Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Facultad de Odontología Universidad de Antioquia
Print version ISSN 0121-246X
Rev Fac Odontol Univ Antioq vol.26 no.2 Medellín Jan./June 2015
ORIGINAL ARTICLES DERIVED FROM RESEARCH
CONDYLAR HYPERPLASIA: CHARACTERISTICS, MANIFESTATIONS, DIAGNOSIS AND TREATMENT. A TOPIC REVIEW
Diego Fernando López B1; Claudia Marcela Corral S2
1 Orthodontist. Orthodontics Professor in undergraduate and graduate programs, Universidad del Valle, Cali, Colombia, E-mail: dr.diegolopez10@gmail.com2 Intern of the third year of the Orthodontics Graduate Program, Universidad del Valle, Cali, Colombia.
SUBMITTED: APRIL 14/2013-APPROVED: MARCH 4/2014
López DF, Corral CM. Condylar hyperplasia: characteristics, manifestations, diagnosis and treatment. A topic review. Rev Fac Odontol Univ Antioq 2015; 26(21): 425-446.
ABSTRACT.
Condylar hyperplasia is a condition that affects not only the proportions and facial symmetry in patients, but also static and dynamic occlusion functions with repercussions in the masticatory activity, the health of the temporomandibular joint (TMJ), and the anatomy and volume of adjacent soft tissues. Therefore, according to its severity this disease concerns maxillofacial surgeons, orthodontists, physical therapists, plastic surgeons, and nuclear doctors, who are all closely involved in the diagnosis stage. Historically, diagnosis of condylar hyperplasia has been based on anamnesis and the initial physical examination of the patient, where asymmetry, malocclusion and in some cases temporomandibular disorders (TMDs) are detected and later confirmed with tests such as bone scan and eventually by pathology report once condylar surgery has been done. The purpose of this literature review is to provide detailed information on the behavior of this disease from the point of view of its etiology, clinical characteristics, and distribution by age, sex and affected condyle, as well as the necessary diagnostic and imaging aids for its diagnosis, differential diagnosis, associated diseases, histological characteristics of the affected tissues, and the different therapeutic approaches according to severity, patient's age, and active or inactive form of the condition. The information was obtained from scientific research articles in different journals and literature reviews, taken from databases such as MEDLINE, EMBASE, and PubMed.
Key words: condylar hyperplasia, hemimandibular hyperplasia, hemimandibular elongation, facial asymmetry, scintigraphy.
INTRODUCTION
Condylar Hyperplasia (CH) is a self-limiting pathologic condition that produces severe facial deformity at the expense of mandibular asymmetry. It is characterized by exaggerated and progressive growth of the condyle and can compromise the neck, the ramus, and the body of the mandible; it tends to be unilateral, although bilateral conditions also exist and can be accompanied by pain and articular dysfunction.1 It is commonly found in patients aged 11 to 25 years in its active form, and after this age it may be found in its passive form, usually like a clinical sequel left by the disease.1, 2 However, it can also occur in its active form in patients between the third and fifth decade of life, and even before the age of ten, and it has been reported to be more prevalent in women than in men.3 This condition can appear in three forms: Hemimandibular Hyperplasia (HH) which corresponds to asymmetry by vertical growth, Hemimandibular Elongation (HE), corresponding to asymmetry by horizontal growth, and a hybrid form of these two types.4
Its etiology is due to factors that may be genetic, traumatic, functional, hormonal, and tumor-related.4, 5
Diagnostic impression of CH can be made by a combination of clinical and radiological findings, next corroborated by means of nuclear medicine tests such as scintigraphy, and finally confirmed by pathology report when the patient undergoes surgery.
There are various diagnostic aids ranging from extraoral photographs, static and articulated study models, panoramic radiography, posterior-anterior radiography, tomography with 3D reconstruction, bone scan and SPECT-type scintigraphy, to histopathology studies for the diagnosis of hyperplasia.6
Early diagnosis is important since treatment modalities considerably differ depending on the affected structures, patient's age, severity of the asymmetry, and the active or passive status of the pathology.
It is necessary to treat the disease and to decide whether the center of growth is to be removed in cases in which active CH is detected or, on the contrary, to treat the sequel with orthognathic surgery and/or dentoalveolar orthodontic compensation when the pathology is inactive. This is why proper diagnosis of the pathology is important, and here is where TMJ bone scan should be essential for the clinician to obtain adequate information, ideally through quantitative data.7
DEFINITION
CH is a disorder characterized by excessive and progressive growth that affects the condyle's head and neck, as well as the mandible's body and ramus. The disease is self-limiting and deforming because growth is disproportionate even before the individual's overall growth has stopped, and can continue beyond its completion.4 This disease affects not only the patients' facial esthetics but also their masticatory functions. It is a condition that concerns not only maxillofacial surgeons but also orthodontists seeking to provide patients with normal occlusion, which is directly affected by an underlying pathology, like cell hyperactivity in the condyle.1
CLASSIFICATION
Obwegeser y Makek4 classified the asymmetry associated with CH in 3 categories: Hemimandibular Hyperplasia (HH), or asymmetry by vertical growth, Hemimandibular Elongation (HE), or asymmetry by horizontal growth, and a combination of these two types.
