CASE REPORT
A 33-year-old woman was admitted with pleuritic chest pain, a febrile episode of 38.5 ºC and several days of progressive dyspnea. Her medical history was unremarkable, except for occasional shortness of breath and two syncopal episodes associated with exercise. Low blood pressure (80/60 mm Hg), tachycardia (100 beats per minute) and a systolic heart murmur along the left upper edge of the sternum were found on physical examination.
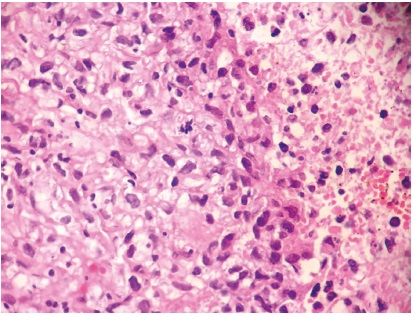
She had sinus tachycardia on electrocardiography, higher values of serum dimerized plasmin fragment D (D-dimer) (5000 ng/mL) and an enlarged pulmonary artery with mild cardiomegaly on the chest X-ray. The cardiac ultrasonographic study showed a 5.5 cm x 2.4 cm mass on the out-flow tract of the right ventricle, occluding 85 % of the main pulmonary artery and causing pulmonary valve insufficiency and pulmonary hypertension (systolic pulmonary pressure of 55 mm Hg). The CT scan revealed a large filling defect with little enhancement, which obstructed the main pulmonary artery and its right branch, with heart involvement and moderate pericardial effusion (Figure 1).
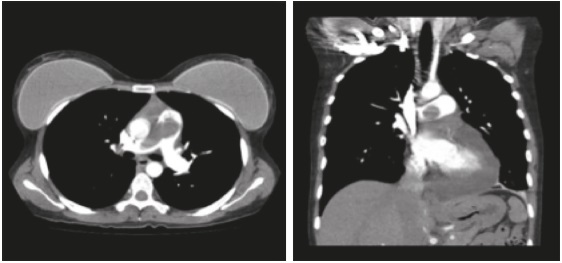
Figure 1 CT scan shows heart involvement, moderate pericardial effusion, and filling defect obstructing the main pulmonary artery and right branch
An acute pulmonary embolism was initially considered, and anticoagulation with thrombolytic therapy was suggested. However, some clinical symptoms (a few months with dyspnea and syncope) and findings (pulmonary hypertension) could not be explained by an acute pulmonary embolism. A chronic thromboembolic pulmonary hypertension could explain both, but the absence of previous deep vein thrombosis, and medical pro-thrombotic conditions, as well as the absence of typical radiological features (pouch defects, webs, bands, intimal irregularities, lobar or segmental involvement), were arguments against it. Her symptoms, ultrasonographic findings, mild contrast enhancement of the mass, apparent myocardial involvement, and pericardial effusion, suggested a neoplastic origin.
The patient was taken to surgery, but a complete resection was not possible, due to extensive myocardial and pericardial involvement; only biopsies were taken. Histopathologic examination revealed areas of necrosis, large round cells, eosinophilic cytoplasm, pleomorphic nuclei and atypical mitoses. Immunohistochemical findings were consistent with an intimal sarcoma of the pulmonary artery (Figure 2). After the intervention, the patient started neoadjuvant chemotherapy and was last seen seven months later.
COMMENT
Primary neoplasms of the pulmonary circulation are extremely rare. Pulmonary artery sarcoma is a rare tumor that often is mistaken for pulmonary thrombus, due to the similarities of their signs and symptoms; both can progress to pulmonary hypertension and both have similar radiological findings. This normally leads to a delayed diagnosis1)(2)(3. After the first case reported by Mandelstamm in 1923, a few cases have been described, mostly on autopsy. Mean age of presentation has been around fifty years, with a slight preference for females (1.3 to 1)4. According to World Health Organization (WHO), there are three types of sarcoma of large blood vessels: angiosarcoma, leimyosarcoma and intimal sarcoma3. Intimal sarcomas have a predominant intraluminal polipoyd growth pattern, often obstructing the lumen of the vessel of origin2. Yet the clinical presentation is variable; patients usually have a long asymptomatic course. Symptoms like chest pain, dyspnea, cough, pre-syncope and syncope are non-specific and usually the result of an obstructive phenomenon, while fever, weight loss, anemia, hemoptysis, clubbing and increased erythrocyte sedimentation rate are associated with the neoplastic behavior. On physical examination a systolic heart murmur over the pulmonary valve, and signs of right heart failure can be found. Because of the nonspecific symptoms and rarity, many cases are misdiagnosed as pulmonary thromboembolism and treated inappropriately1. The absence of deep venous thrombosis, negative results of procoagulant changes and the lack of response to anticoagulant therapy should be valued3.
Chest X-ray may be normal or may be show cardiomegaly, pulmonary hypertension, hilar enlargement, infiltrates, nodules or cavitations4. Echocardiographic findings include right ventricle enlargement, pulmonary hypertension, and obstruction of outflow tract, main pulmonary artery or branches by a pedunculated mass4)(5)(6. Filling defects on CT scan are similar to those of acute or chronic thromboembolism, with or without nodules, or with a mosaic pattern as result of tumor emboli. Yi and collegues7 have reported that CT findings favor the diagnosis of pulmonary artery sarcoma when they include low-attenuation filling defect occupying the entire luminal diameter of the proximal or main pulmonary artery, usually accompanied by expansion of the involved arteries or extraluminal tumor extension1)(2)(3)(7. Gadoliniumenhanced MRI has been described as the most useful method for diagnosis, showing enhancement of the intra-luminal mass due to necrosis, or bleeding2)(3)(4, distinguishing it from pulmonary embolism. PET scan can also differentiate between tumor and acute or chronic thromboembolism, and is useful to follow response to therapy, evaluating tumor metabolic activity4.Dias and colleagues8 reported two cases to emphasize the importance of F-fluorodeoxyglucose PET as a non-invasive method for the diagnostic investigation of patients whose presentation on CT of contrast filling defects in the pulmonary artery is atypical for thromboembolism. Treatment is early surgery, preferably with pulmonary endarterectomy, and success depends on the extent of resection. These tumors arise from the intima and rarely extend to the adventitia to invade surrounding structures, so resection might result in complete removal. Because the tumor often involves vital cardiac structures such as the pulmonary valve (30 % of cases), radical surgery resection can be challenging2. Prognosis, however, is still poor, with mean survival of around 10 months for those who undergo surgery, and 6 weeks for those who do not4)(5.
Neo-adjuvant chemotherapy might shrink the tumor and thereby enable its resection. However, in the event of initial misdiagnosis and severe right ventricular dysfunction requiring immediate surgery, there might not be time for it2. Adjuvant chemotherapy and radiation therapy are recommended for the eradication of any residual tumor foci2.