INTRODUCTION
Endodontically treated teeth that have suffered coronal structure loss need to be rehabilitated with a post and a stump. The post is cemented in the prepared root canal with an apical seal of 4 to 5 mm. For a treatment with prefabricated posts to be effective, it is important to take into account the type of cement and the cementing technique to be used. The mechanical properties depend on the behavior of the whole; a cement with an elastic modulus lower than the rest of the components is therefore ideal.1
There are two types of posts: prefabricated posts and cast posts, which has long been considered the most reliable method to reconstruct tooth structure. Prefabricated posts are recommended because they provide quick treatment, easy handling, and are economical and minimally invasive, unlike cast posts.2) Their advantages include simplicity of technique and manufacturing of the stump in a single session.
Since the commercial introduction of fiberreinforced posts, studies have shown the clinical success of systems including an adhesive, a resin cement, and a post, due to their good retention values and their behavior under mechanical stress, as fiber-reinforced posts have a modulus of elasticity of 18 to 22 Gpa, which is similar to that of dentin (18 Gpa), allowing the production of a stress field similar to that of natural tooth, thus reducing the risk of root fractures.3
Different types of cementing agents and their corresponding adhesive systems have been proposed for cementing prefabricated fiberglass posts to root canal dentin. These materials can be divided into three classes: adhesives, self-etching, and adhesives with an acid etching system. Adhesion to root canal dentin may be affected by the operator′s lack of direct vision when implementing cementation protocols, and because of the difficulty in humidity control. It has been shown that humidity control after the application and removal of orthophosphoric acid, as well as the incomplete penetration of resin in dentin, significantly affect bond strength.4
The influence of dentin humidity on adhesion has been demonstrated in total-etch adhesives. Selfetching adhesives (of a single dose) were introduced to overcome the issue of sensitivity of the waterbased technique during penetration of adhesive in etched dentin. The main difference between self-etching adhesives and total-etch adhesives is acidity, because the phosphoric acid used in the total-etch system is chemically more aggressive compared to that of the self-etching system.5)(6
The literature reports several studies on the use of posts and cements and their different presentations and polymerizations, evaluating resistance to pushout. The reports by Bitter et al in 2006 indicate that demineralization of radicular dentin with 37% phosphoric acid or the use of self-etching adhesive systems do not show a significant influence on dentin bond strength; these authors used FRC Postec®posts and six cementing agents, one of them being RelyX Unicem®. In addition, they observed that thickness of the hybrid layer has no influence on the adhesive ability of self-adhesive self-etching systems.4
In 2008, Wang et al assessed bond strength in the presence of push-out forces in fiber posts strengthened and cemented with two adhesive systems, including RelyX Unicem®, and applying the test on four root sites. Their findings showed that the Aestheti-Plus Bisco®quartz fiber posts cemented with acid-etching and an adhesive system had significantly increased retention of the post than carbon fiber posts cemented with a selfadhesive self-etching system. The coronal area of root canal was more retentive than the apical area.7
All this suggests that the emergence of new systems of self-etching cements and adhesives has reduced the number of clinical steps in restorative procedures with prefabricated posts in endodontically treated teeth. It all seeks greater speed and efficiency at the time of cementing prefabricated posts.8
Finally, the material replacing lost dentin must guarantee appropriate clinical performance; therefore, the material (prefabricated post, cement, or rehabilitator) should closely integrate to dentin, forming a single unit.9
The purpose of this article is to present the results of two cementation protocols in fiberglass posts, in order to identify which shows the best adhesive strength in the presence of the push-out test.
MATERIALS AND METHODS
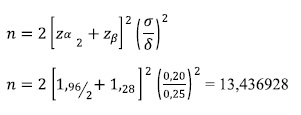
This is an observational, pseudo-experimental, cross-sectional in vitro study seeking to determine the adhesive strength of interfaces in prefabricated fiberglass posts cemented with a luting agent in human premolars subjected to aging effects by storing them at a constant temperature (27 0C) for 30 days in a HigroTerm machine. The size of samples in each group was found with the following formula:
The coefficient of variation was set at 20%, indicating a slight variation, and the global average was set at 25%.
These results showed that each group must have 14 samples; it was finally decided to include 15 samples in each subgroup.