HH is characterized by a three-dimensional widening of one side of the mandible and excessive condyle growth, so that the condyle's neck looks thin and the ramus' height is bigger. It may produce ipsilateral open bite or over-eruption of maxillary teeth as they seek to achieve occlusion; there is very little deviation of the chin, and asymmetry occurs with decrease of the commissure of the affected side. There is compensation in the middle third by enlargement of the alveolar process, as well as downward inclination of the occlusal plane in the affected side, and even inclination in the orbital plane, but tooth midlines usually coincide.4
HE is the most common type of CH; it is characterized by normal size and shape of the condyle's head, but is accompanied by an elongated neck. There is chin deviation to the contralateral side, but there is no vertical increase of the ramus. The mandibular angle shows less alteration than in presence of vertical growth. Intraorally, the midline deviates towards the unaffected side, and occlusion usually shows contralateral cross bite, while the affected side displaces in mesial direction tending to Angle's Class III.4
The lower edge remains significantly unchanged and the compensatory changes of the middle third are mild, although there may be a slight inclination towards the floor of the orbit; it is also possible that both the philtrum of the upper lip and the nasal tip incline towards the unaffected side.
On the other hand, when the elongation is bilateral, it produces severe mandibular prognathism with or without asymmetry.
Type III is the hybrid form. It produces elongation and hyperplasia on the same side. The affected side is more voluminous, with its lower edge located below that of the opposite side. There is chin prominence with displacement towards the unaffected side and evident inclination of the occlusal plane.8
ETIOLOGY
The etiology of this disease is controversial; however, the following factors are the most relevant: genetic factors (congenital malformations, hemifacial microsomia, hemifacial atrophy), environmental factors (prenatal and postnatal trauma, infections, deficiencies in blood supply and hyper-vascularization, as well as neurotrophic disorders), functional factors (habits and occlusal interferences), hormonal factors (endocrine problems and growth factors), and neoplastic factors (osteoma, osteochondroma and chondroma).7, 9, 10
INCIDENCE
CH is usually unilateral and the literature reports a significant predisposition of women compared with men (2:1 ratio), with a prevalence of 57% in the right-side condyle compared to the left-side condyle, with 43%.3 In 2012, Raijmakers et al3 reported that female patients with unilateral CH outnumber male patients in the study populations, then being a female can be considered a risk factor for Unilateral CH (UCH).
Female prevalence has been associated with hormonal differences, especially with estrogens, since most CH patients reported in the literature have been found in the stage of development of secondary sexual characteristics—so it is possible that sex hormones are involved in the abnormal growth of the mandible—.3 The explanation may be that estrogens are one of the main regulators of bone growth and are expressed in articular cartilage and growth plates, since experimental evidence of local synthesis of estrogen has been found in the temporomandibular joint.10, 11
CHARACTERISTICS
It was first described by Robert Adams in 18366 as a condition that causes excessive development of the mandible and generates esthetic and functional alterations. Since then, there have been numerous reports in the literature referring to this clinical entity and the way it compromises facial esthetics and occlusal-functional alterations.
