Introduction
Weaning and disconnection from mechanical ventilation (MV) are important processes in the intensive care unit (ICU), and approximately 10% to 20% of patients fail extubation and/or progress to prolonged weaning1,2. The weaning process is the transition from artificial ventilation to spontaneous ventilation. For the timely recognition of the onset, strategies such as weaning protocols and the use of spontaneous breathing trials (SBT) have been suggested3. The optimization of weaning preparation requires a comprehensive approach for the patient to transition to spontaneous breathing2,4. Performing a SBT helps identifying patients who can be successfully liberated from ventilatory support5. In critical patients with mechanical ventilatory support, bed rest, prolonged MV, and the use of neuromuscular blockers are suggested risk factors for ICU-acquired muscle weakness (ICUAW), which has been shown to increase the number of days of MV, days of hospitalization, mortality, and morbidity, among others6-8.
The use of non-invasive diagnostic tests has been reported to identify the compromise of peripheral and respiratory muscle strength in critical patients. These tests evaluate respiratory muscle strength through maximal inspiratory and expiratory pressure (MIP and MEP, respectively) in the mouth sustained for one second, and overall strength of the peripheral musculature with hand dynamometry (handgrip strength), with diagnostic cut-off points ICUAW (less than 11 kg for men and 7 kg for women)9,10. Moreover, the study by Cottereau et al.11 found that handgrip strength at the first SBT was associated with difficult or prolonged weaning (p-value = 0.004), and the recent study by Fontela et al.12 reported that handgrip strength was an accurate measure to identify ICUAW.
Despite the importance that evaluation of muscle strength in critically ill patients has acquired to date, there is a lack of studies that describe these measurements in the ventilatory weaning process as support in clinical decision-making. Hence, our objective was to determine the relationship between the strength of the handgrip and that of the inspiratory muscles with the success of SBT in adult patients with ventilatory support for more than 48 hours.
The relevance of the results of this research in the field of physiotherapy in critical care is related to the importance of using valid and reliable measurements to identify patients with ICUAW -or with risk factors for acquiring it- and planning interventions that favor ventilatory weaning and functional recovery of patients.
Methodology
This was an observational cross-sectional prospective study performed in an adult ICU between November 2015 and October 2016. We included 18-year-old patients and older, with time on MV greater than 48 hours, with Richmond Agitation-Sedation Scale (RASS) score 0 to -1 and who met criteria to perform SBT according to the protocol established in the general ICU. Patients were excluded if they had acute or chronic neuromuscular disease, delirium, tracheostomy, or burns or amputations of the hand. A convenience sampling was considered, including all the patients who met the selection criteria during the study period.
Measurement protocol
Two trained physiotherapists performed the handgrip strength and MIP measurements once daily immediately before the first SBT test, which lasted 30 or 120 min (Figure 1). The inter-rater reliability of the dynamometry measurement was evaluated. The patients had to meet the weaning criteria established in the institution's protocol and the SBT was performed according to international guidelines13.
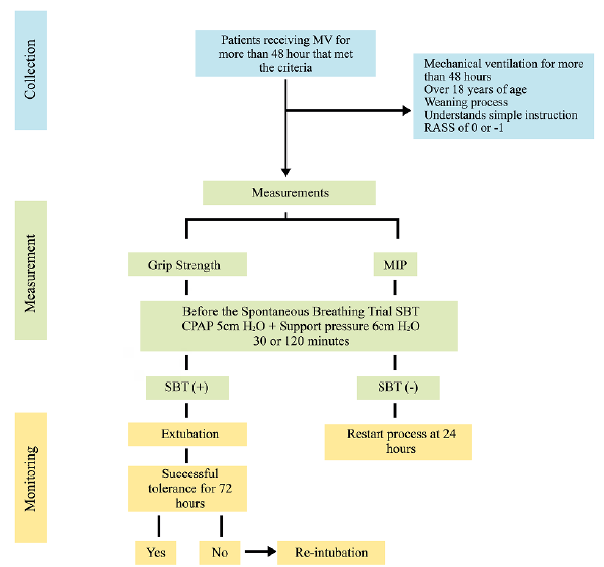
Figure 1 Measurement protocol. SBT: Spontaneous breathing trial, MV: Mechanical ventilation, RASS: Richmond Agitation-Sedation Scale, CPAP: Continuous positive airway pressure, MIP: Maximal inspiratory pressure.
