile duct measuring 4.5 mm. Owing to the risk of choledocholithiasis, an MRCP was performed, which depicted a normal-sized gallbladder devoid of calculi, cystic dilation of the proximal common bile duct approximately 2 cm below the hepatic duct bifurcation extending to the ampulla of Vater, absence of stones in the common bile duct, and non-dilated intrahepatic bile duct (Figure 1).
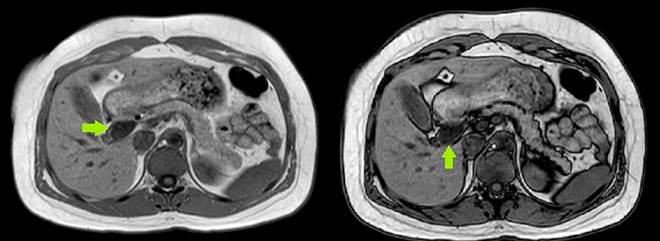
Author’s own research.
Figure 1 Magnetic resonance cholangiopancreatography (coronal section) with a green arrow pointing to the choledochal cyst.
The patient was diagnosed with a choledochal cyst and underwent cyst resection followed by bilio-digestive bypass via Roux-en-Y hepaticojejunostomy (Figure 2).
The surgical exploration revealed a distended gallbladder, a 3 mm cystic duct, and a choledochal cyst measuring 5 x 4 cm with a proximal neck situated 5 mm from the bifurcation of the hepatic ducts and a distal retro-duodenal neck with thickened walls adherent to the portal vein (Figure 3). Two pathological samples were taken: one from the choledochal cyst and one from the gallbladder (Figure 4).
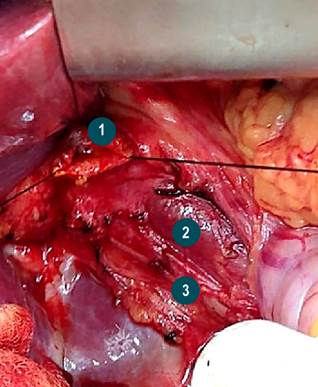
Author’s own research.
Figure 3 Anatomical structures. 1. Confluence of the hepatic ducts. 2. Portal vein. 3. Right hepatic artery originating from the superior mesenteric artery.
Results
The surgical procedure was carried out without any adverse events, and the patient’s postoperative recovery was free of complications. At a follow-up visit fifteen days post-surgery, the patient presented a pathology report which confirmed acute cholecystitis and a benign choledochal cyst.
Discussion
The diagnosis of choledochal cysts in the adult population is becoming increasingly frequent1,19,24,30. In the case under discussion, the definitive diagnosis was established via MRCP after the initial ultrasound yielded inconclusive results. The clinical symptoms and laboratory findings were indicative of cholestasis, prompting the decision to proceed with more definitive imaging. While ultrasound remains the most accessible and cost-effective imaging technique, its variable sensitivity ranging from 71% to 97% can miss choledochal cysts, unlike MRCP, which boasts a detection rate of 96% to 100%29. Prompt diagnosis and intervention are paramount given the elevated risk of complications associated with choledochal cysts in adults, which include obstructive jaundice, symptomatic choledocholithiasis, pancreatitis, secondary biliary cirrhosis, and notably, cholangiocarcinoma1,31,32. The malignancy risk is reported to be approximately 10%-30%6,29,30, and it escalates with age-from 0.7% in the first decade to over 10% beyond the second decade, with more than half of the patients older than 60 years with choledochal cysts showing malignancy1,22. The cyst type is another risk factor, with type I presenting the highest incidence at 68%, followed by type IV at 21%6,14,33.
Consequently, the management of choledochal cysts consists of complete surgical excision6,34. Resection of the cyst along with Roux-en-Y hepaticojejunostomy is the procedure of choice for type I and IV cysts29,30, and partial hepatectomy may be necessary for type IVA. Type II cysts warrant excision and possibly biliary-enteric repair2,29,35. Treatment for type III cysts may involve sphincteroplasty, sphincterotomy36, or the insertion of a drainage tube into the duodenum11. For Todani type V, options include segmental liver resection, liver transplantation, or close patient monitoring to preempt complications29,37,38.
The emergence of minimally invasive surgery has established laparoscopic surgery as a safe and valid alternative. When compared to open surgery, the laparoscopic approach reduces the need for transfusions and shortens the recovery period, despite a typically longer operative duration39,40.
Conclusions
Diagnosing biliary cysts is a significant challenge due to the nonspecific nature of the symptoms and signs associated with the condition. Ultrasound is an effective and cost-effective first-line imaging modality for diagnosing biliary cysts; however, as evidenced in the presented case, a negative ultrasound does not eliminate the possibility of disease. Hence, MRCP is crucial for definitive diagnosis, serving as the gold standard in the detection of choledochal cysts and in ruling out lithiasis and neoplasia. Cyst resection remains the preferred treatment approach due to the significant risk of malignant transformation associated with these cysts.











 text in
text in 