Characteristics of CH include uni- or bilateral enlarged mandibular condyle, so that the condyle's neck is enlarged out, inclining itself and showing downward growth below the mandible's body and ramus, causing enlargement of that side of the face and flattening of the contralateral side. Some patients may experience temporomandibular joint symptoms (TMD), such as pain, articular sounds, and limited mouth opening.12 Therefore, patients seek consultation due to marked facial asymmetry with mandibular deviation, malocclusion, and in some cases articular symptoms, usually noticed between the second and third decades of life.4, 12
It usually occurs in adolescence until the end of pubertal growth. If the deformity occurs before growth is completed, the occlusal plane usually inclines due to dental compensation, while posterior open bite may be evident if the deformity occurs once growth is completed.13
Some biomechanical phenomena may explain why deforming growth occurs in the mandible's body and ramus. Taking into account the mechanisms that maintain compression and tension forces within a range compatible with the tissue's health, in the presence of situations that produce loads exceeding the functional capacity of articular tissues, such as trauma, parafunction, or excessive and fast growth, the force vectors produce a spatial change of the system's structures, generating a sequence of events ranging from remodeling to degeneration and repair, resulting in forces redistribution. These articulatory changes are followed by morphological changes in the ipsilateral ramus and the mandibular body with impacts on facial harmony.4
HISTOPATHOLOGY OF CH
Hyperplasia is known as the increase in number of cells in a tissue, in this case causing excessive development of the condyle. Histologically, the active state of CH is characterized by the presence of a layer of undifferentiated mesenchymal cells and a layer of hypertrophic cartilage, along with islands of chondrocytes in trabecular bone, which is detected by technetium during scintigraphy—and calcification rate appears to be above normal ranges—.12 This cartilage is very thick and is replaced with new bone. This translates into hypermetabolism in the center of condylar growth on the affected side, with conversion of hyaline cartilage into fibrocartilage.2
DAccording to Gray et al in 1990,12 there is another type of hyperplasia during the third and fourth decades of life, characterized by a delayed reaction of growth, in which histologically masses of hyaline cartilage are associated with degenerative areas of the TMJ and painful symptoms.6, 9 The center of growth, however, is located in the center of the condyle instead of the center of the fibrocartilage. When growth stops, the histological appearance is of a normal condyle with an irregular shape.1
Based on histopathology and clinical criteria, CH has been classified into two types: Active CH and Inactive CH (a stable situation in which abnormal growth is completed).14, 15 The active state shows a continuous articular surface and a large area of proliferation in which the hypertrophic cartilage layer shows average thickness. The inactive state is characterized by a discontinuous articular surface and a zone of proliferation in patches; also, the hypertrophic layer presents variable thickness and a large number of hypertrophic chondrocytes in some areasx.16
DIAGNOSIS
Diagnosis of craniofacial asymmetries, one of them being CH, is important because treatment modalities considerably differ depending on the origin of the deformity, i.e., if it has a dental, skeletal, or functional origin. Several methods have been used to identify and quantify the severity of dental and facial asymmetries, including anamnesis, direct clinical evaluation, radiographic analysis, and evaluation of the face's vertical and horizontal proportions by means of facial photographs.7
Many diagnostic aids have been used to complement the clinical and physical examination of this pathology, including extraoral radiographs and photograph analysis, especially front views with a perfect position of the head to prevent alterations in the study of proportions. Study models are also of great help in the assessment of facial asymmetries, as they usually include a dental component.17
RADIOGRAPHIC METHODS FOR CH DIAGNOSIS
Conventional radiographs are used to determine the location of uni- or bilateral discrepancies that contribute to skeletal asymmetry, such as elongation of the mandibular condyle/neck of the involved condyle and the inclination of the mandible's body and ramus,13 and to assess the degree of deviation of dental and skeletal midlines from the mid-sagittal plane. Additionally, nuclear medicine offers planar bone scintigraphy and SPECT (Single-Photon Emission Computed Tomography), which allow a clear identification of active processes of condylar growth between inactive zones.
Lateral cephalic x-rays: it provides useful information about vertical asymmetries, sagittal projection of the asymmetry in ramus height, mandible length, and goniac angle. In addition, individual or serial cephalometric analyses have long been a standard technique for the assessment of growth.5, 18-20 The latter is not very reliable because of the superposition of structures and magnification, due to varying distances between the film and the x-rays; plus it is a 2D technique, so the interpretation of this test is limited..9
In 1999, Kubota reported that the use of cephalometric tracing on lateral radiographs should not be considered a routine test for facial asymmetries, since the size of the condyle will be measured on the right side only and there won't be clarity about the left side.21
Panoramic x-rays: Since the invention of panoramic radiography in 1949 by Paatero, different types of analysis have been developed over the years, such as the ones by Kjellberg et al22 and Levandoski,19 which allow using panoramic radiographs to determine symmetry between planes by comparing both sides of the mandible in the same patient, providing a general view of the temporomandibular joint.21 It is a useful tool to assess dental and bone structures of maxilla and mandible, as it enables a quick identification of asymmetries by comparing size, height and shape of the condyles, as well as the mandible's body and ramus. Its disadvantage lies in the geometric distortion due to projection features of the equipment used to take the images, so the shape of an area may vary from one film to the other.5-9
Posterior-anterior radiography: It is a powerful tool to compare the structures of the right side and left side. This type of radiography is important in cases of asymmetry because by means of Grummons analysis it allows performing a comparative analysis of condylar heights, as well as size of mandibular bodies and rami and the inclination of the occlusal plane, although it is also limited due to superimposition of structures9, 22, 23
Computed Tomography: This technique has recently gained attention in the diagnosis of craniofacial deformities thanks to the advantages offered by the use of software that allows precise measurements, showing the craniofacial bones from different angles by rotating three-dimensional images and observing inside the structures.24 3D tomography is useful to accurately evaluate the morphological and structural alterations of craniofacial bones.25 It allows assessing whether bone growth is generalized or localized in one part of the condyle's head.13 Similarly, it plays an important role in planning surgery, since the predictions based on traditional two-dimensional cephalograms may be very difficult and inaccurate. With diagnosis and planning based on three-dimensional tomography, we can verify the effects of surgical correction in a three-dimensional model.26
NUCLEAR MEDICINE IMAGING
The imaging procedures of nuclear medicine are minimally invasive and, with the exception of intravenous injections to apply radiotracers, they usually are painless medical tests that help physicians diagnose and evaluate health problems. These scans by images use radioactive materials called radiopharmaceuticals or radiotracers.
