INTRODUCTION
Using fluorides is one of the most common strategies for the prevention of tooth decay, and their incorporation in toothpastes has allowed great improvements in coverage, as well as reduction of dental caries, with figures 30 to 70% greater than those achieved with non-fluoride options,(1,2,3,4,5,6) so that higher concentrations of fluoride have been linked to better caries prevention.(7,8,9) However, the use of toothpastes with high fluoride content is also associated with an increased susceptibility to develop dental fluorosis in children,(9,10,11,12) especially when implemented during early childhood (before 6 years of age).(13,14,15,16) Fluoride in toothpastes contributes with approximately 57 to 81.5% of the total intake of fluoride in children aged between 12 months and 6 years.(17,18,19,20,21,22,23) On the other hand, some authors have shown that using these products in children aged 3 to 8 years is related to a significant increase in the concentration of fluoride in urine after toothbrushing(24,25,26) and to the oral intake of fluoridated water in countries like Brazil.(27)
There has been an increase in the prevalence of dental fluorosis worldwide, with percentages ranging from 7.7 to 80.7% in areas with availability of fluoridated water and from 2.9 to 42% in areas with no fluoridated water.(28) Several studies have been conducted in Latin America, reflecting the prevalence of dental fluorosis in the region. In Mexico, in 2004, a prevalence of 56% was reported in school children aged 6 to 9 years (45% light level).(29) In Venezuela, in 2007, 16.6% prevalence was found in children aged 8 to 12 years (8.5% light level).(30) In Colombia, in 1998, a prevalence of 11.5% was reported (light and very light levels) in a population aged 6, 7, 12 and 15 to 19 years.(31) The IV Estudio Nacional de Salud Bucal (ENSAB-IV) carried out in 2014, reported 62.15% at age 12 and 56.05% at age 15.(32)
The Dean’s Community Fluorosis Index (CFI) in the Atlantic, Eastern, Central, Bogotá and Orinoco-Amazon regions in Colombia was 0.90 at age 12, showing that this population is in low risk, ranging from 0.6 to 1.0 in Dean’s CFI, while in disperse rural areas this index reaches 1.05, representing a moderate risk, which is considered a sign of alarm for public health action. This is also the case in the Pacific region, with an index of 1.06, highlighting the need to analyze the unwanted effects in the long run.(32)
As to the concerns about the increase in dental fluorosis prevalence, it is necessary to consider the multiple fluoride sources to which an individual may be exposed: toothpastes, cooking salt, solid foods, and liquid diet-especially water in countries where fluoride is added to drinking water-.(20,33,34,35,36,37,38,39,40,41,42) Authors like Levy et al suggest that a source associated with early childhood dental fluorosis is the fluoride ingested in toothpaste used during the development of permanent teeth,(43) and Löckner et al blame the increased risk to the application of fluoride varnishes simultaneously with the use of fluoride toothpastes.(26)
This topic review seeks to provide information on the type of therapeutic fluoride used in dentifrices, the abrasive material added to this fluoride, the academic recommendations about use and amounts, and variations according to different governmental regulations in Latin American countries. It also includes a description of the availability of products in the market of Medellín (Colombia), which conditions the use and monitoring of clinical recommendations. This information may help understand some conditions affecting the toxic and anti-caries effect of fluoride toothpastes in order to guide patients, since differences among the sources of information apparently create gaps that make it difficult to select and use toothpastes in children. Finally, this information can be used to help parents and guardians make an adequate, conscious, oriented, controlled, and monitored use of toothpastes, and to encourage the manufacturers of these products to be actively involved in consumers’ education.
METHODS
A bibliographic search was conducted in the Pubmed, LILACS, and SciELO databases since the beginning of creation of the databases until the publications made by May 30, 2017, to ensure exhaustiveness. According to the algorithm of each database, a search equation was used with the keywords “toothpaste”, “fluoride”, and “child” in English and Spanish. The equation used in the Pubmed database search was: ((children[Title/ Abstract]) AND toothpaste[Title/Abstract]) AND fluoride[Title/Abstract].
