Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Iatreia
Print version ISSN 0121-0793
Iatreia vol.25 no.2 Medellín Apr./June 2012
INVESTIGACIÓN ORIGINAL
Patterns of treatment for childhood malaria among caregivers and health care providers in Turbo, Colombia
Pautas de tratamiento para la malaria infantil entre los cuidadores y profesionales de la salud en Turbo, Colombia
Ysabel Polanco Lopez de Mesa1
1 Profesora Departamento de Medicina Preventiva y Salud Publica, Facultad de Medicina, Universidad de Antioquia, Medellín, Colombia.
Candidata a PhD en Salud Pública, Universidad de La Florida, Estados Unidos. ipolanco@ufl.edu
Recibido: agosto 12 de 2011
Aceptado: octubre 31 de 2011
SUMMARY
Malaria represents a major cause of death among children in many areas of the world, especially in tropical countries. Colombia constitutes a malaria endemic country in 90% of its territory. This study, undertaken in Turbo (Antioquia), examined care-seeking patterns and barriers to appropriate treatment for Colombian children with fever and /or convulsions, two key symptoms of malaria. The study focused on community perceptions of and responses to febrile illness, using illness narratives as the primary data collection vehicle. The researcher used semi-structured interviews for health narratives with caregivers and health providers. Analyses of 67 illness narratives collected in the course of the study indicated that caregivers, the majority of which are mothers, recognize fever and treat it promptly. They identified fever, chills, headache, vomiting, and weakness as the most frequent symptoms of malaria. Synchronic and diachronic analyses showed that most treatments begin at home. Common home treatments include baths with herbs and use of anti-pyretic drugs. Neither caregivers nor traditional healers conceptualized malaria as a disease that involves the spirits. Caregivers described an intricate mixture of biomedicine, home treatment, and traditional medicine. This pluralistic approach helps to explain, in part, the caregiver's decision-making process. Moreover, from the biomedical perspective, this complex mixture of knowledge can lead to inadequate treatment of children with malaria.
KEY WORDS
Caregivers, Colombia, Children, Malaria
RESUMEN
La malaria representa una causa importante de muerte infantil en muchas áreas del mundo, especialmente en países tropicales. Colombia es considerado como un país endémico para malaria en el 90% de su territorio. Este estudio, llevado a cabo en la localidad de Turbo (Antioquia), exploró los patrones de cuidados y las barreras para el tratamiento apropiado en niños colombianos con fiebre y/o convulsiones, dos síntomas claves de la malaria. El estudio se concentró en las percepciones y respuestas de la comunidad ante la enfermedad febril, utilizando narrativas de la enfermedad como vehículo principal de la recolección de datos. El investigador usó entrevistas semi-estructuradas para las narrativas de enfermedad con los cuidadores de los niños y con los proveedores la salud. El análisis de 67 narrativas de enfermedad colectadas en el curso del estudio indicó que los cuidadores de los niños, que en su mayoría son las madres, reconocen la fiebre y la tratan prontamente. Los cuidadores identificaron la fiebre, los escalofríos, los dolores de cabeza, el vómito y la debilidad como los síntomas más frecuentes de la malaria. Los análisis sincrónico y diacrónico mostraron que la mayoría de los tratamientos comienzan en la casa. Los tratamientos caseros más comunes incluyen baños con hierbas y el uso de medicamentos antipiréticos. Ni los cuidadores ni los sanadores tradicionales conceptualizaron la malaria como una enfermedad que involucre asuntos espirituales. Los cuidadores describieron una mezcla de biomedicina, tratamientos en casa y medicina tradicional. Este enfoque pluralista ayuda a explicar, en parte, el proceso de toma de decisiones de los cuidadores. Adicionalmente, desde la perspectiva biomédica, esta mezcla compleja de conocimientos puede conducir al tratamiento inadecuado de los niños con malaria.
PALABRAS CLAVE
Colombia, Cuidadores, Malaria, Niños
INTRODUCTION
Malaria constitutes a debilitating vector-borne disease with a high incidence in tropical areas. Half of the world's population lives at risk of malaria, and an estimated 243 million cases led to nearly 863,000 deaths in 2008 (1,2). Most cases (~85%) occur in the African Region, followed by South-East Asia (~10%), the Eastern Mediterranean (~4%), and the Americas (1%) (1,3). Children with malaria who do not receive adequate medical care may suffer serious health problems often leading to their death. In 2009, malaria caused an estimated 800,000 fatalities. It is estimated that approximately 85% of annual deaths due to malaria occur in children under 5 years of age (2). In addition to the inherent health problems caused by malaria, the disease has devastating economic impacts. Malaria can reduce gross domestic product by as much as 1.3% in countries with high rates of the disease (2,3).