There are two types of scintigraphic evidence to diagnose CH in order to corroborate the presumptive diagnosis: planar bone scintigraphy and Single-Photon Emission Computed Tomography (SPECT).27-29
Planar bone scintigraphy: (figure 1) This test detects areas of increased or decreased bone metabolism. The test is performed to identify abnormal processes compromising bones, such as growth alterations, tumors, infection, or fractures.7, 9
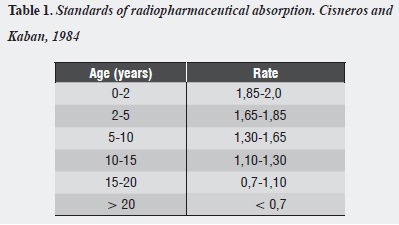
In 1982, Kaban et al30 first used bone scintigraphy in a study of non-symmetrical patients to determine the degree of absorption of the radiopharmaceutical according to age and skeletal maturation. The sample included 34 patients ranging from 15 months to 22 years of age, which were administered Tc-99m MDP in order to determine standards of radiopharmaceutical absorption, finding out that as age increases, absorption decreases in a linear pattern and its rate is close to values below 1 when growth stops. The values found by Cisneros and Kaban31 in 1984 are shown in table 1.
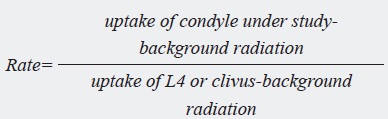
To obtain rate, the following operation was used:
Background radiation is the one the gamma camera detects as coming from the rest of the body, and it should be separated from the one emitted by the tracer's target organs—something that is performed by a computer—. The results are compared with the radionucleotide uptake rate in condyles of normal patients.
Additionally, in this study of symmetrical patients the difference in absorption between the condyles was no greater than 10%; therefore, differences below this percentage of absorption are considered normal. Subsequently, the researchers conducted a study on patients with mandibular asymmetry (Cisneros, 1984), finding out that bone scintigraphy quantifies the bone's uptake of radiopharmaceutical 99mTc-MDP in the condyle, the ramus, and regions of the mandible's body.31
Technetium 99 is a gamma emitter actively captured by bones when intravenously injected along with methylene diphosphonate (MDP); it is metabolized by bone cells and incorporated in areas where new bone is forming or resorbing. It is used to diagnose suspected unilateral or bilateral CH, and its distribution can be measured by gamma rays (gamma camera). The average lifespan of the isotope is six hours and is commercially available. The radiation dose is comparable to that of an x-ray of the skeleton of a child's entire body, or that of a normal skull x-ray series in adults. The uptake of technetium 99 MDP in bone is an indication of recent metabolic activity. For this reason, scintigraphy with this radiopharmaceutical can be used as a good method to evaluate skeletal growth.30, 31
Bone scintigraphy is an instant method of comparison of cellular metabolic activity between normal and abnormal condyles. It can be used to distinguish the normal side from the abnormal and to provide information about hyperplasia stability or activity, since it is often found that hyperplasia shows peaks of exacerbation and greater growth; it also provides information about inactivity, which is only possible to assess by means of scintigraphy.27
Scintigraphy is non-specific, since a positive result can be produced by any kind of increase in bone metabolism, either infectious, inflammatory, traumatic, or neoplastic in nature, and even in normal growth processes.32
Bone scintigraphy has 3 phases. The first is the angiographic phase, performed immediately after injecting the radiopharmaceutical or radiotracer; it detects the level of vascularization of the zone through fast images (2-5 sec/image). The second is the tissue phase, taken approximately 10 minutes later, which analyses adjacent soft tissues. And the third is the bone phase (or late phase), which is taken during the first four hours.5
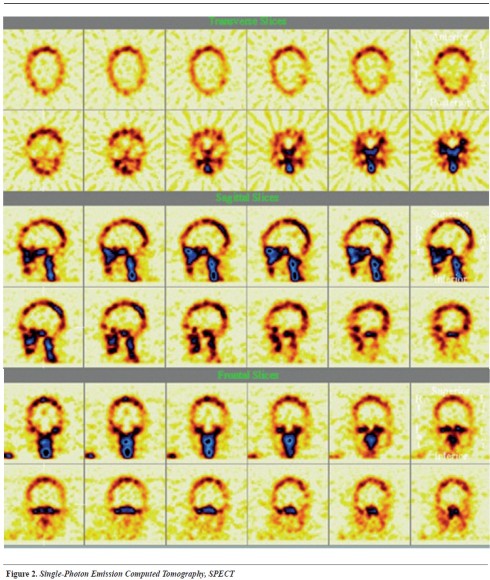
SPECT is a newly developed technique used to collect and display serial images by parallel planes of nuclear medicine (figure 2). It is a variation of scintigraphy and is a method of functional imaging, which reflects the metabolic response of the organ under evaluation through the use of a radiopharmaceutical (technetium 99 MDP), which is brought to an area determined and controlled by the level of metabolic activity and blood flow in the region.28, 33, 34
The procedure involves the use of a gamma camera that rotates around the patient generating circumferential projections. Sections of the axial tomography, of approximately 6.5 mm between one and the other, are computerized in the same way as with an x-ray scanner tomograph.29