The Human Ethics Committee of the Universidad del Valle approved this study (# 156-015) and according to Article 11 of Resolution 008430 of the Ministry of Health and Social Protection of Colombia, it was considered as a study with a risk higher than the minimum. The ethical principles for medical research involving human subjects stated in the Declaration of Helsinki were considered in the development of this study. Patients selected signed an informed consent.
The ICU interdisciplinary team was unaware of the measurement results and the decision to extubate was based on the SBT result and the patient's clinical condition. If the SBT failed, the process was restarted after 24 hours, if the SBT was positive, extubation proceeded.
The handgrip strength was performed with a previously calibrated hand dynamometer (Smedley Digital Hand Dynamometer, Model: 12-0286), following the protocol of Ali et al.10, patient in a sitting position on the bed, back 90°, leaning on the back passively, shoulder adducted, elbow flexed to 90°, wrist neutral, feet supported, it was explained to the patient that he should grasp the instrument with the greatest possible force with the dominant hand and hold it for 6 seconds,10 three measurements were made and the highest value was recorded. To classify the ICUAW, the cut-off points of Ali et al.10 (11 kg for men and 7 kg for women) were taken.
The MIP measurement was performed with a Brazilian industry record mechanical vacuum manometer, following the recommendations of the American Thoracic Society14. Before starting the SBT, the patient was placed in a sitting position with elevation of the head to 45°, trunk and head aligned. They were disconnected from the ventilator, the vacuum manometer was connected, and they were instructed to take a maximal inspiration from the residual volume. Three measurements were made with rest intervals of 2 min and the highest value was recorded. To classify the inspiratory muscle strength, the cut-off points of the American Thoracic Society and the European Respiratory Society of -15 to -30 cmH20 were used14,15.
The characteristics of the population (age, sex, medical diagnosis, the Acute Physiology Score II (Apache II)), were recorded on admission to the ICU. The level of sedation, the duration of the MV until the SBT, the results of the measurement of the handgrip strength and MIP, the type of weaning, the time of the SBT, and the reasons for the failure of extubation, were also recorded.
To ensure the validity of the handgrip strength measurement procedure, the intra-rater reliability was determined using the Intraclass Correlation Index (ICC). For the interpretation, the Landis and Koch classification was used16. ICC higher than 0.95 was classified as excellent. Rater 1: ICC 0.955, (CI: 0.920 -0.977); Rater 2: ICC 0.987, (CI: 0.976 - 0.99); Rater 3: ICC: 0.992, (CI: 0.985 - 0.996).
Statistical analysis
For the analysis and statistical graphics, the R-Gui 4.0 program and Excel 2016 were used. For the description of the clinical characteristics of the patients, the measures of central tendency were used with their respective dispersion measure as the standard deviation (SD), and absolute frequencies and percentages (%) were used, according to the type and distribution of each variable. To find possible relationships between the quantitative variables (handgrip strength and MIP), the Pearson correlation was used. The assumption of normality was previously validated using the Shapiro Wilk test. To identify the presence of association between qualitative (SBT) and quantitative variables, Cohen's D test was used. (Cohen suggests the following interpretative rule: absolute values of d, between 0.2 and 0.5 would indicate a low intensity of the association (effect size); between 0.5 and 0.8 mean; while, from 0.8, high)17.