Despite the apparent undersized malaria figures for the Americas compared to the African and Asian continents, Latin America experiences a pressing malaria situation. In 2008, the Americas reported 560,221 malaria cases. Endemic transmission of malaria exists in 21 countries of the region including Colombia (4). Countries in the Amazon region reported the highest number of cases in 2008. Brazil experienced 315,553 cases in 2008, 56% of the total cases in the Americas. By the year 2010 endemic transmission figures for the Americas increased to 23 countries with almost 20% of the total population at some degree of risk (3). Reported cases in the region decreased from 1.18 million in 2000 to 526,000 in 2009. Albeit this reduction, four countries (Brazil, Colombia, Haiti and Peru) totaled 90% of the cases in 2009, with P. vivax accounting for 80% of all cases reported. For several years, Colombia has occupied an important place with the second highest number of malaria cases in the American continent (4).
Colombia permanently experiences malaria transmission and infection in ~90% of its territory. The number of reported cases doubled from 71,012 cases in 1999 to 139,542 cases in 2002 (5). In 2008, PAHO reported 78,313 malaria cases in Colombia (5). Three South American countries (Brazil, Colombia and Guyana) rank with the smallest reductions (25% to 50%) in the number of confirmed malaria cases between 2000 and 2009 (2).
In addition to climatic conditions favorable for the proliferation of the vector in tropical America (6), cross-sectional studies show that human induced environmental degradation in tropical countries, e.g., deforestation in the Amazon region of Brazil, can drive significant increases in malaria incidence (7). Several studies report that a variety of social, economic, and cultural factors affect exposure to malaria (8,9). Changes in the parasite and the vectors influence the increased rates of malaria morbidity. However, such increases can also be attributed to human behavior that relates to individual, culturally-coded patterns and to larger-scale sociological phenomena, including political and economic factors (10). Despite the importance of human behavior in devising holistic strategies to reduce malaria-related mortality and severe morbidity, few studies that incorporate medical anthropology to assess the problem have been conducted; the majority of them have been undertaken in African communities (8, 11,12). The literature review for this research indicates that similar studies in Colombia are scant.
This research focused on care-seeking behavior of caregivers of children with malaria and on health provider's treatment patterns. Malaria can progress from mild illness to severe disease to death over a brief time span (13). For this reason, understanding the factors that influence caregivers of children to seek and complete adequate treatments constitutes a critical component to develop effective malaria control interventions (8).
Maternal diagnosis of malaria does not always correspond to biomedical diagnosis (4, 11). Local populations often have the ability to recognize malaria symptoms and to associate them with the necessity to seek treatment (14). Caregivers may classify conditions with malaria symptoms as different illnesses, describing them in distinct terms from those they use for fever or simple uncomplicated malaria. Lay people most likely classify malaria as severe when the symptoms include convulsions (14, 15). Studies throughout Africa suggest that when caregivers recognize fever in their children, most of them provide home treatment (12, 16). Caregivers employ multiple treatments for severe and prolonged illnesses (17). Studies identified multiple, and simultaneous patterns of care-seeking behavior for febrile illness. Hierarchy or sequence of resorts may prove important for understanding potential delay in getting appropriate treatment (16, 18). While at least half of all fever cases may eventually make contact with the formal health sector (19), most caregivers initially treat cases at home or through informal health care providers (20). A significant proportion of antimalarial drug use occurs at home. However, people frequently use these drugs in inadequate ways including underdosage treatments, or use of the drug to treat illnesses other than malaria (21). Both procedures contribute to enhance the parasite's resistance to antimalarial drugs (22, 23). Furthermore, several studies also found that a variety of cultural, social and economic factors affect treatment-seeking behavior (21-23).
OBJECTIVES
1) To understand the multiple ways in which caregivers provide treatment to children under 11 years of age, who experience fever and/or convulsions, two key symptoms of malaria.
2) To examine the role of different health providers (e.g., physicians, whether at the health center or in private practice, traditional healers, and drug vendors) in treating febrile illnesses in children, especially malaria.
MATERIALS AND METHODS
Study site
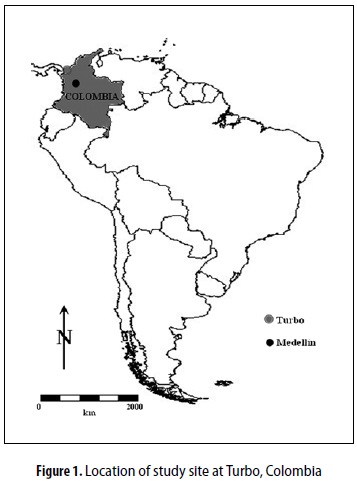
The investigation was undertaken at the San José Health Center in the malaria-endemic town of Turbo, Antioquia Department (Urabá region, northwestern Colombia, figure 1). Turbo has a population of ~140,000 inhabitants, most of them of Afro-Colombian descent (~81%) with a minority of mestizos and indigenous people. Over 40% of Turbo's population consists of individuals under 14 years of age (24). Turbo's precarious sanitation services lack adequate sewage systems and potable water supplies. Environmental characteristics of the municipality, and the region around it, marked by high temperatures and rainfall, and the lowland fluvial networks of the Atrato Basin, are ideal for propagation of the malarial vector (6, 25). Average temperature fluctuates between 28°- 30 °C throughout the year while mean annual precipitation is around 2.500-2.000 mm (26). A combination of socioeconomic and environmental factors in Turbo makes it one of the municipalities in Antioquia with the highest number of malaria cases in the past 10 years: 9.592 were reported in 2007 and 2.571 in 2010 (highest number of cases in the Urabá region) (27).