SPECT has become an essential diagnostic tool to observe condyle's hyperactivity.6 It provides enhanced image contrast and a quantitative capacity that enables the clinician to make a more accurate assessment of the stage of normal and asymmetric activity of mandibular growth.35 The increase in radionuclide uptake by the hyperplastic condyle may mean that abnormal growth continues.31,36
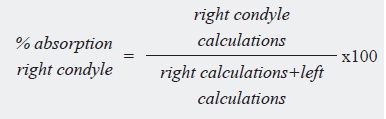
These two techniques (planar scintigraphy and SPECT) can be analyzed in a qualitative (subjective) manner by observing the images delivered by scintigraphy, and in a quantitative (objective) manner by quantifying the condyle's rate of nucleotide absorption.28
In 2011, Saridin et al28 showed that the SPECT technique to detect Unilateral CH is significantly more sensitive than the technique of planar bone scintigraphy, with an additional 19% of the SPECT technique in identifying Unilateral CH.
The use of SPECT technology makes it possible to obtain an image of both condyles and the clivus in the same section. Since it corresponds to the intersection of the occipital bone and the body of the sphenoid, the clivus is located at the cranial base, at the same axial level of mandibular condyles.37
It has been shown that the clivus of the cranial base stops growing when the spheno-basilar synchondrosis fuses. Once this fusion occurs, it may become one of the least metabolically active bones in the body because it has no joints and does not support weight. As they remain stable during growth, this structure and the lumbar vertebra 4 (L4) have been used as points of reference in these diagnostic methods to establish quantitative comparisons of bone cell hyperperfusion between both condyles.29, 38, 39
SPECT images of patients with disease of the cranial base are more sensitive than the planar images and can provide the anatomical location of the pathology and be helpful in patients with negative CT scan.
In 1995, Pogrel et al29 designed a study to compare two methods of quantification of technetium 99-MDP uptake in the mandibular condyle by means of two techniques: a standard planar scintigraphy, having the fourth lumbar vertebra (L4) as a reference, and a SPECT technique, which quantifies the condyle activity compared with absorption in the clivus.
They found out that SPECT provided better reproducibility compared to planar scan, since the activity of the clivus showed a lower variation than that of the fourth lumbar vertebra. They concluded that using SPECT with the clivus as a point of reference solves the problem of superimposition, which usually generated by planar scan, and prevents possible problems associated with the absorption of L4.
Planar bone scintigraphy has proven to be a specific diagnostic test in (85%) and a sensitive test in (67%),29 compared with 93% sensitivity and 96% specificity of the SPECT diagnostic test,40 which could bring us closer to proper diagnosis and therefore provide an ideal timely treatment, preventing severe facial asymmetries in the patient and improving the prognosis of the disease.
The quantitative evaluation of radiopharmaceutical absorption at the condylar level in cases of suspicion of hyperplasia can be done by comparatively detecting the percentage of uptake between the two condyles, and as explained above to identify the rate, uptake of both joints is related to the fourth lumbar vertebra (L4) or the clivus, which, as it is well known, can serve as a reference due to its easy location and symmetrical uptake.36, 40
It has been shown that a 10% difference in absorption between both condyles may indicate asymmetry, and absorption values above 55% are an indication of HC.31, 32
DIFFERENTIAL DIAGNOSIS OF CH
Unilateral CH should be distinguished from other processes that cause facial asymmetry, such as hemifacial microsomia, hemifacial atrophy, ankylosis and bone tumors, unilateral macrognatism (mandibular unilateral hypertrophy, or the enlargement of the mandible in three dimensions, including condyle, ramus and midline of the symphysis), and laterognatia (asymmetric prognathism in which both condyles are of equal size).13, 41
Clinically, hemifacial microsomia resembles the pattern of horizontal growth of CH, although it is due to condylar hypoplasia in the opposite side and obviously it is not accompanied by hyperactivity in the condylar region. They can also be distinguished by the numerous facial and ear features produced by microsomia.42, 43
The differential diagnosis also includes neoplastic conditions, such as osteochondroma, osteoma, osteblastoma and chondrosarcoma, which may show clinical, radiographic, and occlusal characteristics similar to those of CH.
