Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Facultad de Odontología Universidad de Antioquia
Print version ISSN 0121-246X
Rev Fac Odontol Univ Antioq vol.24 no.1 Medellín July/Dec. 2012
ORIGINAL ARTICLES DERIVED FROM RESEARCH
ORAL HEALTH PROFILE AND DENTURE STATUS OF BIMAXILLARY EDENTULOUS PATIENTS TREATED AT UNIVERSIDAD DE ANTIOQUIA'S SCHOOL OF DENTISTRY: A PILOT STUDY1
Jenny A. Moreno Castillo 2, Andrés F. Montoya Sepúlveda 2, Diana P. Gómez Gil2, Alejandro Arboleda Cadavid 2, Francisco J. Zea Restrepo 3, Andrés A. Agudelo Suárez4
1This study was conducted as an academic exercise of the first
four authors at Universidad de Antioquia's Undergraduate Dentistry
Program.
2 Senior Dentistry Students, Universidad de Antioquia.
3 Dentist. Specialist in Comprehensive Dentistry of the Adult; professor
at the School of Dentistry, Universidad de Antioquia. Email address:
fjzearpo@hotmail.com
4 Dentist. Specialist in Health Services Administration. Ph.D. in Public
Health. Assistant Professor, School of Dentistry, Universidad de
Antioquia, Medellín, Colombia. Email address:
oleduga@gmail.com
SUBMITTED: NOVEMBER 8/2011-ACCEPTED: FEBRUARY 29/2012
Moreno JA, Montoya AF, Gómez DP, Arboleda A, Zea FJ, Agudelo AA. Oral health profile and denture status of bimaxillary edentulous patients assisted at Universidad de Antioquia's School of Dentistry: A pilot study. Rev Fac Odontol Univ Antioq 2012; 24(1): 22-36.
ABSTRACT
INTRODUCTION: the main objective of this study was to analyze oral health conditions and denture status of a sample
of bimaxillary edentulous patients treated at the adult clinic of Universidad de Antioquia's School of Dentistry.
METHODS this was a descriptive study on 54 patients seeking consultation between 2008 and 2010. The following variables were considered: age, gender,
socioeconomic level, education level, frequency of brushing, mouthwash use, mucosa cleansing, nightly removal of prosthesis, presence
of stomatitis, ulcers, fibrous increase, porosities, pigmentations, calculi, fractures, lost teeth, dental wear, and level of satisfaction with
the prosthetics apparatus. These variables were described by gender and Chi Square tests in order to observe statistical significances.
RESULTSmost of the studied population come from lower socioeconomic groups and have low education levels. 48% of this population
presented some kind of upper arch stomatitis. 46% of them remove both prostheses at night, with a greater proportion among women
(58%). Calculi were the most important finding in terms of denture status, as it occurred in 79% of lower prostheses. Almost 80% of the assessed population was satisfied with the upper denture, while 44% were satisfied with the lower one.
CONCLUSIONS:the findings suggest lack of care and control of these patients' situation, as well as deficiencies in terms of hygiene habits on both the mouth and the
prosthesis —a situation that does not match the high levels of satisfaction found.
Key words: full denture, oral health, edentulous mouth, oral hygiene.