Sampling procedures
The researcher collected data by means of semistructured interviews with caregivers of children with febrile illness. Inclusion criterion was serving as caregiver for a child 11 years of age or younger, who had experienced fever and/or convulsions in the previous four weeks. For health providers inclusion criterion was working as such in Turbo in one of these categories: medical doctor, traditional healer, or pharmacist. The researcher interviewed 67 caregivers and 15 health providers. Caregivers took the children under their protection to the health center in order to determine, by means of a blood smear test, if they had malaria.
Description of methods
This was a qualitative study but it also included some quantitative demographic information. The researcher used semi-structured interviews to gather information, and subsequently analyzed the quantitative information using Excel® to create descriptive statistics. Qualitative data was transcribed and manually coded to identify common themes and patterns. The qualitative reliability of the study was performed by the main investigator, the academic advisor and a research assistant as follows: a) transcripts were triplechecked to make sure they did not contain mistakes produced during transcription; b) potential shifts in the meaning and definition of codes were identified and removed so as to avoid jargon variations in local terminology concerning symptoms and health conditions that imply or not malarial infection; c) a crosscheck process was developed to assure that the words used by the caregivers and participants were interpreted in a similar, consistent manner (28).
Subjects voluntarily decided to participate in the study and signed an informed consent form approved by the Institutional Review Board 2 (IRB2) at the University of Florida, USA.
Research protocol for the interviews included two simultaneous phases to answer specific questions related to the overall care-seeking process:
Phase 1: Illness Narrative Module. This phase allowed to: 1) identify treatment-seeking patterns, including types and sequence of treatment actions, and factors that affect treatment decisions; 2) examine how caregivers defined the onset of illness, and what symptoms they used to view a child as ''sick'' and the illness as ''severe''; 3) ascertain knowledge of correct dosage for antimalarial drugs, actual dose given to a child, and reasons why that dose was administered; 4) identify what factors prompt caregivers to seek help from various providers; 5) determine the amount of time between onset of ''alarm'' signs and treatment by health providers; 6) identify how caregivers define treatment success or failure; and 7) identify factors that facilitate or impede appropriate care-seeking.
Phase 2: Health Provider Module. The researcher conducted interviews with five medical doctors and 10 non-facility-based providers, and identified three types of health providers. The aims varied for each type of provider:
- Private clinic/health center doctor: To determine the provider's role in treating illnesses with fever, especially malaria; the provider's treatment for malaria, and for convulsions.
- Traditional healer: To determine the provider's role in treating illnesses with fever, especially malaria; the perception of causes for fever, and the treatment for it; role in treating illnesses with convulsions, perception of causes for convulsions, and treatment for them.
- Pharmacist/drug vendors: To determine the vendor's role in treating malaria in children; advice/recommendations for malaria treatment, and if caregivers seek advice from vendors on dosage to treat malaria in children.
The researcher purposely selected the study site based on the incidence and prevalence of malaria. Therefore, the findings may not be generalized beyond the 67 caretakers and 15 health providers interviewed.
Methodology limitations
A potential limitation of the methodology implemented in this study can be identified for the Health Provider Module. Specifically, such limitation can be related to information bias. Information that health providers yielded could be influenced by varying degrees of bias due to the explicit nature of the research objectives and other project-related information included in the informed consent. Possibly, some of the information was given to conform to the researcher's interest. To reduce this bias, the educational background of the researcher was not disclosed to participants and the researcher specified that the answers were anonymous and were not going to be judged ''right'' or ''wrong''.
RESULTS
Treatment-seeking patterns and health careseeking behavior
Caregiver's definition of malaria and its cause(s)
Local people in the Turbo region define malaria disease as ''paludismo''. Four out of five caregivers knew that mosquito bites constitute the main cause of malaria. The remaining caregivers mentioned causes such as: ''taking a bath with cold water when the person is sweating'', ''the bite of a bird'', ''drinking dirty water'', ''living in close contact with sanitary fields'', and ''breathing contaminated air''.
Caregivers, 67% of which were mothers, offered different definitions for malaria such as the following: ''when one has fever and headaches'' (29%), ''virus'' (17%), ''don't know'' (16%); ''illness'' (10%), ''dangerous disease'' (10%), ''infection produced by mosquito'' (9%), ''parasite in the human blood'' (4%), ''illness acquired by drinking non potable water'' (3%), ''illness acquired by weather change'' (1%), ''poison injected by mosquito in the blood'' (1%). The most common symptoms children experienced included fever, chills, headache, and vomiting. In 97% of cases, caregivers interpreted these symptoms as indicative of malarial infection. Caregivers expressed that the word ''fever'' could be related to cold symptoms, but if the fever lasted more than three days, then the same word had a malaria connotation. Caregivers indicated that when fever was accompanied by chills and headache, these symptoms had a strong connection with ''paludismo'' (i.e., malaria) and they were a triggering condition to seek help.