Results
Clinical characteristics of the patients
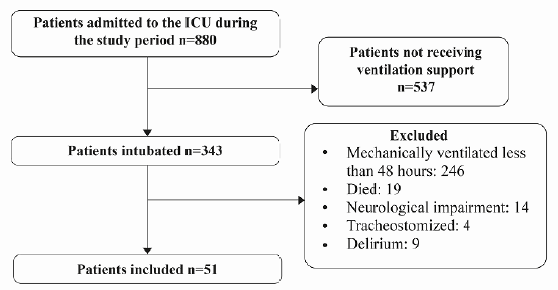
During the data collection period, 880 patients were admitted to the ICU, 343 had MV, of which 292 were excluded. The study sample consisted of 51 patients. Figure 2.
Table 1 describes the clinical characteristics of the patients, 57% were male and the mean age was 54 ± 20. Sepsis was the most prevalent reason (27.5%) for admission to the ICU. Regarding the type of weaning, we found 84.3% simple and 15.7% prolonged.
Table 1 Clinical characteristics of patients
aSD: Standard deviation; bICU: Intensive care unit; cAPACHE: Acute physiology and chronic health evaluation; dMIP: maximal inspiratory pressure; eSBT: Spontaneous breathing trial; fRASS: Richmond agitation-sedation scale.
Relationship between inspiratory muscle strength and handgrip strength
Inspiratory muscle weakness was identified in 14.2% of the population, with a minimum value of -10 cmH20 of MIP for the females and -6 cmH20 for the males, and in 25.5% ICUAW was identified, with a value minimum 3.2 kg for females and 2.8 kg for males (cut-off points (11 kg for men and 7 kg for women). Figure 3 shows the positive relationship between handgrip strength and MIP, indicating that greater handgrip strength is associated to greater MIP.
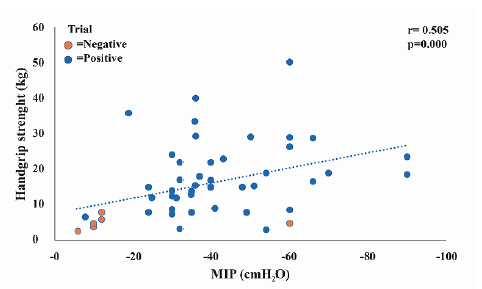
Figure 3 Handgrip strength (Kg) and Maximal inspiratory pressure (MIP) (cmH2O) vs. the outcome of the spontaneous breathing trial (SBT).
To determine the existence of association between qualitative and quantitative variables, Cohen's D test was used, finding that between the MIP and the SBT result, the relationship was high (d 1.29), as well as between the handgrip strength and the result of the SBT (d 1.23).
When adjusting the Pearson correlation taking the result of the SBT as the response variable and the explanatory variables the result of the MIP and the handgrip strength, it was identified that the most significant variable to predict the result of the SBT was the handgrip strength. A negative relationship was identified between the result of the handgrip strength with the days of stay in the ICU (r -0.403; p <0.05) and with the days of MV (r -0.208; p> 0.05). The relationship between the MIP result and the days of ICU stay was negative with statistical significance (r -0.453; p<0.05), and for the days of MV it was also negative without significance (r -0.262; p > 0.05).
Discussion
The objective of this study was to determine the relationship between manual grip strength and inspiratory muscle strength with the success of the SBT in adults with ventilatory support for more than 48 hours, and the results showed a positive correlation. This suggests that the use of objective and reliable measurements for the early identification of ICUAW could allow earlier initiation of therapeutic interventions that favor ventilatory weaning.
The evidence supports that the ICUAW is associated with a prolongation of MV for up to eleven days, in addition to contributing to failure in ventilatory weaning, for which the assessment of peripheral and respiratory muscle strength in a reliable and valid way, is increasingly relevant, to identify patients with weakness or risk factors for acquiring it17. Handgrip strength evaluated with dynamometry, has been used as a tool to diagnose ICUAW, as a predictor of mortality, as a predictor of weaning, and as an indicator of nutritional status9-11,18,19. In this study, handgrip strength was measured with dynamometry and normal strength with positive SBT was identified in 74.5% of the patients.