INTRODUCTION
Despite all the efforts and multiple campaigns to promote oral health,1 caries and periodontal diseases are still highly prevalent in Colombia and the world.2, 3Moreover, the percentage of people who have lost most or all of their natural teeth is still high.4 For these patients, losing teeth represents a great motivation to seek dental services in order to obtain a functional set of teeth and a socially acceptable esthetic aspect.5-7 Similarly, it is important to consider that the elderly population increases 1.7% every year and according to estimations by the year 2025 there will be 1.100 million people over 60 years in the world.8, 9
In Colombia, according to figures from the III Estudio Nacional de Salud Bucal (1998), presence of prosthesis in the upper maxilla occurs in 25.8% of the population, and only 7% of patients have lower maxilla prosthesis, more frequently in the ages of 55 years and over. Out of the people who use prosthesis in the upper maxilla, 41.1% present full denture, while 49.9% have it in the lower maxilla. The use of full denture was most frequently observed among the adult population over 55 years, and even more in both maxillaries arches. The need of full denture is greater in the case of the upper maxilla, 5.2%, compared to 3.3% in the mandible.2
Nevertheless, in spite of the magnitude and severity of the problem, nowadays totally edentulous patients do not receive comprehensive treatment by dentists, as conventional full removable dentures are adapted to them and in very few occasions patients are inquired about their stomatological condition or their prosthesis status after insertion.10
Alterations of these patients' oral mucosa, such as ulcers, fibrous increase, and stomatitis in its three stages are some of the conditions most commonly found in relation to the use of full dentures.11-13 Scarce information is available on topics such as identification of the frequency with which such alterations occur or establishing their relation with prosthesis status14-16in terms of porosities, pigmentations, calculi, fractures, lost teeth, or dental wear, or simply observing the importance given by patients to hygiene of their prostheses or mouths.17-19
Therefore, further follow-up studies are required to guarantee patients better adaptation to their prostheses and a better quality of life while using them.20 This information will serve as reference to clinicians and students in terms of diagnosis, prognosis, treatment plan and supervision of these patients. Conventional removable full dentures are therefore still an excellent alternative for rehabilitation of edentulous patients, so this kind of research must be encouraged among undergraduate and graduate students.21
Consequently, the main objective of this study was to analyze the oral health conditions and denture status of a sample of bimaxillary edentulous patients treated at the adult clinic of Universidad de Antioquia's School of Dentistry.
MATERIALS AND METHODS
This was an exploratory, descriptive, cross-sectional study. A convenience sample was selected from patients who had previously been installed conventional removable full dentures. Inclusion criteria considered all the patients who consulted Universidad de Antioquia's School of Dentistry during the period 2008-2010 and who had bimaxillary prostheses installed; patients with monomaxillary prosthesis were excluded, as well as those who had not used the installed prosthesis at the institution (in one or both maxillaries) or who did not accept to participate in the study.
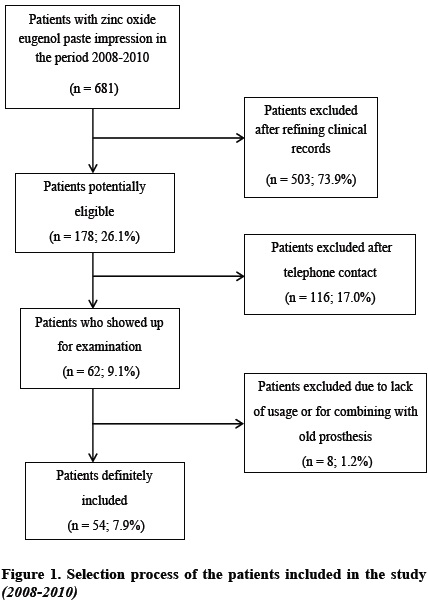
Sample selection implied consulting the database provided by the institution's administrative section, considering those patients who had an impression taken with zinc oxide eugenol impression material in order to construct a prosthesis during the time of study (although there are other impression materials available, such as silicones or polyesters, most of the patients treated at the School of Dentistry are applied zinc oxide eugenol paste due to its qualitycost ratio). Initially, 681 patients were included in the study. Once the data had been refined by revising the patients' clinical records, 178 patients were selected. After telephone contact, 62 patients accepted to participate. Clinical examinations were performed and 8 patients were dismissed, mostly because they did not use the installed prosthesis. The final sample contained 54 patients. Figure 1 shows the process of selection of the studied population.
The socio-demographic variables included: sex, actual age (= 60, 61-70, = 71), education level (none/ primary school, secondary school, technical/technological/ college), time since prosthesis installation, in months (= 12, 13-24, = 25), socioeconomic level (1, 2, 3, 4, 5, 6), and satisfaction with upper and lower prosthesis (satisfied, somehow satisfied, unsatisfied). The variables related to oral hygiene were: frequency of brushing, nightly removal of upper and lower prosthesis, mouthwash use, and mucosa cleansing. In terms of prosthesis status, these variables were assessed: presence of calculi, porosities, pigmentations, fractures, lost teeth, and dental wear. Finally, oral health status included evaluation of presence of ulcers, fibrous increase, and stomatitis (types I, II or III). A data collection instrument was devised and adjusted by means of a pilot test on a group of patients (n = 4) in order to evaluate the variables' internal consistency.
The variables were described, and analyses were performed for males and females separately. Chi square tests were performed in order to observe statistical significance in terms of percentage distribution, as well as Chi square for ratio differences according to sex. Data analysis was performed by using Excel® for Windows®, SPSS® 18.0 (Chicago IL. USA) and EPIDAT 3.1 (Dirección Xeral de Innovación e Xestión da Saúde Pública, Xunta de Galicia, España, Organización Panamericana de la Salud e Instituto Superior de Ciencias Médicas de La Habana).
