Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Facultad de Odontología Universidad de Antioquia
versión impresa ISSN 0121-246X
Rev Fac Odontol Univ Antioq vol.23 no.2 Medellín ene./jun. 2012
CASE REPORT
Oral telangiectatic granuloma. Case series presentation
Jonathan Harris Ricardo1; Ary López Álvarez2; Kery Romero Gómez3
1 D.D.S., Universidad del Sinú. Specialist in Stomatology and Oral
Surgery. Universidad de Cartagena. Candidate to Magister in Molecular
Microbiology, Universidad Libre. Professor of Oral Surgery, Corporación
Universitaria Rafael Núñez
2 D.D.S., Universidad de Cartagena. Specialist in Oral Implantology,
Universidad Católica Argentina. Professor, Corporación Universitaria
Rafael Núñez.
3 Undergraduate dental student at Corporación Universitaria Rafael Núñez
SUBMITTED: MAY 24/2011 - ACCEPTED: FEBRUARY 28/2011
Ricardo JH, López A, Romero K. Oral telangiectatic granuloma. Case series presentation. Rev Fac Odontol Univ Antioq 2012; 23(2): 366-375.
ABSTRACT
Telangiectatic granuloma is a benign hyperplastic lesion that results from trauma or local irritation. When it is present in the oral cavity, it appears as a fast growing red tumor with spontaneous bleeding, and it occurs more frequently in the vestibular gingiva of the maxillary anterior region. It`s a common pathology in South America, with cases in Argentina, Brazil, Chile, and Colombia. It is important for dentists to know its etiological factors, as well as the clinical and histological features for correct diagnosis and proper treatment. A series of four cases with diagnosis of telangiectatic granuloma is reported in this article.
Key words: telangiectatic granuloma, oral surgical procedures, dental plaque.
INTRODUCTION
The oral cavity is often exposed to traumatic and irritating lesions that produce tissue response, especially by the soft tissues.
The gingiva, oral mucosa, lips and tongue are the areas most affected by these lesions.1 The oral telangiectatic granuloma (OTB), formerly called pyogenic granuloma, is a benign inflammatory hyperplastic lesion that affects the skin and the oral mucosa, and appears as a response to local trauma or chronic irritation creating a repair tissue (granulation) produced by the body as a defense mechanism.2
This condition is very common in South American countries; Gordon, Vasconcelos et al, in 2010, published a study of 293 cases of OTB in a Brazilian population;3 Duarte, Vallejos et al, in 2006, reported 12 cases in Argentina;4 Espinoza, Rojas et al, in 2003, in Chile, reported 62 cases in patients over 65 years of age.5 In the Colombian geographical area its incidence is high since there are multiple case reports: Jiménez et al, in 2006, published a retrospective analysis of 9.023 oral pathology cases in Medellín and reported 375 cases with OTB, out of which 262 were females;6 there were also cases reported in Cartagena de Indias by authors like Díaz, Vergara et al, in 2009,7 and Rebolledo, Harris et al, in 2010.8
The etiology of this disease is related to aspects such as presence of bone spicules, use of orthodontic appliances, root fragments, gingival irritation and plaque or calculus, to name just a few. Several authors claim that its etiology is largely related to traumatic factors, or to local irritants that seem to be associated to hormonal female sex changes, as it appears especially in puberty and pregnancy, altering tissue response thus enabling the appearance of granulation tissue.9, 10
Clinically, it is characterized by a red tumorous lesion, whose size varies from a few millimeters to a larger size and occupies a big part of the oral cavity, its surface may be smooth or rough, and the surface of some of the affected areas may also be ulcerated, especially the ones that are in constant trauma. Its base can be sessile or pedunculated, with a soft consistency and is likely to bleed copiously when manipulated. It may occur at any age, and is most frequently found in females, most often affecting the vestibular gingiva of the maxillary upper anterior region.11, 12