It differs from osteochondroma because in this disease enlargement is limited to the tumor. The dimensions of both mandible halves are equal, the tumor has flattened margins, cartilage covering is not observed in the x-ray, it can be seen as a separate initial bone growth, and growth is not selflimiting. Also, it can occur in a non-available space and create mandibular asymmetry and changes in occlusion.4
For an immediate response upon suspicion, techniques such as scintigraphy or its SPECT variation can be used.44
TREATMENT OF CH
Surgical treatment varies according to the level of activity of the disease. Surgery should be based on the findings of technetium 99 MDP uptake, which is used to monitor the activity of condyle growth, since the radiolucency is concentrated in areas of increased osteoblastic activity.14
Treatment of mandibular deformity is mainly surgical; it consists of intervention based on the activity of the condyle: high condylectomy or trimming of the condyle on the affected side is intended to limit the progression of the asymmetry during the active phase of condylar overgrowth. It consists of removing the top of the condyle with a dissection of 3-5 mm of the condylar head, including the medial and lateral poles. This must be preceded by a deep dissection of the fascia layer and the condyle must be gently divided from the joint disk. The osteotomy line is usually caudal to the edge of the condyle head, and is performed with a 2 mm deep fissure but. Once the section has been made, reintegration of the pterygoid external muscle must be achieved by suturing the tendon to the new condylar head. When condylectomy is performed along with bi- or mono-maxillary orthognathic surgery, it should be done in the following order: maxillary osteotomy, condylectomy, and mandibular osteotomy. Finally, the clinician must make sure that the condyle reaches the fossa9 and to suture the capsule, the fascia and the ligaments.45-47
Condylectomy must be performed once CH has been diagnosed, followed by orthodontic treatment either by dentoalveolar decompensation, in order to prepare the patient for orthognathic surgery to correct sequels of the disease (asymmetry), or by compensatory orthodontic treatment in cases where the disease has been detected in time and what needs to be corrected is an occlusal compromise instead of an esthetic condition by skeletal alteration. The basic considerations in the management of secondary facial asymmetry or CH should include control of the growth process to allow for balanced facial development as well as control of the occlusal plane and correction of the dentoalveolar compensations that occur during the active phase of the disease.14, 16 In cases where the diagnosis includes suspicion of the presence of tumor, this procedure is compulsory.13, 14, 39, 44
Pre-surgical orthodontic treatment of hyperplasia in its inactive state is used to align and level the dental arches in order to eliminate the dental compensation produced in the three spatial planes and to correct inclinations, torque and axial shaft of the entire dentition, while post-surgical orthodontics provides patients with and ideal occlusion which is at the same time functional and esthetically harmonious with the new post-surgery patient condition.48
In 2002, Wolford et al45 compared the results of CH treatment in a long term follow-up of postoperative stability in patients diagnosed with this disease. One group was treated with orthognathic surgery only to correct asymmetry, while the other group was treated with high condylectomy, articular disc repositioning and simultaneous orthognathic surgery, proving that the latter is more stable and reliable over time, with a statistically significant difference.
LHigh condylectomy stops excessive and disproportionate mandibular growth by surgical removal of the main sites of mandibular growth49, 50
CONCLUSIONS
The literature shows that CH can occur at any age, but there is predisposition during the stage of growth and development; also, it is prevalent among females and the unilateral form is more common than the bilateral.
Of the three forms of manifestation of CH, Hemimandibular Elongation is the most common, characterized by deviation of the mandible body and adjacent tissues towards the unaffected side.
Early diagnosis of CH allows for the establishment of treatment plans that stop the pathology in its active phase and guide the remnants of patients' growth, reducing the sequels left by the disease when diagnosed after the stage of development.
It is important to present the scintigraphy results in a quantitative manner in order to know the percentage of absorption of each condyle and thus establish the difference between the two. Taking into account that absorption values over 55% are indicative of hyperplasia and a 10% difference between both condyles suggest asymmetry.
It is necessary to perform studies that establish the behavior of the pathology in our population, comparing different scintigraphic scans and, in turn, these results should be correlated with pathology reports in order to exactly establish the specificity of scintigraphic tests.