This research project complied with Resolution 008430 of 1993, which includes the technical standard requirements for health research in Colombia, seeking confidentiality of the obtained data and informed consent to participate in the study. This study did not represent any kind of risk for the participants. The needs identified in terms of prosthesis adaptation, oral hygiene instructions, and stomatology variations were solved according to the protocols established in the School of Dentistry's clinic of the adult, with supervision by an expert professor. Patients requiring treatments of more complexity, such as prosthesis repetition, rebase, and teeth adaptation, were referred for further treatment at the School's clinic of the adult.
This study was approved as an academic exercise of the four first authors in the Dentistry Undergraduate Program at Universidad de Antioquia, Medellón, Colombia.
RESULTS
Table 1 shows the socio-demographic characteristics of the participants. In general, more than 70% are older than 61 years. More than half of them have had the prosthesis for more than two years, with more frequency among males, and with significant statistical differences (p < 0.05). Most of the population presents a lower education level (none/primary school): 92% of males, and 71% of females. Two thirds of males and two fifths of females live in houses of lower socioeconomic levels. In terms of degree of satisfaction with the full upper denture, almost 80% of the sample expressed being satisfied, especially the males; in relation to lower denture, almost half of the sample expressed being satisfied with it. The rest of the sample is similarly distributed as somehow satisfied and unsatisfied.
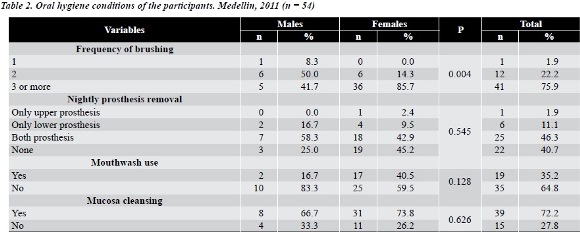
In terms of oral hygiene conditions of both prosthesis and mucosa (table 2), most of the population brush their teeth three or more times a day, with a higher tendency among females (statistically significant differences p < 0.05). In relation to nightly prosthesis removal, 46% of the patients remove both prostheses; this is true especially among females (58%). Also, more than a third of the population does not use any kind of mouthwash; males are the ones who less practice this habit (more than 80%). Almost three fourths of the patients said they usually cleanse their mucosa; similar percentage distribution is found among males and females.
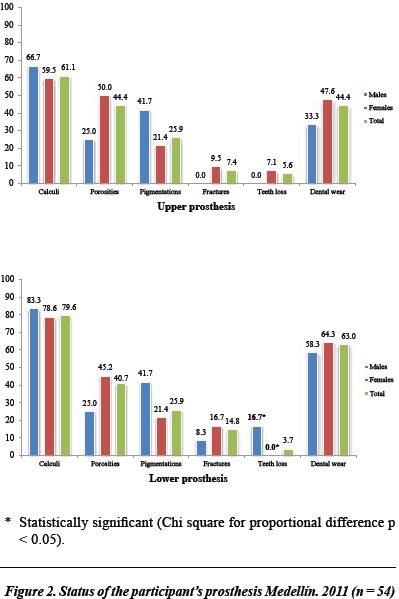
Evaluation of prosthesis status (figure 2) revealed a high percentage of calculus in both upper and lower prosthesis. Being more prevalent in males. Also, more porosity was found in the upper prosthesis of females and more pigmentation in both upper and lower prosthesis of males. The prosthesis with the most fractures were the lower ones. especially among females (17%); teeth lost occurred more frequently in males' lower prosthesis (significant differences p < 0.05) and in females' upper prosthesis. More than half of the lower prosthesis presented dental wear both in males and females.
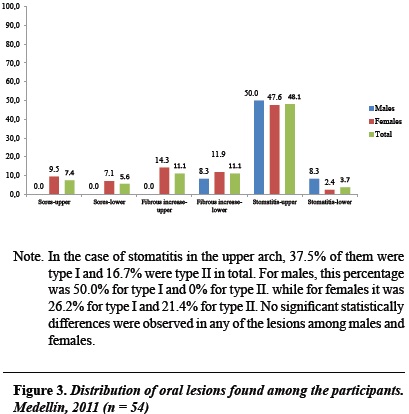
Finally, figure 3 presents information on oral lesions. No sores were found among males and among females the percentages are lower than 10%. Observations indicate that 11% of upper and lower edges presented fibrous increase. Almost half of the studied population presented stomatitis in the upper arch and one tenth of them in the lower arch (with no significant statistical differences among males and females).
figura 4 displays images of some of the patients in the study (status of mucosa and full dentures).