The histologic examination shows granulation tissue with chronic inflammatory infiltration composed of polymorphonuclear neutrophils and endothelial tissue, underneath the epithelium there is proliferation of small thin-walled blood vessels surrounded by loose connective tissue. Its center usually presents signs of necrosis, but not in all the cases.13, 14 The differential diagnosis includes peripheral giant cell granuloma, peripheral fibroma, and Kaposi's sarcoma, which present some clinical similarities such as lesion type, color, location and evolution, also with a capillary hemangioma since it shows a similar histological pattern and spontaneous bleeding.9, 15
TREATMENT
The initial treatment seeks to intercept and eliminate the local etiologic factor that is associated to OTB and to perform plaque control, removal of faulty restorations, and elimination of periodontal pockets. After these initial treatment steps, decrease in lesion size may be observed. Among the treatment alternatives, the use of CO2 laser, cryosurgery and the application of acidic substances have been used in recent years. Such substances produce precipitation and protein denaturation of the microorganisms involved in the pathology. But the most effective therapy is surgical removal reaching the periosteum and removing the entire base of the lesion, with root planing and dental extractions if needed.16-18 Surgical removal is usually performed in pregnant women after childbirth and it is only performed during pregnancy if the lesion causes significant functional impairment or profuse bleeding, because the rate of recurrence is higher during pregnancy.19
This article will present a series of four cases with a diagnosis of telangiectatic granuloma in patients treated at the Stomatology and Oral Surgery Department of Corporación Universitaria Rafael Núñez Dental Clinics. Being this a common disease in our geographical area, it is very important to know its etiologic factors, as well as its clinical and histological features, for correct diagnosis and treatment.
CASE 1
A 17-year-old female patient presented an asymptomatic oral cavity tumor-like lesion with four months of evolution, interfering with the articulation of words, spontaneous bleeding when brushing and progressively increasing over time. Family history reveals grandmother on the father's side with high blood pressure, and no personal relevant clinical history. The exploration of organs and significant systems showed normal conditions.
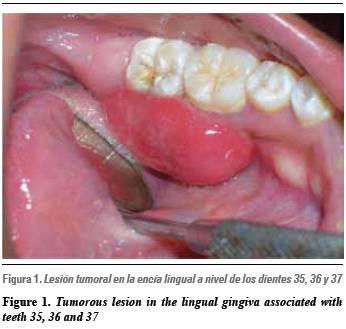
The Intraoral examination revealed a tumor at the lingual gingiva of teeth 35, 36 and 37, with an approximate size of 2.5 cm in diameter, red, smooth, with a pedunculated base, soft consistency, and plenty of supragingival plaque and calculus (figure 1). The clinical diagnosis was telangiectatic granuloma, the preoperative laboratory test results reported normal values and therefore it was scheduled for surgery. Three days before the surgical procedure, a hygienic session was performed and brushing techniques were demonstrated.
Procedure
Anesthetic was applied to the lingual margin an incision was performed at the base of the lesion with a scalpel blade and handle N.° 15. Bard Parker # 3, the measures taken were to scrape the entire area, also the teeth adjacent to the lesion; the specimen was removed and placed in a specimen jar filled with formaldehyde at 10%. Immediately after, a hemostasis was performed subsequently ordering analgesic and antibiotic therapy for seven days. Postsurgical: 8 days after the procedure, the soft tissue showed positive results, 6 months after surgical procedure there was no recurrence.
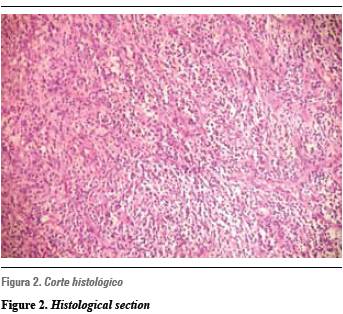
The microscopic histopathology study reported tissue fragments with stratified squamous epithelium and no atypia, partially ulcerated, whose lamina propria presented a proliferation of small vessels, surrounded by abundant inflammatory cells of the neutrophils lymphoma type (figure 2). The specimen was negative for malignancy and was consistent with telangiectatic granuloma.