The obtained data were entered in an Excel® spreadsheet and processed in version 15 of the SPSS® software. The averages of adhesive strength and deformation were compared among groups by means of ANOVA test or its respective nonparametric test (Kolmogorov-Smirnov), upon verification of the conditions of normality. P < 0.05 was considered statistically significant.
The design of this study meets the Declaration of Helsinki10 standards for research in humans; similarly, it complies with the provisions in Resolution 008430 of Colombia′s Ministry of Social Protection.11
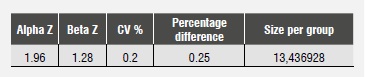
The sample included 60 single-root human premolars extracted for orthodontic reasons, aged 18 to 30 years (prior approval of the Committee for Institutional Review and Human Ethics of Universidad del Valle School of Health) and meeting the inclusion criteria. The samples were randomly sorted out into two groups before root canal treatment; each group was subdivided into two subgroups of 15 teeth and each tooth was cut in four parts, getting three radicular discs of the cervical, middle, and apical areas, which were later analyzed (Table 1).
The crown of each tooth was cut two millimeters above the cemento-enamel junction using a diamond disc (Isocut Wafering Blade-CBN HC, of 7 inches in diameter and 0.03 inches thick), under cooling with abundant water. The roots were endodontically prepared, instrumenting at a working length of 1 mm from the radiographic apex with an apical standardized file #35. All the conducts were instrumented by the same operator using the technique of Step Back® (stainless-steel K-files®) and burs of Gates Glidden drills® (size 2-4 Union Broach®). Irrigation was performed with 5.25% sodium hypochlorite after changing each file, rinsing with distilled water, wiping with paper tips (Dentsply-Maillefer®) and filling with guttapercha cones (Dentsply-Maillefer®) plus Top Seal® Dentsply® epoxy resin-based root canal sealer for Group 1 and Grossman® cement for Group 2, using a lateral condensation technique. Then the cervical portion was temporarily sealed with a cotton wad and coltosol (Coltene®), and the teeth were stored in 100% humidity in dark containers for 8 days to room temperature.
Group 1: 30 teeth received endodontic treatment and filling with Top Seal® Dentsply® epoxy resinbased root canal sealer by an endodontics expert.
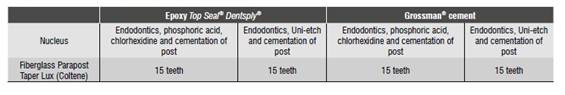
Subgroup 1.1: 15 teeth were applied Condac FGM® 37% phosphoric acid in gel, rinsing and wiping with paper cones, Consepsis Ultradent® 2% chlorhexidine gluconate, wiping with paper cones and cementing the post with Parapost Taper Lux Coltene®, following instructions of the manufacturer of Duo-link universal TM BISCO® cement (Table 2).
Subgroup 1.2: 15 teeth were applied Unietch BISCO® 32% acid in gel, rinsing and wiping with paper cones, and cementing the post with Parapost Taper Lux Coltene®, following instructions of the manufacturer of Duo-link universal TM BISCO® cement (Table 2).
Group 2: 30 teeth received endodontic treatment and filling with Grossman® cement by an endodontics expert.
Subgroup 2.1: 15 teeth were applied Condac FGM® 37% phosphoric acid in gel, rinsing and wiping with paper cones, Consepsis Ultradent® 2% chlorhexidine gluconate, wiping with paper cones and cementing the post with Parapost Taper Lux Coltene®, following instructions of the manufacturer of Duo-link universal TM BISCO® cement (Table 2).
Subgroup 2.2: 15 teeth were applied Unietch BISCO® 32% acid in gel, rinsing and wiping with paper cones, and cementing the post with Parapost Taper Lux Coltene®, following instructions of the manufacturer of Duo-link universal TM BISCO® cement (Table 2).
Once the endodontic treatments were completed, the root canals were unfilled at a depth of 9 mm with respect to the cemento-enamel junction, leaving at least an apical seal of 4 to 5 mm of gutta-percha into the canal. The canals were widened with the right system for the type of nucleus to use, and then they were rinsed with sterile water and wiped with paper tips (Dentsply-Maillefer®).