Treatment-seeking patterns
Treatment-seeking patterns incorporate two components: recognition of signs, and treatment for fever. Recognition of signs explains how promptly caregivers identify the signs of illness, including fever, chills, convulsions, and vomiting, as an indication of malarial infection. Based on their perceptions of these signs, caregivers make decisions about treatment.
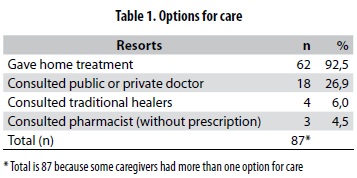
Recognition of signs: In the narratives, fever emerged as a defining indicator of illness. Fever indicates a serious problem when temperature exceeds 40 °C, or when accompanied by other signs including vomiting, weakness, headache, and chills. Other symptoms caregivers related to malaria included diarrhea, delirium, dizziness, and thirst. Treatment for fever: Home treatment constitutes the initial response to fever. Approximately 92% of caregivers reported a form of home treatment as their first response to febrile illness (table 1). Only 36% of children were taken to the health center within 36 hours from the time caregivers noticed fever. The children included in the study remained sick for an average of 6 days before seeking medical attention at the health center. This delay indicates that the caregiver's decision to look for treatment was not sufficiently prompt. Ideally, caregivers should take children to the health center within 24-48 hours following onset of symptoms.Home treatments include both traditional and modern remedies. Common home treatments found included:
- Sponging/bathing: Performed with cold or warm water and sometimes with herbal infusions to lower the fever. Herbs most commonly used: rosa amarilla and matarratón . Less commonly used: balsamina, lemon leaves, leafs from orange trees, guandú, anamú, malba, bonche, gallinaza, venturosa, and leaves from avocado trees. Over 28% of caregivers reported using warm or cold water, and over 34% used baths with herbs.
- Commercial anti-pyretics: Caregivers provided commercial anti-pyretics at home in 85% of cases as the initial treatment, including acetaminophen, acetylsalicylic acid, hyoscine butylbromide, and ibuprofen.
- Herbal drinks: Caregivers used herbal drinks as initial treatment in 7% of cases. Herbs and substances used included: anamú, coryander, onion, yanten, ajenjo, paico, matarratón, garlic, and/or lemon. A mixture of herbs with ''aguardiente'' (a local alcoholic drink derived from sugar cane) was also reported by caregivers as of use to treat fever.
- Antimalaric medications: One caregiver reported the use of chloroquine and primaquine at home as a first response. This caregiver used quantities below the recommended dose (underdose) and without prescription. No use of artemisinin-based combination therapy (ACT) was found in this study. Some caregivers expressed awareness of the risks associated with administering medication to children without diagnosis and prescription. Some caregivers (15%) reported that if they give a pill (other than acetaminophen) to the child, the blood smear can be negative. The smear test should be positive when children experience ''paludismo''. Using biomedical standards, if a patient with malaria receives antipyretics, other that acetaminophen, the blood smear test can produce a false negative result.
Factors that affect health care-seeking behavior
Several factors influenced the health care-seeking behavior of these caregivers including availability of diagnosis and drugs, role and quality of health provider, distance from the health center, paper work, and cost.
Availability of diagnosis and drugs. Two major reasons explained why caregivers went to the health center: 1) the possibility of having a correct diagnosis using the blood smear, and 2) to obtain the drugs for treatment.
Role and quality of health provider. In this study the term health provider refers to three categories: medical doctors, traditional healers, and pharmacists. Caregivers generally expressed a high level of confidence in formal, biomedical health providers for treating childhood febrile illnesses. They believed these caregivers possess medical expertise to give appropriate treatment to their children.
- Medical doctors. Some of the caregivers (25%) visited medical doctors before they obtained the blood smear at the health center. In 53% of those visits, medical doctors did not order the blood smear for the febrile child. Despite the fact that they provide medical services in a highly endemic malaria zone, surprisingly two out of five medical doctors interviewed did not know how to treat patients with malaria. They did not remember the names or pharmacologic properties of the different antimalaric drugs available, and they did not know the combinations commonly used and/ or the appropriate dosages.
- Traditional healers. This category of health providers includes three types:
- Rezandero (prayer): Members of the community with no formal study whom people consider to possess spiritual power for healing. Other community members seek their help when they believe the illness has a spiritual or supernatural cause. These healers cure by praying, and by performing various healing rituals with the ill person.
- Traditional healers with some degree of formal study (diploma) and with a homeopathic orientation. These healers use traditional beverages and potions they prepare using a wide range of herbs.
- Traditional healers without formal study. These healers, which have never received diplomas or certificates, also use traditional herbal beverages but they do not pray.
