Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Medicas UIS
Print version ISSN 0121-0319
Medicas UIS vol.26 no.2 Bicaramanga May/Aug. 2013
Bile fistula after penetrating hepatic trauma with
expectant management in the "era" of endoscopic
treatment: clinical report
Eduardo Armenta-Duran*
Lenin Enríquez-Domínguez*
Juan de Dios Díaz-Rosales**
Ever Duarte-Erives***
*MD General Surgeon. Medical Staff. Hospital General Regional No. 66. Instituto Mexicano del Seguro Social. México
**MD General Surgeon. Posdegree Division. Universidad Autónoma de Ciudad Juárez. México
*** Medical Intern. Universidad Autónoma de Ciudad Juárez. México
Correspondence author: Dr. Lenin Enríquez-Domínguez. Calle de los Alamos 9741, Fraccionamiento Los Alamos. Chihuahua. México. e-mail: lenin_enriquez@hotmail.com,
Artículo recibido el 26 de mayo de 2013 y aceptado para publicación el 29 de julio de 2013.
ABSTRACT
Objective: to report a clinical case of bile fistula after penetrating hepatic trauma given its low incidence, which was expectant managed by not having endoscopic retrograde cholangiopancreatography. Clinical case: we present a 28 years-old man, with biliary fistula resulting after a penetrating hepatic trauma. Discussion: bile leakage is a major complication after liver surgery and a rare one in complication of major hepatic trauma. Conventional treatment has consisted of surgical intervention with hepatic debridement, ductal repair, controlled drainage and ERCP when available. Conclusion: biliary fistula was treated successfully with conservative management, the duration of time between hepatic trauma and closure of the fistula was 35 days. (MÉD.UIS. 2013;26(2):71-3).
Keywords: Wounds, Gunshot. Wounds and injuries. Biliary fistula.
Fístula biliar secundaria a trauma hepático penetrante con conducta expectante en la "era"
del tratamiento endoscópico: reporte clínico
RESUMEN
Objetivo: reportar un caso clínico de fístula biliar secundaria a trauma hepático penetrante dada su baja incidencia, que fue tratado de manera convencional al no contar con colangiopancreatografía retrógrada endoscópica. Caso clínico: se presenta un hombre de 28 años de edad, con fístula biliar resultante de trauma hepático penetrante. Discusión: la fuga biliar es una complicación mayor después de cirugía hepática y una complicación poco frecuente después de un trauma hepático mayor. El tratamiento convencional ha consistido en intervención quirúrgica con debridación hepática, reparación ductal, una fistula controlada y ERCP cuando está disponible. Conclusión: la fístula biliar fue tratada exitosamente con manejo conservador, el tiempo entre el trauma hepático y el cierre de la fístula fue de 35 días. (MÉD.UIS. 2013;26(2):71-3).
Palabras Clave: Heridas por arma de fuego. Heridas y traumatismos. Fístula biliar.
INTRODUCTION
Bile fistula is a rare cause of major morbidity after major hepatic trauma, corresponding to 0.5-4.5%1,2 and results in prolongation of the hospital stay. Furthermore, bile retention in the necrotic space leads to the development of the intraperitoneal septic complications that are known to be a cause of dead. Bile leakage is defined as continuous biliary discharge from drainage ducts irrespective of its bilirubin concentrations or delayed biliary fluid collection (biloma), at the scar surface of the liver, with the patient having clinical symptoms such as fever, pleural effusion, or an elevated serum C-reactive protein level after removing the drainage tubes3. A bile fistula may develop following hepatic trauma, as higher pressures in the biliary system make to easier for bile to flow into injured area than to duodenum4.
The Endoscopic Retrograde Cholangio Pancreatography (ERCP) is indicated to identify obstruction, and as a rule endoscopic sphinterotomy promotes healing, when fistula not responding have been successfully treated by placing an endoprosthesis. Actually, ERCP is both diagnostic and therapeutic tool for the safe treatment of biliary ductal injury after severe liver trauma5. But, if this tool is not available in our setting? We evaluated a patient presenting early after liver penetrating trauma with bile leakage in whom the site of fistula was the orifice of gunshot trauma. We discuss the value of the approach and expectant management of this condition.
CASE PRESENTATION
A 28 years-old man was admitted to emergency room with thoracic-abdominal penetrating gunshot trauma. Exploratory laparotomy and right pleural drainage were performed; during surgery we found hepatic injury grade IV, parenchymal disruption involving approximately 25% of right lobe, between Couinaud segments VII and VIII. The patient was hemodynamically unstable, the Pringle maneuver was done and we tried to repair the hepatic injury. However, the injured area was in a continuous bleeding so abbreviated surgery, a damage control surgery, was done; the hepatic areas was packaged and superficial layers closed. The patient was send to intensive care unit.
At day 1 after damage control surgery, the patient was stable and we decided make relaparotomy, we found necrotic tissue and no active bleeding, however a biliary leakage was observed. We tried to repair the area and necrotic tissue was debrided. An open Penrose drain was inserted close to injured area. The package was retired and the abdominal wall closed using mass technique.