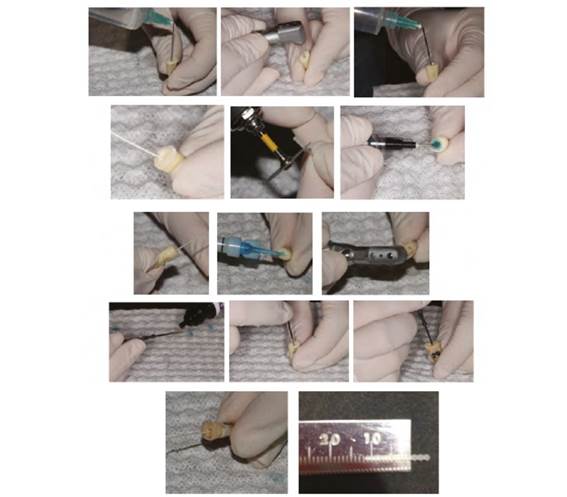
The teeth were sorted out into two groups and the cementation protocol for each subgroup was carried out as previously described (Figure 1).
The samples were subjected to aging by storing them at a constant temperature (27 0C) for 30 days in a HigroTerm machine, a procedure consisting on immersing the samples in distilled water to assess the behavior of resin materials, since the presence of water is crucial to its deterioration and its effect is noticeable when used in adhesive systems. The cuts were performed with an Isomet® 1000 Precision (Buehler) machine and a diamond disc (Isocut Wafering Blade-CBN HC, of 7 inches in diameter and 0.03 inches thick) under cooling, in order to produce four cuts of a post/dentin thickness of two millimeters (cervical, middle, and apical), thus producing three radicular discs per sample.
In order to determine bonding strength between cement and root dentin, the so-called push-out test was conducted using the universal machine (Instron, Model: ELS-5 made in China, with 1 to 600 Kn load capacity), and assessing adhesive strength between the interfaces of materials and teeth. For this test, each sample was attached to the base of the universal machine with a cyanoacrylate adhesive, ensuring that the sample′s coronal surface was located against the universal machine, and the post was placed in the center of the hole in the base. The discs of dental samples were loaded with a cylindrical plunger of a 1 mm in diameter located in the center of the disc, avoiding contact with the surface of surrounding dentine. Loads were applied in an apical-cervical direction with respect to the evaluated tests, at a speed of 0.5 mm/min, until posts were pushed out (Figure 2).
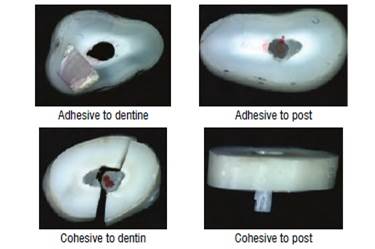
Samples were photographed with an AxioCam ERc5s®Zeiss digital camera of the Stemi 2000-CG®stereomicroscope in order to conduct an observational analysis of the results according to failure type.
RESULTS
In this study, a significance level in α (alfa) 0.05 (5%) was taken as a decision criterion; there was no percentage of reliability because no intervals of confidence were used, statistical hypothesis testing was used instead.