The obtained records were exported to the Zotero software applying the inclusion and exclusion criteria, for a final total of 38 articles to analyze (Figure 1).
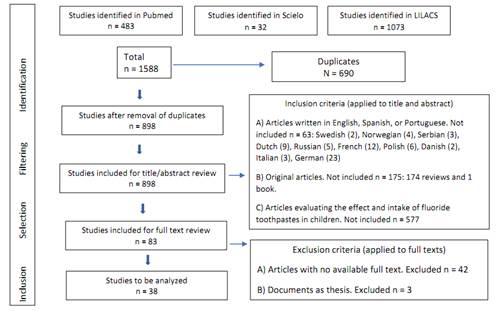
Figure 1 Methodology for topic review: used databases, retrieved records, inclusion and exclusion criteria
An additional search for guidelines and regulations regarding the use of fluoride in toothpastes in government archives was conducted, finding out information from the national ministries of health of Colombia, Brazil, Peru, Chile and Guatemala and from Mexico’s Secretary of Health. Documentation issued by American Dental Association (ADA), American Academy of Pediatric Dentistry (AAPD), American Academy of Pediatrics (AAP), European Academy of Paediatric Dentistry (EAPD), American Dental Association Council on Scientific Affairs (JADA), World Dental Federation (FDI), the Andean Community, and Mercosur was also retrieved.
RESULTS
Influence of dentifrices components in their preventive capacity
The preventive effect of dentifrices depends on their chemical characteristics and therefore on their components and the interactions among them.(44) These products contain a mixture of substances that vary in concentration depending on the intended objectives; among these substances are abrasives, which constitute 25 to 60% of a typical toothpaste.(45) Abrasives are insoluble particles that allow the mechanical removal of bacterial plaque; some examples are: dicalcium phosphate (CaHPO4), calcium pyrophosphate (Ca2P4O7), aluminium hydroxide (Al(OH)3), calcium carbonate (CaCO3), silicas, zeolites, and hydroxyapatite (Ca (PO ) OH).(45,46)
On the other hand, the therapeutic or active agents most commonly used for toothpastes are fluorides; the most widely used is sodium fluoride (NaF), followed by monofluorophosphate (MFP). Sodium fluoride is a highly ionizable compound, and therefore it becomes active as soon as it enters the mouth. In the case of MFP, fluoride is covalently bonded to the phosphate and for this fluoride to be active it must be released by enzymatic hydrolysis of the MFP molecule during toothbrushing by the action of phosphatases-enzymes that are normally present in both plaque and saliva-; this means that sodium fluoride releases fluoride ions immediately after it comes in contact with the oral environment, while MFP requires prior enzymatic action.(47,48)
There have been discussions about the effectiveness of these two types of fluoride in caries control. Some authors, such as DePaola,(49) Volpe et al,(50) and Basch et al,(51) conclude that no fluoride is superior than others and that their activity in caries control is equivalent; however, Churchley et al claim that there are significant differences in anti-cavity effectiveness of toothpastes with NaF and MFP, and that remineralization is related to the amount of fluoride on enamel.(48) It should be noted that fluoride absorption is conditioned by different excipients in the dentifrices,(44) since their compounds can be either active or inactive, and active ingredients can be inactivated, as is the case with NaF, which becomes quite ineffective as an anti-caries agent when calcium carbonate (abrasive) is bonded to it.(52)
Concerning the concentration of fluoride in dentifrices, and by regulations of the United States Food and Drug Administration (FDA), these products should have at least 60% of their content of total fluoride, as the sum of the soluble fluoride ion and soluble ionic forms, such as fluoride and fluorophosphates to NaF and MFP, respectively. Then the total content of soluble fluoride depends on the calcium contained in the abrasive of the toothpaste, which can form insoluble salts that do not contribute to remineralization.(53) Therefore, it is not possible for consumers to know the concentration of active fluoride in a given toothpaste, since the labels indicate the total concentration added to the product.(53)
According to the American Dental Association (ADA), one of the minimum requirements for a dentifrice to have the ability to control the carious process is to keep soluble and reactive fluoride. The general opinion is that toothpastes should have about 1000 ppm (average concentration), and hence 1450-1500 ppm are considered high concentrations, while 500 ppm is a low concentration.(54)
