Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Facultad de Odontología Universidad de Antioquia
versión impresa ISSN 0121-246X
Rev Fac Odontol Univ Antioq vol.25 no.2 Medellín ene./jun. 2014
ORIGINAL ARTICLES DERIVED FROM RESEARCH
FACTORS ASSOCIATED TO ENDODONTICALLY TREATED TOOTH SURVIVAL IN PATIENTS OVER 20 YEARS OF AGE SEEN IN A PRIVATE IPS BETWEEN 2006 AND 2012
Eliana Pineda Vélez1, Ángela María Segura Cardona2
1 Dentist, Endodontics specialist, Magister in Epidemiology. Undergraduate Professor, Universidad de Antioquia, Medellín, Colombia. Email: elipineda1@gmail.com
2 Ph.D. in Epidemiology. Professor, Universidad CES, Medellín, Colombia
SUBMITTED: MAY 14/2013-ACCEPTED: JUNE 30, 2013
Pineda E, Segura AM. Factors associated to endodontically treated tooth survival in patients over 20 years of age seen in a private IPS between 2006 and 2012. Rev Fac Odontol Univ Antioq 2014; 25 (2):.
ABSTRACT
INTRODUCTION: endodontics is the branch of dentistry that studies the morphology, function, and alterations of the dental pulp and periodontal region, as well as their treatment. Success rates in endodontics are usually high but survival has not been thoroughly studied. The objective of this study was to determine survival time and clinical and demographic factors influencing endodontically treated teeth loss.
METHODS: this was a cohort follow-up study with survival analysis in order to assess the status of endodontically treated teeth based on systematic collection of information obtained from medical records.
RESULTS: we found a population with low income and with technical or vocational education; males were predominant in this population. Extraction or tooth loss occurred earlier in males, and even earlier in those with lower income and apical lesions larger than 11 mm.
CONCLUSION: having a tooth with an apical lesion larger than 11 mm significantly explains earlier dental loss.
Key words: endodontics, survival, dental extraction.
INTRODUCTION
Dental treatment plans often imply the decision of keeping one of the teeth, which is influenced by success of the endodontic treatment by a 90%, as the literature demonstrates. 1, 2
In endodontically treated teeth survival, Lazarski et al observed only a 5% loss in teeth with endodontic treatment due to extraction, with no difference between students and professionals and an overall success rate of 94% after 3-5 years post-treatment.3 However, an important aspect was evaluated by Friedman, who showed that treating teeth with periapical inflammation, as evidenced by periapical radiopacity, decreases success.4
Caplan and Weintraub reported five factors that were used to predict endodontically treated teeth loss in a period of 6-8 years: age, history of facial trauma, missing molars (not third molars), high plaque levels, and less than two proximal contacts on the endodontically treated tooth at the time of intrumenting5
The objective of this study was to assess endodontically treated tooth survival, as well as associated clinical and demographic factors.
METHODS
This study intended to associate clinical and socio-demographic factors with tooth survival after root canal treatment. The study was performed between 2006 and 2012, systematically collecting information from medical records and including tooth permanence in the oral cavity as factor of interest..
We took all the dental records of patients who underwent root canal treatment and were treated in an endodontics referral center in Medellín during a minimum follow-up of 6 months. This information was saved in a Microsoft Excel® spreadsheet with a predefined form. The data were gathered taking into account the inclusion criteria and sorted out according to the study's variables in such a way that the unit of analysis were teeth with endodontic treatment.
Summary measures, and relative and absolute frequencies were used in the descriptive analysis. The independence Χ2 test and Fisher's exact test were used to establish associations between the dependent variable (tooth loss) and qualitative, socio-demographic, and clinical factors as independent variables. In addition, measures of association (raw OR) were calculated, with their respective 95% confidence intervals (95% CI).
Overall survival was calculated using the Kaplan-Meier analysis, and curves were compared through the Log Rank Test. For multivariate analysis, we used the Cox proportional hazards model for explanatory purposes, where raw measures of association or hazard radio (HR) (loss versus time) were obtained and adjusted.
Those patients who did not present the factor of interest (tooth extraction) at the end of the study were considered has having no loss (censoring). The time variable were the months since the endodontic treatment until extraction or until the end of the follow-up period. Data systematization, processing and analysis was performed using SPSS, version 21.
Since the data used came from clinical records, this study is classified as a research project with no biological, physiological, psychological or social risks for patients, according to Ministry of Health Resolution 8430 of 1993,6 title II, article 11.
RESULTS
The total study population was 811 patients, with an average age of 40.6 years (12,0 SD); 50% of patients were 40 years or over, the older being 91 years. 61.7% were women, and the predominant socio-economic level was that of "less than two minimum legal wages", with 87.1% of participants under this category.
The most common occupation was that of technical or professional, with 15.2%, followed by housewife, 12.1%, auxiliary, 11%, and various trades, 9.1%. In analyzing the dental conditions of patients 20 years old or over, we found out that 22.4% presented tooth loss. The most frequent dental diagnosis was asymptomatic apical periodontitis, with 64.9%; concerning tooth type, the most frequent were posterior teeth, with 86.8%. During the follow-up period, 62.5% of participants saw the specialist (an endodontist) once and 27.5% did so on two occasions. The most frequent lesion size was 10 mm or less, with 89.4% in this age group (table 1).