CASE 2
A 52 year-old female patient presented a tumorous asymptomatic lesion in the gingiva, with three months of evolution, and spontaneous bleeding when brushing and chewing. This tumorous lesion rapidly increased in size. Family and personal history is irrelevant to the case. Exploration of organs and significant systems revealed normal conditions.
Upon intraoral examination a tumor was detected, located in the marginal gingiva and vestibularly attached to the tooth 21; it was of a bright red color, 1 cm in diameter, with irregular surface, pedunculated base and soft consistency. Presence of plaque around tooth 21 and occlusal wear of anterior teeth were observed (figure 3). The clinical diagnosis was telangiectatic granuloma, the preoperative laboratory test results reported normal and it was scheduled for surgery. Three days before the surgical procedure a hygienic session was performed and brushing techniques were demonstrated.
Procedure
An infraorbital anesthesia technique was applied on the left side and an incision was performed at the base of the lesion followed by curettage of the affected area, scraping and root planing of tooth 21. The pathological sample was removed and placed in a specimen jar filled with formaldehyde at 10% and hemostasis was performed ordering analgesic and antibiotic therapy for seven days. Postsurgical care: eight days after the procedure the soft tissue showed positive results, and nine months later no recurrence occurred.
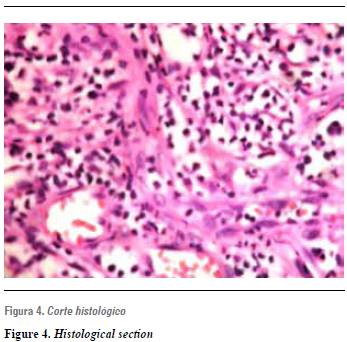
The microscopic histopathological description consisted of tissue fibrocollagen proliferation, highly vascularized, with chronic inflammatory cells of the polymorphonuclear neutrophils type, and ulcerated areas. It was negative for malignancy and showed no atypia. Also, it was compatible with telangiectatic granuloma (figure 4).
CASE 3
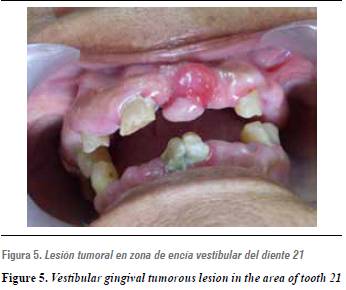
Female patient age 59, who presented an asymptomatic tumorous lesion in the gingiva, with two months of evolution, easily and rapidly bleeding and fast growing. Family history: father has diabetes; personal history is not relevant to the case and the examination of organs and systems did not show any significant alterations.
During clinical examination, an intraoral tumor was observed, located in the marginal gingiva and attached to the vestibular zone of tooth 21; it was of a bright red color in some areas and pale pink in other areas. Its measurement was 1.5 cm in diameter, with smooth surface, pedunculated base, firm consistency, and presence of generalized bacterial plaque and multiple root remains in tooth 21, which was located near the area of the tumor (figure 5). The clinical diagnosis was telangiectatic granuloma, the preoperative laboratory test results reported normal activity and it was scheduled for surgery. Four days before the surgical procedure, a hygienic session was performed and brushing techniques were demonstrated.
Procedure
Infraorbital and nasopalatine taeniacide anesthesia was applied. An incision was made at the base of the lesion, and tooth 21 was extracted; then surgery was performed to remove tissue in the affected area (curettage), the pathological sample was included in a specimen jar at 10% and hemostasis was finally, analgesic and antibiotic therapy was prescribed for seven days. Postoperative care: eight days after the procedure there was appropriate healing of the scar/ soft tissue, extractions of the remaining root fragments were performed and the patient was referred to oral rehabilitation for dental prostheses. After a year of surgery, no recurrence has occurred.
The microscopic histopathological description revealed vascular proliferation, chronic inflammatory tissue, and ulcerated areas, without atypia or malignancy. It was compatible with telangiectatic granuloma.