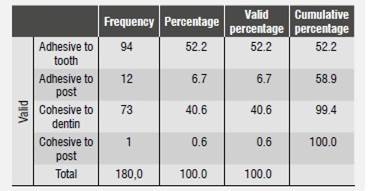
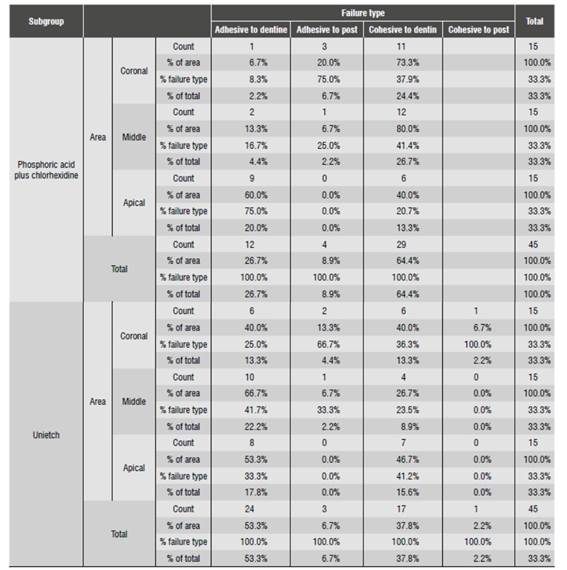
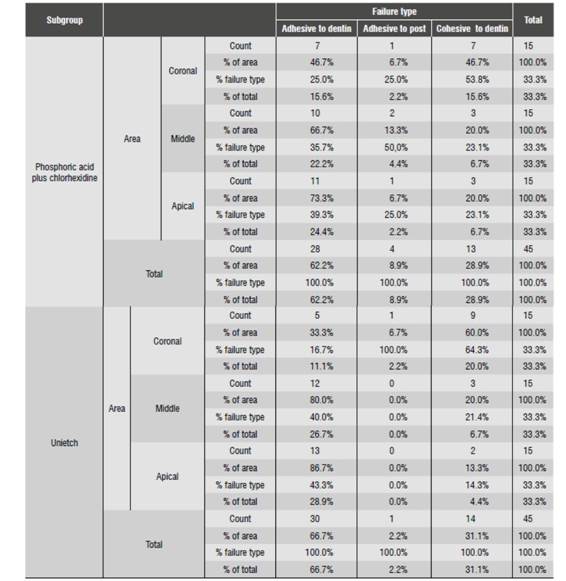
The types of failure found in the study were: adhesive to dentine (AD), adhesive to post (AP), cohesive to dentine (CD), and cohesive to post (CP). The failure percentages are described in Table 3 and in Figure 3.
The means and standard deviations of Group 1 adhesive strength (push out) comparing subgroups 1.1 and 1.2, as well the coronal (C), middle (M), and apical (A) areas, are shown in Table 4.
Table 4 Group 1 descriptors comparing subgroups and areas
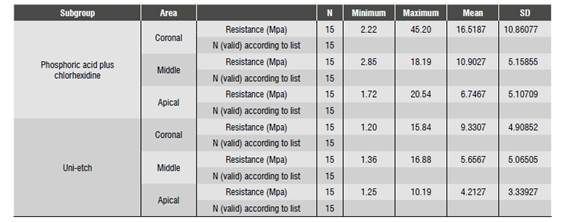
* MPa: Megapascal * N: Newton * SD: Standard deviation
The means and standard deviations of Group 2 adhesive strength (push out) comparing subgroups 2.1 and 2.2, as well the coronal (C), middle (M), and apical (A) areas, are shown in Table 5.
Table 5 Group 2 descriptors comparing subgroups and areas
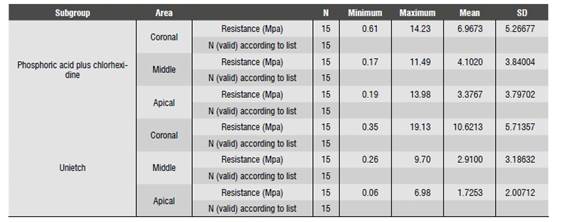
* MPa: Megapascal * N: Newton * SD: Standard deviation
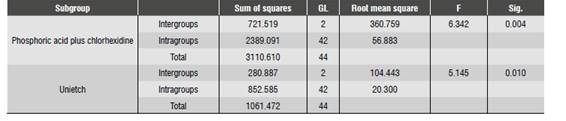
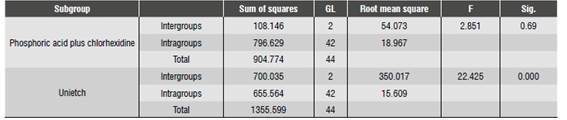
The Kolmogorov-Smirnov test confirmed that there was normality in Group 1, subgroup 1.1 and in Group 2, subgroups 2.1 and 2.2 (p = 0.383, p = 0.086, p = 0.099, respectively), and nonnormality in Group 1, subgroup 1.2 (p = 0,048). The Anova test showed significant difference in adhesive strength in Group 1, subgroups 1.1 and 1.2, and in Group 2, subgroup 2.2 (p < 0.05) and no significant difference in Group 2, subgroup 2.1 (p > 0.05) (Table 6 and Table 7).