Traditional healers mentioned that they treated children with malaria. None of the individuals interviewed (caregivers and traditional healers) considered malaria as an illness produced by spiritual disorders.
- Pharmacists. According to the narratives, caregivers seldom go to the pharmacists to buy pills without prescriptions. Only 3% of caregivers bought medicine at a pharmacy without prescriptions before they went to the health center.
Distance from the health center. Caregivers who came from rural areas reported difficulty going to the health center because of the distance, and travel time.
Paper work. To receive service at the health center people need to complete paperwork, which creates an obstacle in the care-seeking process, causing delays in response to malaria. This situation is more problematic for illiterate individuals.
Cost. Under the current scheme of medical services in the country, patients often need to make a copayment. A substantial number of caregivers could not afford to pay 20,000 Colombian pesos (US $12) which represents the full cost of the visit.
Resorts to care and sequence of treatment
Each illness narrative provided a chronological account of places where caregivers seek care. Caregivers gave information for synchronic analysis that documented frequency of use for care options available, while diachronic analysis showed the sequence of options in seeking care. Caregivers reported the following options as sources of care: home treatment, health center, traditional healer, pharmacy, and public or private medical doctor.
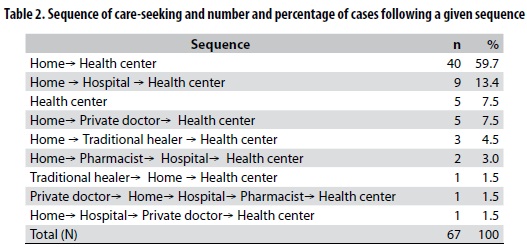
The synchronic analysis (table 1) shows the percentage of sample cases involving, at any point in the illness, a particular option for care. Home treatment dominates this parameter with 92,5% followed by visits to private or public doctors with 26,9% and to traditional healers with 6,0%. The minority of cases are represented by visits to the pharmacists (4,5%). The diachronic analysis focused on the sequence in which caregivers sought treatment from each of these sources. A total of nine sequences was found and they appear in table 2. The predominant health seeking pattern is Home- Health Center (59,7%) followed by Home- Hospital - Health Center (13,4%), Health Center only (7.5%) and Home - Private Doctor - Health Center (7,5%). All other sequences exhibit lower percentages.
DISCUSSION
Health narratives from this research showed that caregivers possess a variety of definitions for malaria. These definitions indicate a limited understanding about the current biomedical knowledge concerning the disease. Caregivers explicitly stated their lack of understanding of the nature of the disease, cause, treatment, prevention, and associated threats to human health. Low levels of awareness relative to the biological cause of malaria often lead to inappropriate health seeking processes. Although it is undetermined weather this low level of awareness can be attributed to inadequate public health and education practices within the community, it underlines the need for more coherent public health intervention. Such interventions must incorporate educational efforts in relation to malaria etiology, transmission process, associated symptoms and appropriate treatmentprevention schemes.
Fever represents a serious condition when accompanied by other illness signs including vomiting, weakness, headache, and/or chills. In this study fever was identified as the most frequently recognized symptom of childhood malaria, a finding that is consistent with comparable studies in Africa (11, 12, 29). Similarly, convulsion is seen by caregivers as a symptom of an advanced stage of malaria development, although in the majority of cases mothers informed not to have seen their malaria infected children in stages of convulsion, probably because fever is usually controlled before it leads to convulsion events. Alternatively, reduced reports on convulsion stages can be explained by the fact that the most prevalent species of malaria infection in Turbo is P. vivax and not P. falciparum which is the type that more often leads to convulsive stages as it has been documented mostly in African malaria endemic countries (16).
Caregivers practiced home treatment as their first response to febrile illness. Synchronic analysis showed that treatment occurred predominantly at home (92%). Diachronic analysis showed that caregivers provide treatment at home first (more than 96%), and then take the child to the health center, usually when complications develop or to get the blood smear for a definite diagnosis. Since the home is the place where treatment is first implemented (totaling 92%), it is suggested that individuals who provide care at home, most notably mothers (67%), be trained to more accurately recognize, diagnose, and treat malaria in their children, and to judge when to refer to the health facilities. This will aid rapid diagnosis and treatment of malaria, another essential element of the Roll Back Malaria Partnership (30), with a great potential to impact malaria control programs in Colombia.
Perception of malaria as a serious health condition did not translate into a high level of utilization of the health center as the initial step for health care of ill children. Proximity and the need to obtain a definite diagnosis are perhaps the major reasons for utilizing the services of the health center. In addition to increasing the level of awareness of mothers, there are numerous advantages in training health center personnel and other health providers including pharmacists and traditional healers to maximize the efficiency of their services considering the important role they play in the malaria treatment process. This approach should be supported by systematic research and education efforts, with a high degree of community participation.