Concerning participants over 20 years of age, we found out that the only variable associated with tooth loss was lesion size (p < 0,05), so that patients with lesions 11 mm or larger present 12.18% risk of losing teeth. The diagnosis variable also presented association (p < 0,05) with predominance of pulp necrosis, with a 2.26% risk of losing teeth (table 2).
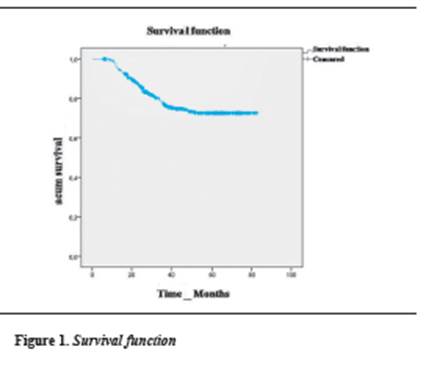
Kaplan-Meier Survival Analysis shows that tooth loss is evident from month six, and the probability of not losing teeth until month 17 is 92.3%. The average survival was 67,02 months (figure 1).
In comparing the time of tooth loss with the following variables: sex, age, economic status, lesion size, diagnosis, number of appointments, and tooth type, the only variables with significant values were lesion size and diagnosis (table 3).
According to the model, patients with lesions 11 mm or larger lost their teeth 6.1 times faster than those with lesions smaller than 10 mm. Adjusting by the other variables in the model, the speed of tooth loss was 8.92 times faster than in smaller lesions, and this difference was statistically significant (HR 8.92; 95% CI 6.02-13.21) (table 4).
DISCUSSION
This study evaluated tooth survival after endodontic treatment and the association of clinical and socio-demographic factors influencing faster tooth loss or extraction.
Tooth loss can have significant impact on the patient's dental function and physiology, and although the lost tooth may be replaced by an implant, the endodontically treated tooth maintains the proprioception mechanism, which is lost with the implant. Therefore, patients who have their teeth also have better jaw control. In addition, implant treatment involves separated evaluations by different specialists, multiple visits, and a variety of x-rays, so in analyzing endodontic treatment cost versus implant cost, the latter might be 70 to 400% higher than root canal treatment with coronal restoration. On the other hand, patients who require implants may need more interventions, compared with those who receive endodontic treatment.
For many patients and professionals, endodontic therapy is then the first treatment option and is still valid for the dental profession, so all kind of knowledge about success and prognosis will benefit the discipline and the patient's well-being.7-9 It must be taken into account, in addition, that epidemiological data on the frequency and distribution of endodontically treated teeth reflect the need and the demand for this procedure.10, 11
Advances in endodontics have increased the percentage of successful treatments, which is between 70 and 95% when performed by specialists, and between 64 and 75% when performed by general dentists. That is why operator qualification is among the prognostic factors for survival after endodontic treatment12, 13—but this is not a relevant factor in this study since the treatments were by performed a specialist.
This study showed that women are the population portion that most often consults (61.7%), possibly for being more patient to attend controls. With respect to the age factor, we found out that the average age was 40.6 years, in a population over 20 years of age earning less than two minimum wages as personal income and with professional/technical education. This characterizes this population, and no other survival studies have been done, probably because the countries' social security scheme has not been considered important, or economic capacity is not considered as a factor that effects treatment and therefore the permanence of teeth in the oral cavity.
These conditions suggest that most patients lack resources to pay costly restorations of prosthetic type in case of coronal fracture or tooth structure weakening as a result of endodontic treatment. The clinical characterization shows higher prevalence of chronic apical periodontitis with a lesion smaller than 10 mm, attended on a single appointment for treating a posterior tooth, with dental loss or extraction of about 22.4% for the total population aged 20 years.
Dental loss varies with patient's age and gender; similarly, these factors influence the presence of caries and periodontal disease—major causes of such loss—.9, 11 As for social aspects, more teeth are lost in men with lower income, working as operators. These findings cannot be contrasted with other studies because they do not include this type of characterization. In terms of clinical aspects, we found out that performing endodontic treatment of posterior teeth in two sessions offers greater risk of tooth loss in patients with lesions larger than 11 mm (12.18 times tooth loss risk compared to patients with smaller injuries), this being a statistically significant finding.
Caplan and Weintraub5 studied the association of clinical factors in order to predict treatment outcome, finding out that the higher the amount of adjacent lost teeth the higher the plaque index, and not placing restoration after treatment leads to higher probability of tooth loss. Additionally, in terms of apical radiopacity, a larger size decreases treatment success; in general, they find that posterior teeth are more often lost than the anterior ones. The present study also found out that greater apical radiopacity, as well as dealing with a posterior tooth, are conditions for greater tooth loss—agreeing with other studies.4, 5, 14
Endodontic therapy offers high long-time survival rates2, 13, 15, 16 as shown in this study, in which univariate Kaplan-Meier Survival Analysis shows that tooth loss starts from month six, and the probability of not losing teeth until month 17 is 92.3%. In addition, tooth loss happens more rapid among men, with similar survival rates among the different income levels. In terms of lesion size, patients with lesions larger than 11 mm lost tooth faster, showing a significant difference with the group of lesions smaller than 10 mm, which showed no difference in the number of appointments.