The activity of fluoride in dentifrice formulations should be assessed over time, since part of the MFP fluoride is released during storage and reacts with calcium forming insoluble fluoride. Some evaluations indicate that the anti-caries activity of these products remains for the time they are going to be used by the population,(55,56,57) but other studies suggest that in some cases the total fluoride declared in labels does not correspond to the actual concentration measured by gas chromatography,(58) and in some cases this is less than the total concentration of the formulation,(6,59,60) which further substantiates the need of surveillance and control programs. Manufacturers should provide information about the concentration of fluoride in its active form on the labels, in order to ensure the bioavailability within the concentration range suggested by the FDA, allowing a better approach to its true preventive potential.(53)
Quantity and concentration of dentifrice to use in children
The total daily intake of fluoride by an individual results from the combination of fluoride from the diet (solids and liquids) plus toothpaste fluoride and other supplements. The amount of fluoride ingested from toothpaste depends on the amount placed on the toothbrush and the concentration of fluoride in the toothpaste.(13,61,62) To reduce the risk of developing dental fluorosis, it is considered that the dose should not exceed 0.07 mg F/kg of body weight/day.(63)
Paiva et al(64) conducted an analysis of the total fluoride ingested by children aged 19 to 38 months (a critical period for the development of fluorosis in permanent incisors) in two Brazilian cities (Ibiá and Piracicaba). Both cities add fluoride to water (0.7 ppm), and the study only included children who drink water from public supply regularly. The authors found out that the children’s diet made a contribution of fluoride below the safe upper limit for the development of fluorosis, with variations depending on the children’s location, perhaps because of differences in nutrition patterns. Conversely, the amount of ingested fluoride from toothpastes was close to the upper limit of the dose accepted as safe for the development of dental fluorosis, which the authors blame to the use of a large amount of toothpaste and a greater frequency of toothbrushing by Brazilian children in comparison with those from other communities. These results are similar to those obtained by Lima et al, who found out that in a tropical Brazilian city (Teresina, Piauí) with access to fluoridated water, 74% of children aged 3 to 4 years consumed less than 0.07 mg F/kg of body weight/day, with variable contributions of diet and toothpaste, linking the same associated factors and suggesting that the amount of fluoride ingested is considered safe in termsofdental fluorosis risk.(65) Do Nascimento et al(66) estimated the intake of fluoride from toothpastes in children aged 2 to 6 years in a Brazilian city with no supply of fluoridated water (Campina Grande). The authors claim that the use of toothpastes is related to the risk of fluorosis in children, mainly due to improper use of toothpastes.
In search for safer strategies for fluoride toothpastes use in children, in 2014 the ADA(54) and the American Association of Pediatrics (AAP)(67) recommended -bearing in mind that 1 inch (equivalent to 2.5 centimeters and to 1 gram) of 1000 ppm dentifrice contains 1 mg of fluoride-to use a small amount of toothpaste (0.3 g/brushing, “similar to a pea”) in children aged 3 to 6, and an amount of the size of a “grain of rice” for children under 3 years starting as soon as the first tooth erupts (Figure 2), always under the supervision and help of an adult, who should indicate the adequate dose, taking into account individual needs, especially the risk of caries and fluorosis-although dentists may recommend its use in younger ages when the risk of tooth decay is higher-.
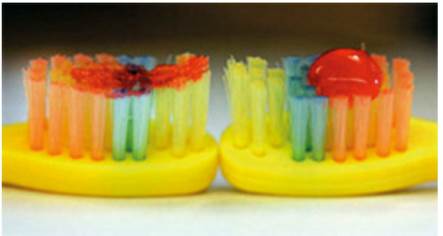
Figure 2 The photo on the left shows the amount of toothpaste recommended for children younger than 2 years (0.1 mg of fluoride) and the one on the right shows amount corresponding to a “pea”, recommended for children aged 2 to 6 years (0.25 mg of fluoride). Taken from American Dental Association Council on Scientific Affairs, 2014.