CASE 4
Female patient, age 62, presented an asymptomatic tumorous lesion on her lip, with one month of evolution, spontaneous bleeding, and progressively increasing in size. The patient reported a dental prosthesis change one month earlier and often biting her lip; family history is not relevant in this case, and personal clinical history revealed high blood pressure controlled with medication, diet and exercise. Examination of organs and systems showed normal conditions.
While conducting the intraoral examination, a tumor was observed, located in the lower lip mucosa, with 9 mm in diameter. It was red in some areas and pale pink in other areas, smooth, with a pedunculated implantation base, and soft consistency on palpation. The patient was totally edentulous, with fixed devices used as anchors for the dentures (figure 6). Clinical diagnosis: telangiectatic granuloma, the preoperative laboratory test results reported normality and surgery was scheduled.
Procedure
An infiltrative anesthetic technique was applied around the lession, an incision was made at the base of the tumor, the pathological sample was placed in a jar with formaldehyde at 10% and hemostasis was performed, finally analgesic and antibiotic therapy was ordered for seven days. Postoperative care: eight days after the procedure there was good healing of scar/soft tissue, the patient was referred to oral rehabilitation to prevent the cause of frequent biting of her lower lip, which is produced by the dental prosthesis and the prosthetic restoration. After eight months of surgery there was no recurrence.
The microscope histopathology study reported hyperplastic tissue degranulation, endothelial proliferation, and a vascular network with a great amount of chronic inflammatory cells infiltrated without atypia, partially ulcerated and negative for malignancy. It was compatible with telangiectatic granuloma.
DISCUSSION
Telangiectatic granuloma is described as a localized reactive lesion caused by a given stimulus that produces excessive connective tissue; it is frequently found in the oral cavity, usually affecting areas such as gingiva, lips and alveolar mucosa.9
Gordon, Vasconcelos et al., in a 2010 retrospective study in a Brazilian population that included 293 cases of OTB, found out more prevalence in women, with a 2,38:1 ratio. The most frequent target was the gingiva (83%), most cases were asymptomatic and presented spontaneous bleeding. The lesions were described as having a red surface (73.2%), soft consistency (62.3%) and a pedicular base (61.1%); the average lesion size was 1.3 cm.3 All of these characteristics were found in the present series of four cases, in which 100% of the patients were females, in three cases the affected area was the gingiva, and all the cases presented lesions of red color, soft pediculate consistency, spontaneous bleeding, and they were all asymptomatic.
Diaz et al in 2009 and Zhang et al in 2007 reported local irritants such as dental plaque and calculus, chronic trauma, foreign bodies in the tissues, and overhanging margins of the crowns, just to name a few, as OTB etiological factors,7, 20 thus agreeing with the present series, in which the first three cases presented dental plaque and calculus as associated etiologic factors, while in the fourth case the causal factor was trauma.
Regarding OTB treatment, Al-Khateeb and Ababneh confirmed that oral hygiene, surgical excision, curettage of the lesion base to decrease the frequency of recurrence, accompanied by antibiotic and analgesic therapy is the most accurate treatment, and reported that among 85 patients who were in postoperative follow up in a range of 2 to 12 years, only five of them had recurrences;21 similar results are shown in this series of cases, which also were subjected to surgical excision, curettage at the base of the injury and medical therapy with antibiotics and analgesics, presenting no recurrences so far.