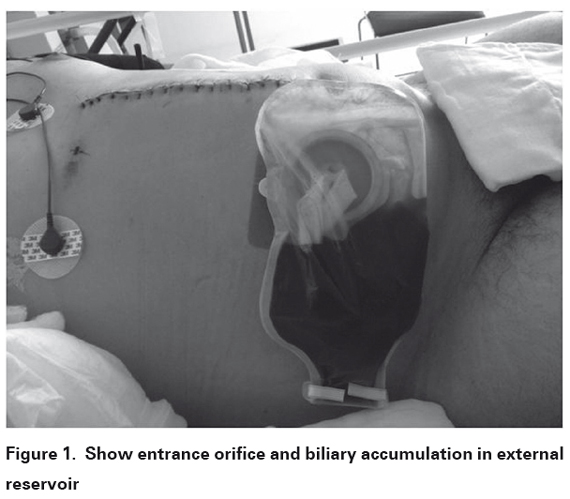
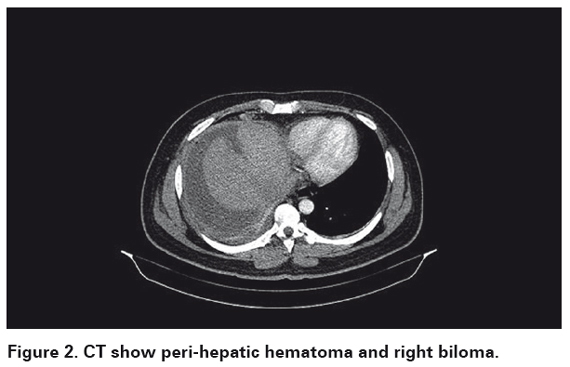
The patient presented biliary leakage of 350 ml/day after second surgery (See Figure 1). Although ERCP is used for definitive treatment in posttraumatic bile fistula, lack of this tool forced us to decided expectant management and wait the healing tissue to close the fistula. The biliary leakage was diminishing and augments during next days, (30 to 250 ml/day). After a full expansion of the right lung, the chest drain was removed on day 6. At day 10, biliary leakage was 50 ml/day. Right peri-hepatic hematoma, right biloma, and right pleural effusion were reported in computer tomography at day 22 (See figure 2), right inferior thoracotomy was performed at day 28. No bile leakage to pleural space was detected, and pleural drain was inserted to re-expand the lung after thoracic surgery. The chest drain was removed on postoperative day 5, and discharged on postthoracotomy day 6 with only 15 ml/day of biliary leakage. Clinical follow-up has been continued for 2 months without any complaint.
DISCUSSION
Trunkey et al. reported that 30% of patients with hepatic trauma had one or more complications in it. The overall mortality in this series was 13%, and this mortality was related to hemorrhage and hypovolemic shock2. Biliary leakage was not common, in our review of 86 patients with hepatic penetrating trauma we do not found any biliary fistula6. Literature report only 4-6% patients with blunt and penetrating trauma will develop bile leak7,8. Posttraumatic bile leaks may present either as bile peritonitis or as a bile lead through a drain site like our patient7.
Although earlier studies showed that the majority of complications following liver trauma can be successfully managed with percutaneous drainage8, safety of endoscopic management is the gold standard currently9. But in developing countries, with lack of many diagnostic and therapeutic tools, expectant management in patients with biliary fistula continues like an efficient tool in the patient with severe liver trauma. The median for bile leak closed spontaneously is 33-44 days7,8, our patient had 35 days to closed biliary leakage. Although, no mortality is reported due to biliary leakage, all complications reflect the severity of the initial injury rather than the bile leak7,8.
CONCLUSION
Although endoscopic sphincterotomy is a reliable and effective therapeutic, in management in patients with external biliary fistulas10,11. Patients in hospitals without this tool, expectant management with percutaneous drainage remains like an effective and safe conduct.
CONSENT
Written informed consent was obtained from the patient for publications of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
1. Silvio-Estaba L, Madrazo-González Z, Ramos-Rubio E. Current treatment of hepatic trauma. Cir Esp. 2008;83(5):227-34. [ Links ]
2. Trunkey DD, Shires GT, Mc Clelland R. Management of liver trauma in 811 consecutive patients. Ann Surg. 1974;179(5):722-8. [ Links ]
3. Terajima H, Ikai I, Hatano E, Uesugi T, Yamamoto Y, Shimahara Y, et al. Effectiveness of endoscopic nasobiliary drainage for postoperative bile leakage after hepatic resection. World J Surg. 2004;28(8):782-6. [ Links ]
4. Vagianos C, Polydorou A, Karatzas T, Vagenas C, Stavropoulos M, Androulakis J. Successful treatment of postoperative external biliary fistula by selective nasobiliary drainage. HPB Surgery. 1992;6:115-24. [ Links ]
5. Grala P, Skrzywanek P, Sowier A. Biliary fistulas resulting from blunt hepatic injury treated by endoscopic diversion of the bile flow. Acta Chir Belg. 2009;109(1):47-51. [ Links ]
6. Enríquez Domínguez L, Castillo Moreno JR, Herrera Ramírez F, Díaz Rosales JD. Trauma hepático por heridas punzocortantes y por arma de fuego. Nuestra experiencia en Ciudad Juárez. Cir Gen. 2011;33(1):21-5. [ Links ]
7. Hollands MJ, Little JM. Post-traumatic bile fistulae. J Trauma. 1991;31(1):117-2 [ Links ]
8. Howdieshell TR, Purvis J, Bates WB, Teeslink CR. Biloma and biliary fistula following hepatorraphy for liver trauma: incidence, natural history and management. Am Surg. 1995;61(2):165-8. [ Links ]
9. Hommes M, Kazemier G, Schep N, Kuipers E, Schipper I. Management of biliary complications following damage control surgery for liver trauma. Eur J Trauma Emerg Surg. 2013;39(5):511-6. [ Links ]
10. Del Olmo L, Meroño E, Moreira VF, Garcia T, Garcia Plaza A. Successful treatment of postoperative external biliary fistulas by endoscopic sphincterotomy. Gastrointest Endosc.1988;34(4):307-9. [ Links ]
11. Piper GL, Peitzman AB. Current Management of hepatic trauma. Surg Clin North Am. 2010;90(4):775-85. [ Links ]