In Group 1, subgroup 1.1, the most frequent failure in the coronal area was CD (73.3%), in the middle are it was CD (80%) and in the apical area AD (60%). In subgroup 1.2, the coronal area showed an equal percentage in CD and AD (40%), in the middle area the most common failure was AD (66.7%) and in the apical zone AD (53.3%) (Table 8).
In Group 2, subgroup 2.1, the most frequent failure types in the coronal area was CD (46.7%) and AD (46.7%); in the middle area it was AD (66.7%), and in the apical area AD (73.3%). In subgroup 2.2, the most common failure in the coronal area was CD (60%), in the middle it was AD (80%), and in the apical area AD (86.7%) (Table 9).
DISCUSSION
This study evaluated the adhesive strength of fiberglass posts cemented in single-root human premolars extracted for orthodontic reasons, using different cementing protocols and two different filling materials, and analyzing three specific root areas (coronal, middle, and apical). The first protocol was phosphoric acid plus chlorhexidine (subgroups 1.1 and 2.1) and the second protocol used Unietch (subgroup 1.2 and 2.2), which is a phosphoric acid containing benzalkonium chloride, an antimicrobial agent that according to scientific evidence has the same function as chlorhexidine.12) Once posts had been cemented, the samples were subjected to aging by storing them at constant temperature (27 °C) for 30 days. This method was used in order to assess the clinical performance of materials over time, simulating the degradation of restorations.13)(14)(15) Another commonly used method is aging by thermocycling, which simulates thermal changes in the oral cavity. Recently, in the 2014 Charlotte Convention, Kwon, Burgess and Beck pointed out as one of their conclusions that 10,000 cycles do not show significant difference with the storage method for 24 hours.15) The literature recommends standardizing the protocols in terms of time to determine the number of cycles. However, one hypothesis states that there could be 20 to 50 cycles per day, and therefore there would be about 10,000 cycles per year.
In order to evaluate adhesive strength, the pushout test was used as it provides data on the smallest adhesive areas, uniform distribution of adhesive interface stress, fewer sample loss during experiments, low standard deviation values, and is easy to perform.16)(17
The initial assumption was that there would be no significant differences between the protocols used, but variations were found in terms of adhesive strength depending on the material used to fill the root canals, the cementing protocol, and the tooth area under evaluation.
Once the physical tests were completed, the results yielded data suggesting that the maximum adhesive strength happened in the coronal area of teeth filled with the Top Seal cement (Group 1) where the posts were cemented with phosphoric acid, chlorhexidine, and dual resinous cement (Duolink) (subgroup 1.1), with a score of 45.2 Mpa. In the case of teeth treated with Unietch (subgroups 1.2 and 2.2), the maximum values were 19.13 MPa in those treated with the Grossman filling cement (Group 2) and 15.84 Mpa in those treated with the Top Seal cement (Group 1). While the scores of the Unietch protocol were lower than those of the group treated with phosphoric acid plus chlorhexidine (subgroup 1.1), these scores are still higher than those obtained in 2013by Pereira et al, who found peak scores of 11.5 Mpa for Duolink.17) These authors used a different cementing protocol, since they did not use versa brush together plus hypochlorite, which provides chemical and mechanical cleaning. The versa brush is a rotary instrument used along with low-speed piece to optimize the cleaning of the root canal and to remove the contaminants left by unfilling the root canal (components of the sealing cement and the smear layer). In addition, they did not use chlorhexidine after applying phosphoric acid, and did not take into account the filling cement, which in the present study showed relevance in assessing adhesive strength.
In 2013, Saraiva et al analyzed the effect of etching with phosphoric acid and pretreating dentin with sodium hypochlorite on adhesive strength by means of the push-out between post and canal dentin, using a dual resinous cement (Variolink IIIvoclar/ Vivadent). They found out that pretreating with sodium hypochlorite did not show statistically significant differences in the evaluated groups; however, when phosphoric acid was applied for 60 s in the apical portion without sodium hypochlorite (as pretreatment), the adhesive forces were higher. The present study also used a dual resinous cement (Duolink-Bisco), sodium hypochlorite was used as pretreatment in both groups, and demineralizing acid was used for 15 seconds.