Most home treatments include the use of commercial anti-pyretics, and baths with or without herbs. Self medication ranks as the preferred first option for management of childhood malaria, particularly for the control of febrile stages. Potential dangers of self medication have been documented worldwide (3) and it should not be encouraged unless supported by very efficient educational strategies. Caregivers have limited knowledge about the dangers posed by undertreatment including life threatening risks for the child and parasite resistance to antimalarial drugs; both situations lead to harmful public health outcomes (22, 31). In 2007 a study by Bosman and Mendin reported that Colombia was among a group of nine endemic countries (Botswana, China, Colombia, Eritrea, Nepal, Pakistan, Sri Lanka, Swaziland, Vanuatu) with recorded treatment failure rates of their first-line antimalarial medicines exceeding 10%, concluding that heath programs for these countries should adopt the use of artemisinin-based combination therapies (ACTs) (32). Although by 2009 ACTs were adopted as national health policy for first-line treatment of P. falciparum malaria in most countries of the American Continent, chloroquine is still widely used in some countries, including Colombia (3). Until 2006, Colombia was the only country in South America that had not yet introduced ACTs into its national malaria program (23). However, a recent investigation carried out in Western Colombia (in the Choco Department) indicates that ACTs are being used for treatment of P. falciparum malaria since the end of 2006 (31).
The possibility of having a correct diagnosis using the blood smear, and obtaining appropriate drugs for treatment, constitute the most important determinants for caregivers to proceed in the care-seeking response. Caregivers generally experience high confidence in the biomedical system for treating childhood febrile illness. Nevertheless, home treatment is perhaps the preferred option for caregivers due to a combination of factors that may include: ease of attention of the ill child by the mother, the benefits of staying at home and take care of other home-related obligations, low cost, reduced travel time, lack of medical centers in the vicinity, etc. The fact that lack of money is among the most common reasons for not using the health center or private practitioners as the first resort underlines the prevalent role poverty plays in the decision making process and how other competing needs hinder access to treatment in health facilities. Monetary costs associated with biomedically oriented health services as a barrier to health access have been documented in similar studies in Africa (12) and is a hallmark of the health situation in Colombia whereby malaria is just another piece of the puzzle of deficient and costly heath services(33, 34). The choice of treatment has also been shown to be dependent on access, attitudes towards the provider, and beliefs about the disease. Geographic isolation (distance) and cost -two prevalent features of marginalized social groups in Colombia-, as the main constraints to proper utilization of the health center for malaria, have been highlighted in similar studies elsewhere (15, 16, 19). Home treatment as the first resort clearly dominates both the synchronic and diachronic analyses. Healers identified by caregivers included rezanderos (prayers) and traditional healers (curanderos) with or without some degree of formal study and with a clear homeopathic orientation. However, caregivers rarely seek help from these care providers. Caregivers and traditional healers do not consider malaria as an illness produced by spiritual disorders contrary to what has been found in African countries (15, 16) .
In addition to the economic and logistic difficulties linked to the use of home treatment as the first resort for malaria infected children, it is important to highlight the lack of specific training for malaria treating procedures in the medical personal interviewed in this investigation. Medical doctors in this malariaendemic region have a vague knowledge of the epidemiology of the disease and often ignore some malaria treatment schemes, and adequate dosages. Situations like this are related to exacerbation of the disease mortality and morbidity in the region.
Thus, the low level of awareness of the cause of malaria by mothers and medical personnel may be an important factor in the increase of morbidity and mortality of malaria in children. This situation can only be improved with further research and coherent health and education interventions which should address specific beliefs and perceptions. This is in agreement with strengthening community awareness as a key element of the Roll Back Malaria Initiative (30).
Results of this investigation are important for the implementation of coherent public health policies designed to reduce the incidence of malaria at the regional scale. To this goal, it is fundamental to promote a social and institutional milieu that supports further research (particularly in medical anthropology and public health) and participatory educational strategies in which local knowledge is considered a key aspect of the public health interventions for the target population. This local knowledge should be valued and recognized so as to include the community under study as active participant in public health programs aimed at reducing malaria incidence and prevalence. A participatory approach in research, education and public health policy should have more significant effects on malaria prevention and treatment.
The compartmentalization of health practices that derived from the introduction of health legislation by the Colombian government (Law 100, year 1993) (34) is another key aspect to be considered in how to approach malaria as a major public health issue. The privatized, profit oriented scheme of health services in Colombia, despite its supposedly ''regulated competence'' nature, modified the organization, planning, execution and finances of health services, including the malaria control program. The Sistema General de Seguridad Social en Salud (SGSSS) (General System for Social Security and Health Services) created a disconnection between malaria control activities provided by government-based agencies and those offered by private institutions (Instituciones Prestadoras de Salud, IPS). Under this sociopolitical framework, malaria control activities (prevention and treatment) have been fragmented and are profit oriented (33).