DISCUSSION
The main findings of this study account for the oral health situation of patients with removable conventional bimaxillary full denture as it evaluated not only prosthesis status but also other variables related to the oral conditions most commonly found in this population. This is one of the first studies on this topic carried out at Universidad de Antioquia.
Our study showed that a high percentage of the population is satisfied with their full upper denture due to the retention support and stability achieved on the area of contact with the palate while a greater number of the participants are unsatisfied with the lower prosthesis because of alveolar resorption as a natural aging process occurring at the lower edentulous maxilla.22 Nevertheless, the degree of satisfaction does not agree with clinical results found at the prosthesis themselves as on underlying tissues. This could be explained because these patients' perception of oral health is related to prosthesis adaptation only, leaving aside some important aspects such as care and hygiene both of the prosthetic apparatus and the stomatology structures.23
The high percentage of upper maxilla stomatitis may be connected to causes such as low frequency of prosthesis removal at night.24 Similarly, high prevalence of calculus in both upper and lower prosthesis was found not agreeing with the high brushing frequency reported by patients. This situation has been reported in previous studies which show that most prosthesis users do not receive sufficient instruction on oral health from their dentists.25 This could also be explained for the difficulties expressed by the elderly in terms of accomplishing adequate hygiene actions maybe because of lack of strength and autonomy.26
In comparison to other studies that included nightly prosthesis removal (which in this study was 52.8%). relative agreement was observed with Peracini et al (2010),25 who reported that 41.5% of the patients usually remove their prosthesis, while Evren et al (2011) informed that only 31% of them do.24
In terms of oral pathologies, some similarities are found, taking into account that according to Dóaz Martell et al (2007)27 sub-prosthesis stomatitis is the prevalent, with 35.3%, followed by sores with 33.8%, and fibrous increase with 27.9% —the two first ones being prevalent in females. On the other hand, Lemus Cruz et al (2009)28report stomatitis in 39.5%, sores in 4.7% and fibrous increase in 15.3%; Sotomayor Camayo et al (2002)29 report stomatitis in 33.3%, sores in 21.4% and fibrous increase in 16.7% (while the figures yielded by the present study are 25.9; 6.5, and y 11.1%, respectively).
In turn, the III Estudio Nacional de Salud Bucal (1998)2 reports that tissue increase due to prosthesis is the pathology with the most prevalence in the nation (with 3.9%) in comparison to other studied pathologies. It appears more frequently in adult people over 55 years of age, and more often among females. The prevalence of traumatic ulcers is 1.9%. It increases with age and is most common among males (provided that these pathologies have not been exclusively assessed in complete edentulous patients).
For analysis of these results it is important to bear in mind the limitations and strengths of this study. Even though this is a pilot study at the School of Dentistry having a convenience sample makes it difficult to generalize the findings to the population of Medellin. It is important to point out that this study becomes a reference framework for future studies. Although it yields important information on oral conditions and prosthesis status, further knowledge is required on other variables such as tobacco or alcohol consumption, medicine intake or systemic diseases that may alter the stomatognathic system in an attempt to assess associations among different oral health conditions and some risk factors. Among the study's strengths it is important to highlight the contribution of experts in thematic and methodological issues as well as the careful selection of variables for the study and its subsequent calibration in order to ensure agreement among examiners. Also the data collection tools were analyzed by means of a pilot test which allowed assessing internal consistency.
Health personnel-training institutions that use the teaching-service outreach model as a base to assist patients usually lack follow-up appointments to allow permanent education and constant assessment of the changes that may occur not only in tissues but also in prosthetics apparatuses.30-32 .All of this is important since most of these patients come from the lowest socioeconomic groups, who usually experience limitations to accessing health services; therefore, these institutions become points of reference to the elderly population when lacking treatments not included in Colombia's General System of Social Security33, 34
Incorporating supervision and control strategies for patients using full dentures at Universidad de Antioquia's School of Dentistry as well as improving information systems for these patients would enable better clinical and epidemiological characterizations, and would build up a model to be replicated in other health organizations and education institutions.