When Saraiva et al analyzed their samples using phosphoric acid for 15 seconds, they found out maximum adhesive strength scores of 9.6 Mpa on apical by pretreating with hypochlorite, while the present study observed a maximum score of 20.54 Mpa in the apical zone using the same protocol; the use of versa brush explain the difference in results.18
In 2013, Shiratori et al evaluated the adhesive strength of three self-adhesive cements using different methods to bring the cement to the interior of the root canal. They found maximum resistance values of 13.65 Mpa in the group that used lentulo to insert the material into the canal, concluding that the technique used to carry the cement seems to influence adhesive strength when cementing intraradicular posts; the protocol in another group used intracanal tips to apply the cement. In the apical area, which is the hardest to reach due to a reduction in canal diameter, they observed a maximum adhesive strength of 20.54 Mpa, being higher than that obtained in self-adhesive cements in general, so the use of intracanal tips possibly influenced the higher adhesive strength values in critical areas such as the apical.19
An important factor in the protocols of the present study was the use of chlorhexidine, which is currently used in dental adhesion as a protease inhibitor. The literature reports that demineralized dentin contains matrix metalloproteinases (MMP) and cathepsins, which can slowly degrade collagen fibers.12) MMP are a type of calcium and zincdependent endopeptidases, capable of degrading all components of the extracellular matrix. Collagenolytic and gelatinolytic activity can be controlled by protease inhibitors, indicating that MMP inhibition may preserve integrity of the hybrid layer. In fact, applying chlorhexidine in vivo improves integrity of the hybrid layer. When phosphoric acid is applied without no subsequent application of chlorhexidine, this does not inhibit the collagenolytic activity mineralized of mineralized dentin, while using chlorhexidine after acid etching, even in very low concentrations, strongly inhibits this activity. The results of the present study generally showed higher adhesive strength scores in protocols with chlorhexidine, compared with those that only used Unietch (benzalkonium chloride) in the three thirds of groups 1 and 2 (Top Seal and Grossman respectively), which is consistent with literature reports about the prevention of degradation of the hybrid layer, thus improving the adhesion to dentin.12
There are various studies on adhesive strength in fiberglass posts cemented with conventional glass ionomers and modified with resin (cementitious). In 2014, Pereira et al found values ranging from 0.5 Mpa to 19.6 Mpa, observing that area were the post is located (cervical, middle, or coronal) does not influence adhesive strength of posts to root dentin. The present study yielded values ranging from 0.6 Mpa to 45.20 Mpa, but unlike the study by Pereira et al, there were differences between the assessed areas. This shows that resin cements need a reliable bonding interface-something that is hart to achieve, especially in the apical area, where hardly there is room for the post-. The absence of hybrid layer at the adhesive interface may contribute to these differences when fiber posts are cemented with resin cements.19)(20)(21
The findings of the present study showed that the lowest adhesive strength levels are at the apical third. This may be due to the residues of guttapercha and endodontic sealer material that may remain in the apical area after preparation, as reported by Bolhuis et al.22
In 2002, Hagge et al evaluated the effect of three cements to seal the root canal on the retention of fiberglass posts cemented with resin cements. The authors used epoxy resinbased cements, eugenol, and calcium hydroxide, finding out that the chemical formulation of sealing cements did not significantly affect the posts retention values. Our study assessed epoxy resin-based cements (Top Seal) and zinc oxidebased cements (Grossman), finding out the lowest values in the group treated with Grossman cement, but these were not statistically significant, agreeing with the findings by Hagge et al.23
One of the limitations of our study is that it is an in vitro research imitating oral conditions. Cement type and the different protocols for cementation of fiberglass posts require clinical studies in greater periods of time in order to evaluate their behavior and to have more reliable results.
CONCLUSIONS
There were no statistically significant differences in using the Top Seal and Grossman sealing cements; however, the group with the lowest adhesive strength scores was that using a zinc oxide-based cement (Grossman) and in the apical areas of the groups -although they remained higher than those found in other related studies-.
Using chlorhexidine as part of the cementation protocol cementing showed higher strength scores compared to the group where it was not used; these results were statistically significant only in the group using the Top Seal cement (epoxy resin) as a sealer.
By comparing the samples using phosphoric acid and chlorhexidine versus Unietch, the lower values were found when using only Unietch only.











 text in
text in