Specifically in the Antioquia Department, long-term malaria trends indicate a fall in mortality accompanied by an increase in the morbidity, particularly since 1990 (35). Decentralized malaria policies have strongly influenced the structure of the malaria control program. Malaria and other vector-borne diseases control programs exist both at the department level and in the municipalities where diagnostic and treatment activities are carried out. Research has shown that the control model has some weaknesses in the sectorial and intersectorial public policies. The program has not managed the disease in an integral and effective way, i.e., in its social and political contexts. Moreover, social involvement has not reached its potential (35), despite the fact that findings of this study, as well as those of studies in Africa, indicate the value of local knowledge in understanding the epidemiology of malaria. Such knowledge base (attitudes, beliefs, etc.) must be an essential component of community participation to help design and implement malaria control interventions and programs provided either by the state or by IPSs in the Urabá region specifically in Turbo. These educational activities marked by a participatory approach rooted in medical anthropology studies should target the population at the individual and community levels.
CONCLUSION
A dual system of health care exists in Turbo for children infected (or suspected to be infected) by malaria in which caregivers implement a mixture of biomedicine and traditional medicine. Febrile illness care administered at home, in the majority of cases by mothers, is a hallmark of the care seeking behavior of most caregivers. Therefore, educational programs about proper diagnosis and treatment for malaria should be implemented to raise the level of understanding among said caregivers while also including health providers, and drug vendors (pharmacists). In establishing such programs, government planners in Turbo must take into account caregiver knowledge and beliefs, particularly in the case of mothers.
Researchers and health providers should consider the knowledge that local individuals possess about traditional treatments for malaria because their awareness can suggest important directions for expanding research on medicinal plants. Promoting use of these plants may also be appealing within the context of the local culture. These prospects require further study.
Treatment-seeking behavior in the community is largely determined by individual perceptions of the relative effectiveness of competing care systems. Inadequate treatment-seeking behaviors found in this study, expressed by the lower level of use of the health facilities as a place where treatment is first sought and/or inadequate treatment at home (delay in seeking treatment for childhood malaria, no use or underdosage of antimalaric drugs, etc.), clearly indicate the need for health education supported by coherent intervention programs, participatory in nature, as well as the implementation of urgent measures to relieve poverty and reduce the cost of allopathic care.
ACKNOWLEDGMENTS
This study was possible thanks to the Summer Research Grant provided by the Tinker Foundation University of Florida, USA. I thank my family for all the unconditional support given during my research effort.
REFERENCES BIBLIOGRÁFICAS
1. World Health Organization. World Malaria Report 2009. Geneva: 2009. [ Links ]
2. World Health Organization. Malaria. Fact sheet. 2011;(94). [ Links ]
3. World Health Organization. World Malaria Report 2010. Geneva: World Health Organization; 2010. [ Links ]
4. Pan American Health Organization. Report on the Situation of Malaria in the Americas, 2008. Washington D. C.: PAHO; 2008. [ Links ]
5. Pan American Health Organization. Interactive statistics of malaria in Colombia [Internet]. Interactive malaria statistics. 2010; Available from: http://new.paho.org/hq/index.php?option=com_contenttask=viewid=2632Itemid=2049 [ Links ]
6. Poveda G, Rojas W, Quiñones ML, Vélez ID, Mantilla RI, Ruiz D, et al. Coupling between annual and ENSO timescales in the malaria-climate association in Colombia. Environ Health Perspect. 2001 May;109(5):489–93. [ Links ]
7. Olson SH, Gangnon R, Silveira GA, Patz JA. Deforestation and malaria in Mâncio Lima County, Brazil. Emerg Infect Dis. 2010 Jul;16(7):1108–15. [ Links ]
8. Tanner M, Vlassoff C. Treatment-seeking behaviour for malaria: a typology based on endemicity and gender. Soc Sci Med. 1998;46(4-5):523–32. [ Links ]
9. Bates I, Fenton C, Gruber J, Lalloo D, Medina Lara A, Squire SB, et al. Vulnerability to malaria, tuberculosis, and HIV/AIDS infection and disease. Part 1: determinants operating at individual and household level. Lancet Infect Dis. 2004 May;4(5):267–77. [ Links ]
10. Desowitz RS. The Malaria Capers : more tales of parasites and people, research and reality. New York: W. W. Norton & Company; 1991. [ Links ]