In a multivariate analysis, Eckerbom et al17 note that teeth with periapical pathology are more probably lost between 5-7 years than those with no lesions. They also identified variables that predict endodontically treated teeth loss, such as the number of proximal contacts, patient's age, the number of teeth already lost, and facial trauma history. They also found out that teeth with two proximal contacts were lost three times less than those with one contact or no contact at all; coronal restoration had no significance in the bivariate analysis.
The multivariate survival model used for the present study included the following variables because of their significance: sex, age, socioeconomic level, lesion size, number of appointments, and type of tooth. According to Cox regression, tooth loss or extraction occurred earlier in men than in women and even faster in those with lower income. This was very similar to what happened when analyzing the independent variable, as teeth with apical lesions larger than 11 mm were lost more quickly.
CONCLUSIONS
This was an adult population in productive age with low income, technical or vocational education and with predominance of women, seeking endodontic therapy as a way of not losing their teeth or extending permanence in the mouth.
In terms of socio-demographic factors, we can conclude that there is more tooth loss among men between 40 and 49 years and over 80 years of age, usually with low income. Occupation showing more tooth loss is operator.
Concerning the clinical factors associated with tooth loss, patients with lesions larger than 11 mm lose their teeth more often than those with smaller lesions; similarly, those who require several appointments lose their teeth more often than those requiring a single session.
Tooth loss or extraction happens earlier in men in the group of 40 to 49 years of age, and even earlier among those with lower income and with apical lesions larger than 11 mm.
In the absence of health plans with total coverage, the patients should pay for the cost of prosthetic restorations. We suggest conducting this study in patients with other social characteristics, in order to determine how this can affect endodontically treated tooth loss.
CONFLICTS OF INTEREST
The authors declare not having conflicts of interest.
REFERENCES
1. Alley BS, Kitchens GG, Alley LW, Eleazer PD. A comparison of survival of teeth following endodontic treatment performed by general dentists or by specialists. Oral Sur.Oral Med Oral Pathol Oral Radiol Endod 2004; 98(1): 115-118. [ Links ]
2. Caplan DJ, Kolker J, Rivera EM, Walton RE. Relationship between number of proximal contacts and survival of root canal treated teeth. Int Endod J 2002; 35(2): 193-199. [ Links ]
3. Lazarski MP, Walker WA III, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J Endod 2001; 27(12): 791-796. [ Links ]
4. Friedman S, Mor C. The success of endodontic therapy--healing and functionality. J Calif Dent Assoc 2004; 32(6): 493-503. [ Links ]
5. Caplan DJ, Weintraub JA. Factors related to loss of root canal filled teeth. J Public Health Dent 1997; 57(1): 31-39. [ Links ]
6. Colombia. Ministerio de Salud. Resolución 8430 de 1993, octubre 4, por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá: El Ministerio; 1993. [ Links ]
7. Pennington MW, Vernazza CR, Shackley P, Armstrong NT, Whitworth JM, Steele JG. Evaluation of the cost-effectiveness of root canal treatment using conventional approaches versus replacement with an implant. Int Endod J 2009; 42(10): 874-883. [ Links ]
8. Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod 2008; 34(11):1302-1305. [ Links ]
9. Morris MF, Kirkpatrick TC, Rutledge RE, Schindler WG. Comparison of nonsurgical root canal treatment and single-tooth implants. J Endod 2009; 35(10):1325-1330. [ Links ]
10. Chen SC, Chueh LH, Hsiao CK, Tsai MY, Ho SC, Chiang CP. An epidemiologic study of tooth retention after nonsurgical endodontic treatment in a large population in Taiwan. J Endod 2007; 33(3): 226-229. [ Links ]
11. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod 2004; 30(12): 846-850. [ Links ]
12. Imura N, Pinheiro ET, Gomes BPFA, Zaia AA, Ferraz CCR, Souza-Filho FJ. The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod 2007; 33(11): 1278-1282. [ Links ]
13. Swartz DB, Skidmore AE, Griffin JA Jr. Twenty years of endodontic success and failure. J Endod 1983; 9(5): 198-202. [ Links ]
14. Byström A, Happonen RP, Sjögren U, Sundqvist G. Healing of periapical lesions of pulpless teeth after endodontic treatment with controlled asepsis. Endod Dent Traumatol 1987; 3(2): 58-63. [ Links ]
15. Dammaschke T, Steven D, Kaup M, Ott KHR. Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod 2003; 29(10): 638-643. [ Links ]
16. Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002; 87(3): 256-263. [ Links ]
17. Eckerbom M, Magnusson T, Martinsson T. Reasons for and incidence of tooth mortality in a Swedish population. Endod Dent Traumatol 1992; 8(6): 230-234. [ Links ]











 texto en
texto en