Muscle activation requires alert state and active collaboration of the patient. This situation reflected in the patients of this study, who were awakened early, which could suggest that these actions facilitated voluntary movement, and together with physiotherapy activities, could explain preservation of respiratory and peripheral muscle strength20,21. Ali et al.10 compared the handgrip strength with the Medical Research Council (MRC) scale in critically ill patients, finding a high correlation (Pearson = 0.96, p <0.001) and defined the cut-off points (11 kg men and 7 kg women), with 80% sensitivity and 83.2% specificity10. In this regard, in the present study, using the same protocol and cut-off points, ICUAW was identified in 25.5% of the patients.
Cottereau et al.11 conducted a prospective study in two ICUs and evaluated the grip strength in 86 patients on MV for at least 48 hours, before each SBT, the authors found a relationship between grip strength and weaning from difficult or prolonged MV and the stay in the ICU, but not with the result of extubation11. In the present study, the relationship between the grip strength with the success of the SBT was investigated, finding a positive relationship with the MIP and with the handgrip strength, which could suggest that in daily practice, MIP or handgrip strength can be used to identify patients with ICUAW and define the performance of SBT.
In the present study, it was considered that despite the good reliability reported in handgrip strength measurements in critically ill patients, it should be complemented with respiratory muscle strength measurements, considering that MV is a factor that compromises respiratory muscle performance. Efstathiou et al.22 evaluated the relationship between handgrip strength and MIP in young healthy and middle-aged individuals, finding a significant correlation (Pearson 0.76; p<0.001). We consider that although the results of Efstathiou et al.22 are not comparable with those of our investigation, the respiratory and peripheral muscles can behave in a similar way; however, further studies should be carried out in critical patients, which justifies measuring both muscle groups.
Tzanis et al.9 investigated the development of ICUAW using MIP as a surrogate parameter for MRC score, reporting a significant correlation between MIP and MRC score (r = 0.68, p<0.001) and establishing a cutoff point of 36 cmH2O for MIP (88% of sensitivity, 76% specificity)9. These authors, unlike the present study, did not measure handgrip strength and MIP was measured 48 hours after the cessation of sedation9. The cut-off point for MIP established by Tzanis et al.9 is high, when compared to those suggested by the American Thoracic Society and the European Respiratory Society (-15; -30 cmH2O, respectively)14 which were used in this study.
Cut-off points for the MIP in critically ill patients in our population are currently unknown, for which the ones recommended by the American Thoracic Society and European Respiratory Society were used14, which are traditionally the most used, and higher average values were identified. So, it was considered that the above could be related to differences in anthropometric characteristics, which suggests the need to identify cut-off points in our population. Considering this, we highlight the need for new investigations in this field that address this issue.
The findings of the present study identified a relationship between the handgrip strength and the days of stay in the ICU with statistical significance (r = -0.403 p<0.05), suggesting that the days of stay in the ICU might impact the ICUAW, and that early mobilization activities can be a strategy to improve functional recovery during prolonged critical illness, decreasing the onset of ICUAW, and the hospital stay23,24.
The limitations of this study are related to the performance in a single institution and the absence of nutritional assessment and anthropometric analysis. The presence of edema was considered a confounding factor since there was no validated scale available to measure it objectively. Moreover, the methodological strengths of the study are related to the inter-rater reliability of the dynamometry measurement and the quality control during the data collection and analysis processes.
Future experimental studies that evaluate the impact of early mobilization in the ICU on the improvement of manual grip strength and respiratory muscles are recommended.
Conclusions
Handgrip strength and MIP were positively correlated with SBT success. According to our results, we suggest that if the result of the handgrip strength is within normal ranges, the SBT can be performed. If the result is below the cut-off points, it should be complemented with a MIP measurement and if the MIP measurement is low, the diagnosis of ICUAW might be considered. If the result of the grip strength is below the normal low ranges and the MIP is normal, it is suggested to eliminate confounding factors and perform a test.