11. Lubanga RG, Norman S, Ewbank D, Karamagi C. Maternal diagnosis and treatment of children's fever in an endemic malaria zone of Uganda: implications for the malaria control programme. Acta Trop. 1997 Oct 14;68(1):53–64. [ Links ]
12. Agu A, Nwojiji J. Childhood malaria: mothers' perception and treatmentseeking behaviour in a community in Ebonyi State, South East Nigeria. Journal of Community Medicine and Primary Health Care. 2005;17(1):45–50. [ Links ]
13. Greenwood B, Mutabingwa T. Malaria in 2002. Nature. 2002 Mar 7;415(6872):670–2. [ Links ]
14. Bukirwa H, Nayiga S, Lubanga R, Mwebaza N, Chandler C, Hopkins H, et al. Pharmacovigilance of antimalarial treatment in Uganda: community perceptions and suggestions for reporting adverse events. Trop Med Int Health. 2008 Sep;13(9):1143–52. [ Links ]
15. Makemba AM, Winch PJ, Makame VM, Mehl GL, Premji Z, Minjas JN, et al. Treatment practices for degedege, a locally recognized febrile illness, and implications for strategies to decrease mortality from severe malaria in Bagamoyo District, Tanzania. Trop Med Int Health. 1996 Jun;1(3):305–13. [ Links ]
16. Baume C, Helitzer D, Kachur SP. Patterns of care for childhood malaria in Zambia. Soc Sci Med. 2000 Nov;51(10):1491–503. [ Links ]
17. Njama D, Dorsey G, Guwatudde D, Kigonya K, Greenhouse B, Musisi S, et al. Urban malaria: primary caregivers' knowledge, attitudes, practices and predictors of malaria incidence in a cohort of Ugandan children. Trop Med Int Health. 2003 Aug;8(8):685–92. [ Links ]
18. Ryan GW. What do sequential behavioral patterns suggest about the medical decision-making process?: modeling home case management of acute illnesses in a rural Cameroonian village. Soc Sci Med. 1998 Jan;46(2):209–25. [ Links ]
19. Malik EM, Hanafi K, Ali SH, Ahmed ES, Mohamed KA. Treatment-seeking behaviour for malaria in children under five years of age: implication for home management in rural areas with high seasonal transmission in Sudan. Malar J. 2006 Jan;5:60. [ Links ]
20. Foster SD. The distribution and use of antimalarial drugs: not a pretty picture. In: London School of Hygiene and Tropical Medicine First Annual Public Forum, editor. Malaria: Waiting for the Vaccine. London: John Wiley & Sons; 1991. p. 123–40. [ Links ]
21. Djimde A, Plowe CV, Diop S, Dicko A, Wellems TE, Doumbo O. Use of antimalarial drugs in Mali: policy versus reality. Am J Trop Med Hyg. 1998 Sep;59(3):376–9. [ Links ]
22. Blair S, Lacharme LL, Carmona Fonseca J, Tobón A. Resistencia de Plasmodium falciparum a tres fármacos antimaláricos en Turbo (Antioquia, Colombia), 1998. Rev Panam Salud Publica. 2001;9(1):23–9. [ Links ]
23. Osorio L, Gonzalez I, Olliaro P, Taylor WRJ. Artemisinin-based combination therapy for uncomplicated Plasmodium falciparum malaria in Colombia. Malar J. 2007 Jan;6:25. [ Links ]
24. DANE Departamento Administrativo Nacional de Estadística. Censo general 2005: perfil Turbo Antioquia [Internet]. DANE. 2010;Available from: http://www.dane.gov.co/files/censo2005/PERFIL_PDF_CG2005/05837T7T000.PDF [ Links ]
25. Gutiérrez LA, Naranjo NJ, Cienfuegos AV, Muskus CE, Luckhart S, Conn JE, et al. Population structure analyses and demographic history of the malaria vector Anopheles albimanus from the Caribbean and the Pacific regions of Colombia. Malar J. 2009 Jan;8:259. [ Links ]
26. Silva Barrera M, Robayo Vásquez BI, editors. Atlas de Colombia. Bogotá D.C: IGAC Instituto Geográfico Agustín Codazzi; 2007. [ Links ]
27. Secretaría Seccional de Salud y Protección Social de Antioquia. Eventos de salud pública [Internet]. Secretaría Seccional de Salud y Protección Social de Antioquia. 2011 (cited 2011 Oct 15);Available from: http://www.dssa.gov.co/index.php/estadisticas/eventos-de-salud-publica [ Links ]
28. Creswell J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 3rd ed. Los Angeles: SAGE; 2009. [ Links ]
29. Cropley L. The effect of health education interventions on child malaria treatment-seeking practices among mothers in rural refugee villages in Belize, Central America. Health Promot. Int. 2004;19(4):445–52. [ Links ]
30. Roll Back Malaria Partnership. Global Malaria Action Plan. Geneva: Roll Back Malaria Partnership; 2008. [ Links ]
31. Rojas Álvarez DP. Evaluación de la eficacia terapéutica y la tolerabilidad de las combinaciones fijas de Artesunato-Amodiaquina y Artemeter-Lumefantrina para el tratamiento de la malaria por P. Falciparum no complicada en el departamento del Chocó,. Universidad Nacional de Colombia; 2010. [ Links ]
32. Bosman A, Mendis KN. A major transition in malaria treatment: the adoption and deployment of artemisinin-based combination therapies. Am J Trop Med Hyg. 2007 Dec;77(6 Suppl):193–7. [ Links ]
33. Reformas sanitarias e impacto del control de malaria en dos áreas endémicas de Colombia, 1982-2004. Colomb. Med. 2007;38(2):113–31. [ Links ]
34. Vélez M. Salud: negocio e inequidad, quince años de la Ley 100 en Colombia. Bogotá D.C: Ediciones Aurora; 2008. [ Links ]
35. Modelo de control de malaria en el departamento de Antioquia: estudio de casos. Rev Salud Publica. 2004;6(1):64–79. [ Links ]