CORRESPONDING AUTHOR
Jonathan Harris Ricardo
Programa de Odontología
Corporación Universitaria Rafael Núñez
Centro Avenida Escallón, Pasaje la Moneda. Local 111
Cartagena, Colombia
Correo electrónico: j.harris.r@hotmail.com
REFERENCES
1. Al-Zayer M, Da Fonseca M, Ship JA. Pyogenic granuloma in a renal transplant patient: case report. Spec Care Dentist 2001; 21(5): 187-190. [ Links ]
2. Patil K, Mahima VG, Lahari K. Extragingival pyogenic granuloma. Indian J Dent Res 2006; 17(4): 199-202. [ Links ]
3. Gordon-Núñez MA, de Vasconcelos M, Benevenuto TG, Lopes MF, Silva LM, Galvão HC. Oral pyogenic granuloma: a retrospective analysis of 293 cases in a Brazilian population. J Oral Maxillofac Surg 2010; 68(9): 2185-2188. [ Links ]
4. Espinoza I, Rojas R, Aranda W, Gamonal J. Prevalence of oral mucosal lesions in elderly people in Santiago, Chile. J Oral Pathol Med 2003; 32(10): 571-575. [ Links ]
5. Duarte S, Vallejos R, Briend M, Rosende C. Investigación retrospectiva de granulomas telangiectásicos. Rev Fac Odont Univ Nord 2006; M009. [ Links ]
6. Jiménez R, Alejandro L. Análisis retrospectivo de 9.023 informes de patología bucal en la Facultad de Odontología de la Universidad de Antioquia, Medellín, Colombia. 1972-2003. Rev Fac Odontol Univ Antioq 2006; 17(2): 19-25. [ Links ]
7. Díaz A, Vergara C, Carmona M. Granuloma telangiectásico en cavidad oral. Reporte de un caso clínico. Av Odontoestomatol 2009; 25(3): 131-135. [ Links ]
8. Rebolledo M, Harris J, Cantillo O, Carbonell Z, Díaz A. Granuloma telangiectásico en cavidad oral. Av Odontoestomatol 2010; 26(5): 249-253. [ Links ]
9. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci 2006; 48(4): 167-175. [ Links ]
10. Amirchaghmaghi M, Falaki F, Mohtasham N, Mozafari PM. Extragingival pyogenic granuloma: a case report. Cases J 2008; 1(1): 37. [ Links ]
11. Gonçales ES, Damante JH, Rubira CM, Taveira LA. Pyogenic granuloma on the upper lip: an unusual location. J Appl Oral Sci 2010; 18(5): 5385-5341. [ Links ]
12. De Souza AG, Da Silva BC, Israel MS, Lindenblatt R, De Andrade AM, Ramos ME. Atypical location of pyogenic granuloma in two pediatric patients. Gen Dent 2008; 56(5): 447-450. [ Links ]
13. Bakshi J, Virk RS, Verma M. Pyogenic granuloma of the hard palate: a case report and review of the literature. Ear Nose Throat J 2009; 88(9): E4-E5. [ Links ]
14. Ababneh KT. Biopsied gingival lesions in northern Jordanians: A retrospective analysis over 10 years. Int J Periodontics Restorative Dent 2006; 26(4): 387-393. [ Links ]
15. Vergara CI, Díaz A, Arévalo L. Granuloma periférico de células gigantes. Reporte de un caso. Rev Fac Odontol Univ Antioq 2010; 22(1): 117-121. [ Links ]
16. Zarei MR, Chamani G, Amanpoor S. Reactive hyperplasia of the oral cavity in Kerman province, Iran: a review of 172 cases. Br J Oral Maxillofac Surg 2007; 45(4): 288-292. [ Links ]
17. Giblin AV, Clover AJ, Athanassopoulos A, Budny PG. Pyogenic granuloma-the quest for optimum treatment: audit of treatment of 408 cases. J Plast Reconstr Aesthet Surg 2007; 60(9): 1030-1035. [ Links ]
18. Kirschner RE, Low DW. Treatment of pyogenic granuloma by shave excision and laser photocoagulation. Plast Reconstr Surg 1999; 104(5): 1346-1349. [ Links ]
19. Silva-Sousa YT, Coelho CM, Brentegani LG, Vieira ML, de Oliveira ML. Clinical and histological evaluation of granuloma gravidarum: case report. Braz Dent J 2000; 11(2):135-9. [ Links ]
20. Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: a retrospective analysis of 108 cases. J Oral Maxillofac Surg 2003; 61(11): 1285-1288. [ Links ]
21. Zhang W, Chen Y, An Z, Geng N, Bao D. Reactive gingival lesions: a retrospective study of 2,439 cases. Quintessence Int 2007; 38(2): 103-110. [ Links ]











 texto en
texto en