REFERENCES
1. Nitzan DW, Katsnelson A, Bermanis I, Brin I, Casap N. The clinical characteristics of condylar hyperplasia: experience with 61 patients. J Oral Maxillofac Surg 2008; 66(2): 312-318. [ Links ]
2. Eslami B, Behnia H, Javadi H, Khiabani KS, Saffar AS. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96(6): 711-717. [ Links ]
3. Raijmakers PG, Karssemakers LH, Tuinzing DB. Female predominance and effect of gender on unilateral condylar hyperplasia: a review and meta-analysis. J Oral Maxillofac Surg 2012; 70(1): e72-76. [ Links ]
4. Obwegeser HL, Makek MS. Hemimandibular hyperplasia-hemimandibular elongation. J Oral Maxillofac Surg 1986;14(4): 183-208. [ Links ]
5. Anaya JA. Manejo interdisciplinario de la hiperplasia condilar. Revista Ortousta 2002; 2: 7-20. [ Links ]
6. Villanueva-Alcojol L, Monje F, González-García R. Hyperplasia of the mandibular condyle: clinical, histopathologic, and treatment considerations in a series of 36 patients. J Oral Maxillofac Surg 2011; 69(2): 447-455. [ Links ]
7. Sora C, Jaramillo P. Diagnóstico de las asimetrías faciales y dentales. Rev Fac Odontol Univ Antioq 2005; 16(1 y 2): 15-25. [ Links ]
8. Mishra S, Mishra YC. Hemimandibular elongation: a case report with a 7-year follow up. J Oral Maxillofac Surg 2013; 25(4): 347-350. [ Links ]
9. Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod 1994; 64(2): 89-98. [ Links ]
10. Talwar RM, Wong BS, Svoboda K, Harper RP. Effects of estrogen on chondrocyte proliferation and collagen synthesis in skeletally mature articular cartilage. J Oral Maxillofac Surg 2006; 64(4): 600-609. [ Links ]
11. Yu S, Xing X, Liang S, Ma Z, Li F, Wang M et al. Locally synthesized estrogen plays an important role in the development of TMD. Med Hypotheses 2009;72(6): 720-722. [ Links ]
12. Gray RJ, Sloan P, Quayle AA, Carter DH. Histopathological and scintigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg 1990;19(2): 65-71. [ Links ]
13. Mehrotra D, Dhasmana S, Kamboj M, Gambhir G. Condylar hyperplasia and facial asymmetry: report of five cases. J Oral Maxillofac Surg 2011; 10(1): 50-56. [ Links ]
14. Munoz MF, Monje F, Goizueta C, Rodriguez-Campo F. Active condylar hyperplasia treated by high condylectomy: report of case. J Oral Maxillofac Surg 1999; 57(12): 1455- 1459. [ Links ]
15. Luz JG, de Rezende JR, de Araújo VC, Chilvarquer I. Active unilateral condylar hyperplasia. Cranio 1994; 12(1): 58-62. [ Links ]
16. Angiero F, Farronato G, Benedicenti S, Vinci R, Farronato D, Magistro S et al. Mandibular condylar hyperplasia: clinical, histopathological, and treatment considerations. Cranio 2009; 27(1): 24-32. [ Links ]
17. Pripatnanont P, Vittayakittipong P, Markmanee U, Thongmak S, Yipintsoi T. The use of SPECT to evaluate growth cessation of the mandible in unilateral condylar hyperplasia. Int J Oral Maxillofac Surg 2005; 34(4): 364-368. [ Links ]
18. Murray RR. Cephalometric analysis and synthesis. Angle Orthod 1961; 31: 141-156. [ Links ]
19. Levandoski RR. Mandibular whiplash. Part I: an extension flexion injury of the temporomandibular joints. Funct Orthod 1993; 10(1): 26-29, 32-33. [ Links ]
20. Epker BFL. Dentofacial deformities. Integrated orthodontic and surgical correction. St. Louis: Mosby; 1986. [ Links ]
21. Kubota Y, Takenoshita Y, Takamori K, Kanamoto M, Shirasuna K. Levandoski Panographic analysis in the diagnosis of hyperplasia of the coronoid process. Br J Oral Maxillofac Surg 1999;37(5): 409-411. [ Links ]
22. Kjellberg H, Ekestubbe A, Kiliaridis S, Thilander B. Condylar height on panoramic radiographs. A methodologic study with a clinical application. Acta Odontol Scand 1994; 52(1): 43-50. [ Links ]
23. Grummons DC, Kappeyne van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod 1987; 21(7): 448-465. [ Links ]
24. Letzer GM, Kronman JH. A posteroanterior cephalometric evaluation of craniofacial asymmetry. Angle Orthod 1967; 37(3): 205-211. [ Links ]
25. Olszewski R, Zech F, Cosnard G, Nicolas V, Macq B, Reychler H. Three-dimensional computed tomography cephalometric craniofacial analysis: experimental validation in vitro. Int J Adult Orthodon Orthognath Surg 2007; 36(9): 828-833. [ Links ]
26. De Moraes ME, Hollender LG, Chen CS, Moraes LC, Balducci I. Evaluating craniofacial asymmetry with digital cephalometric images and cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2011;139(6): e523-531. [ Links ]