ACKNOWLEDGEMENTS
We would like to thank the patients who unselfishly participated in this study, as well as Guillermo Flórez (administrative support) for facilitating the database of the School's patients and professor Hugo Sánchez Fajardo for his advice during the process of research subject design.
CORRESPONDING AUTHOR
Jenny A. Moreno Castillo
Francisco J. Zea Restrepo
Facultad de OdontologÍa
Universidad de Antioquia
Calle 64 N.° 52-59. MedellÍn, Colombia
Phone number: +57 (4) 219 67 40
Email addresses: jelexa001@gmail.com;
fjzearpo@hotmail.com
REFERENCES
1. Organización Mundial de la Salud. Centro de Prensa. Salud Bucodental. Nota informativa N.° 318. Febrero de 2007. Ginebra: OMS; 2007. [ Links ]
2. Colombia. Ministerio de Salud. III Estudio Nacional de Salud Bucal ENSAB III. Bogotá: El Ministerio; 1998. [ Links ]
3. Reyes Obediente F, Espeso Nápoles N, Hernández Suárez A. Promoción de salud bucal en la tercera edad en un centro comunitario de salud mental. Arch Méd Camaguey [revista en línea]. 2009 [fecha de acceso 7 de junio de 2011]; 13(3). URL disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttextpid=S1025-02552009000300002Ing=es [ Links ]
4. Unfer B, Braun K, Pafiadache C, Pereira F, Dias L. Autopercepção da perda de dentes em idosos. Interface 2006, 10(19): 217-226. [ Links ]
5. Matus López P. Salud oral. En: D'Hyver C, Gutiérrez Robledo LM. GeriatrÍa. México: Manual Moderno; 2006. p. 335-347. [ Links ]
6. Locker D, Clarke M, Payne B. Self-perceived oral health status, psychological well-being, and life satisfaction in an older adult population. J Dent Res 2000; 79(4): 970-975. [ Links ]
7. Vergés Callard E, Corona Carpio M, Pineda RodrÍguez A, López RodrÍguez B. Causes of rejection of total prostheses in the older adult. Rev Cubana Estomatol [revista en lÍnea]. 2007 Dic; [fecha de acceso 16 de junio de 2011]; 44(4) URL disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttextpid=S0034-75072007000400008lng=es [ Links ]
8. MarÍn Zuluaga D. Influencia de la boca en la calidad de vida de los ancianos. Encuentro Internacional de Terapia Neural 2003. Bogotá, Colombia [revista en lÍnea]. [fecha de acceso mayo 25 de 2011] URL disponible en: http://www.terapianeural.com/index.php?option=com_content&task=view&id=161&Itemid= [ Links ]
9. EcheverrÍa P, Roldán M. Rehabilitación del paciente edentado. MedellÍn: Universidad de Antioquia; 1997. [ Links ]
10. Reyes R, Merchant R. OdontogeriatrÍa: parte integral del tratamiento en ancianos. Archivo Geriátrico 1999; 2(2): 53-56. [ Links ]
11. Hidalgo Hidalgo S, Ramos DÍaz MJ, Fernández Franch N. Alteraciones bucales en pacientes geriátricos portadores de prótesis total en dos áreas de salud. Arch Méd Camaguey [revista en lÍnea]. 2005 [fecha de consulta 16 de junio de 2011]; 9(6) URL disponible en: http://redalyc.uaemex.mx/src/inicio/ArtPdfRed.jsp?iCve=211117924001 [ Links ]
12. Bagan J, Scully C. Medicina y PatologÍa Oral. Valencia: Medicina Oral; 2006. [ Links ]
13. Lazarde J. Estomatitis Subprotésica. Acta Odontol Venez 2001; 39(3): 9-17. [ Links ]
14. Arias A. Diagnóstico de las patologÍas de los tejidos blandos en mujeres con prótesis parcial o total removible. Rev Estomat 2001; 9(2): 21-29. [ Links ]
15. Boucher C, Zarb G, Bolender C, Hickey J, Carlsson G. Prostodoncia total de Boucher. México: Interamericana; 1994. [ Links ]
16. Sáez C, Carmona M, Jiménez Z, Alfaro X. Oral changes in the older adult. Rev Cubana Estomatol [revista en lÍnea]. 2007 [fecha de consulta 13 de julio de 2011]; 44(4) URL disponible en: http://search.scielo.org/?q=cambios%20bucales%20en%20adulto%20mayorwhere=ORG [ Links ]
17. Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. J Dent Educ 1990; 54(11): 680-687. [ Links ]
18. Kulak Ozkan Y, Kazazoglu E, Arikan A. Oral hygiene habits, denture cleanliness, presence of yeasts and stomatitis in elderly people. J Oral Rehabil 2002; 29(3): 300-334. [ Links ]
19. Marchini L, Tamashiro E, Nascimento DF, Cunha VP. Self-reported denture hygiene of a sample of edentulous attendees at a University dental clinic and the relationship to the condition of the oral tissues. Gerodontology 2004; 21(4): 226-228. [ Links ]
20. MacEntee MI. Quality of life as an indicator of oral health in older people. J Am Dent Assoc 2008; 139(3): 252-253. [ Links ]
21. Carlsson G, Omar R. The future of complete dentures in oral rehabilitation. A critical review. J Oral Rehabil 2010; 37: 143-156. [ Links ]
22. Zarb G, Schmitt A. Implant therapy alternatives for geriatric edentulous patients. Gerodontology 1993; 10(1): 28-32. [ Links ]
23. Slade GD, Sanders AE. The paradox of better subjective oral health in older age. J Dent Res 2011; 90(11): 1279-1285. [ Links ]
24. Evren BA, Uludamar A, Iseri U, Ozkan YK. The association between socioeconomic status, oral hygiene practice, denture stomatitis and oral status in elderly people living different residential homes. Arch Gerontol Geriatr 2011; 53(3): 252-257. [ Links ]
25. Peracini A, Machado de Andrade I, Oliveira Paranhos H, Lovato da Silva CH, Freitas de Souza R. Behaviors and hygiene habits of complete denture wearers. Braz Dent J 2010; 21(3): 247-252. [ Links ]
26. Ávila Funes J, Garant M, Aguilar Navarro S. Relación entre los factores que determinan los sÍntomas depresivos y los hábitos alimentarios en adultos mayores de México. Rev Panam Salud Púteblica 2006; 19(5): 321-330. [ Links ]
27. DÍaz Martell Y, Martell Forte I, Zamora DÍaz JD. Afecciones de la mucosa oral encontradas en pacientes geriátricos portadores de prótesis estomatológicas. Rev Cuba Estomatol [revista en lÍnea] 2007 [fecha de consulta 3 de octubre de 2011]; 44(3) URL disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttextpid=S0034-75072007000300002lng=es [ Links ]
28. Lemus Cruz LM, Triana K, Valle Selenenko O, Fuertes RufÍn L, Sáez Carriera R. Rehabilitaciones protésicas y su calidad como factor de riesgo en la aparición de lesiones en la mucosa bucal. Rev Cuba Estomatol [revista en lÍnea] 2009 [fecha de consulta 3 de octubre de 2011]; 46(1): URL disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttextpid=S0034-75072009000100003lng=esnrm=iso [ Links ]
29. Sotomayor Camayo J, Pineda MejÍa ME, Luis Gálvez Calla L, de la Cruz Castillón A. Alteraciones clÍnicas de la mucosa bucal en personas de la tercera edad portadoras de prótesis totales. Odontología Sanmarquina 2002; 1(10): 17-22. [ Links ]
30. Felton D, Cooper L, Duqum I, Minsley G, Guckes A, Haug S et al. Evidence-based guidelines for the care and maintenance of complete dentures: a publication of the American College of Prosthodontists. J Am Dent Assoc 2011; 142 Supl 1: 1S-20S. [ Links ]
31. Jagger DC, Harrison A. Denture cleansing-the best approach. Br Dent J 1995; 178(11): 413-417. [ Links ]
32. Polyzois GL. Denture cleansing habits. A survey. Aust Dent J 1983; 28(3): 171-173. [ Links ]
33. Colombia. Congreso de la Repúteblica. Ley 100 de 1993 por la cual se crea el Sistema de Seguridad Social Integral y se dictan otras disposiciones. Bogotá: El Congreso; 1993. [ Links ]
34. Colombia. Ministerio de la Protección Social. Plan Obligatorio de Salud (POS). Bogotá: El Ministerio; 2009. [ Links ]











 text in
text in