27. Pelo S, Correra P, Gasparini G, Marianetti TM, Cervelli D, Grippaudo C et al. Three-dimensional analysis and treatment planning of hemimandibular hyperplasia. J Craniofac Surg 2011; 22(6): 2227-2234. [ Links ]
28. Saridin CP, Raijmakers PG, Tuinzing DB, Becking AG. Bone scintigraphy as a diagnostic method in unilateral hyperactivity of the mandibular condyles: a review and meta-analysis of the literature. Int J Oral Maxillofac Surg 2011; 40(1): 11-17. [ Links ]
29. Pogrel MA, Kopf J, Dodson TB, Hattner R, Kaban LB. A comparison of single-photon emission computed tomography and planar imaging for quantitative skeletal scintigraphy of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 80(2): 226-231. [ Links ]
30. Kaban LB, Cisneros GJ, Heyman S, Treves S. Assessment of mandibular growth by skeletal scintigraphy. J Oral Maxillofac Surg 1982; 40(1): 18-22. [ Links ]
31. Cisneros GJ, Kaban LB. Computerized skeletal scintigraphy for assessment of mandibular asymmetry. J Oral Maxillofac Surg 1984; 42(8): 513-520. [ Links ]
32. Saridin CP, Raijmakers P, Becking AG. Quantitative analysis of planar bone scintigraphy in patients with unilateral condylar hyperplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104(2): 259-263. [ Links ]
33. Slootweg PJ, Muller H. Condylar hyperplasia. A clinicopathological analysis of 22 cases. J Maxillofac Surg 1986;14(4): 209-214. [ Links ]
34. Motamedi MH. Treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg 1996; 54(10): 1161-1169. [ Links ]
35. Fahey FH, Abramson ZR, Padwa BL, Zimmerman RE, Zurakowski D, Nissenbaum M et al. Use of (99m)Tc-MDP SPECT for assessment of mandibular growth: development of normal values. Eur J Nucl Med Mol Imaging 2010; 37(5):1002-1010. [ Links ]
36. Hodder SC, Rees JI, Oliver TB, Facey PE, Sugar AW. SPECT bone scintigraphy in the diagnosis and management of mandibular condylar hyperplasia. Br J Oral Maxillofac Surg 2000; 38(2): 87-93. [ Links ]
37. Melsen B. The cranial base. Acta Odontol Scand 1974; 32(62): 86-101. [ Links ]
38. Israel O, Jerushalmi J, Frenkel A, Kuten A, Front D. Normal and abnormal single photon emission computed tomography of the skull: comparison with planar scintigraphy. J Nucl Med 1988; 29(8): 1341-1346. [ Links ]
39. Kircos LT, Carey JE, Keyes JW Jr. Quantitative organ visualization using SPECT. J Nucl Med 1987; 28(3): 334- 341. [ Links ]
40. Saridin CP, Raijmakers PG, Tuinzing DB, Becking AG. Comparison of planar bone scintigraphy and single photon emission computed tomography in patients suspected of having unilateral condylar hyperactivity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(3): 462-432. [ Links ]
41. Khorsandian G, Lapointe HJ, Armstrong JE, Wysocki GP. Idiopathic noncondylar hemimandibular hyperplasia. Int J Paediatr Dent. 2001; 11(4): 298-303. [ Links ]
42. Kaban LB. Cirugía oral y maxilofacial en niños. México D.F.: Interamericana; 1992. [ Links ]
43. Pirttiniemi P, Peltomäki T, Müller L, Luder HU. Abnormal mandibular growth and the condylar cartilage. Eur J Orthod 2009; 31(1): 1-11. [ Links ]
44. Venturin JS, Shintaku WH, Shigeta Y, Ogawa T, Le B, Clark GT. Temporomandibular joint condylar abnormality: evaluation, treatment planning, and surgical approach. J Oral Maxillofac Surg 2010; 68(5): 1189-1196. [ Links ]
45. Wolford LM, Mehra P, Reiche-Fischel O, Morales-Ryan CA, García-Morales P. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop 2002; 121(2): 136-150. [ Links ]
46. Brusati R, Pedrazzoli M, Colletti G. Functional results after condylectomy in active laterognathia. Cranio 2010; 38(3): 179-184. [ Links ]
47. Lippold C, Kruse-Losler B, Danesh G, Joos U, Meyer U. Treatment of hemimandibular hyperplasia: the biological basis of condylectomy. Br J Oral Maxillofac Surg 2007; 45(5): 353-360. [ Links ]
48. Crank S, Gray S, Sidebottom AJ. Condylar hyperplasia- Review of treatment outcomes and suggested pathway for management. Br J Oral Maxillofac Surg 2007; 45(7): e60-61. [ Links ]
49. Bertolini F, Bianchi B, De Riu G, Di Blasio A, Sesenna E. Hemimandibular hyperplasia treated by early high condylectomy: a case report. Int J Adult Orthodon Orthognath Surg 2001; 16(3): 227-224. [ Links ]
50. Ferreira S, Da Silva-Fabris AL, Ferreira GR. Unilateral condylar hyperplasia: a treatment strategy. J Craniofac Surg 2014; 25(3): e256-258. [ Links ]











 text in
text in