On the other hand, in 2009 the EAPD (European Academy of Paediatric Dentistry) issued some guidelines suggesting the use of 500 ppm dentifrices in children aged 6 months to 2 years, 1000 ppm in children aged 2 to 6 years, and 1450 ppm in children aged 6 years or older. These recommendations take into account the importance of accompanying parents in dosing and supervising toothbrushing until the child learns to not swallow the toothpaste, and thus avoid the risk of ingestion; it also shows the relevance of education programs aimed at parents,(68) and identifies children under 4 years (especially those aged 15 to 30 months) as the ones at greater risk of developing dental fluorosis in permanent incisors and first molars.(69)
According to the literature, dentifrices with low fluoride concentrations (between 500 and 600 ppm) are the most recommended to reduce total intake of fluoride in children.(70,71) Paiva et al(64) claim that this may be a partial measure because some children swallow large amounts of toothpaste (above 0.181 mg F/kg/day). These authors believe that 60% of the daily total consumption of fluoride can be attributed to toothpaste; therefore, a child exposed to a dose of 0.20 mg F/kg of body weight/day of a toothpaste with 50% less fluoride will be exposed to a dose two times greater than the safe upper limit for the development of fluorosis (0.07); it is then considered that the use of low-concentration toothpastes can reduce the risk of fluorosis in the majority of the population,(61,63) and that the amount of fluoride toothpaste should be reduced (to the size of a pea) in young children at risk of ingesting this substance.(72) It has been noted that toothpastes aimed at children are more expensive and therefore do not cover children from different socio-economic status, which is discriminatory, since most children would keep using the same toothpaste (less expensive) used by their parents or caregivers. The authors also argue that, while advertisements can make the product attractive to children, no product is specially designed for them.(64)
The evaluations of the anti-caries effect of low-concentration toothpastes under different conditions indicate that, in the case of children with active caries and individuals with a high exposure to sugar (6 to 8 times a day), or with high plaque rates, these toothpastes are less effective than conventional fluoride dentifrices (1100 ppm F).(59,73,74,75,76)
Arana and Villa(77) analyze the widespread use of toothpastes among families with children aged 3 to 5 years from the districts of Pesqueda, Mampuesto, and La Esperanza in the province of Trujillo, Peru, containing NaF, MFP, or both. The concentration of fluoride in these products is 1100, 1450, and 1500 ppm, but the authors found out abundant variations in the way labels describe the amount and concentration of fluoride. Most children in their study brush teeth more than twice a day with these toothpastes, agreeing with the findings by Paiva et al(64) and Lima et al(65) in Brazilian children. The evidence shows that fluoride toothpastes with higher concentrations offer more protection against tooth decay, but clearly these also increase the risk of fluorosis.(77,78,79) Studies conducted in Colombia and Mexico obtained similar findings to those of Paiva et al,(64) in which intake of fluoride through toothpastes represents up to 69% of the total fluoride intake, placing it above the value accepted as safe to prevent fluorosis.(80,81)
Arana and Villa(77) encourage health authorities to improve the control on these products and to standardize the way to describe their contents, in order to facilitate the reading and understanding of labels-a measure needed by both the final consumer and the dentist, who needs the best possible information available to guide and educate patients-.
The management of the amount of toothpaste to control fluoride intake makes sense considering the correlation between amount used and dose.(64,82) Paiva et al(64) point out that, if under the conditions evaluated in their study, a child uses 0.3 g of toothpaste each time he/she brushes, as recommended by the ADA,(54) the AAPD (American Academy of Pediatric Dentistry)(83) and the AAP,(67) this may be sufficient to reduce the intake of fluoride from toothpaste and to include children who are used to swallowing large amounts of toothpaste.(64) However, it should be noted that this contradicts what advertising displays; some packages and other forms of advertisement on the use of toothpastes show the entire brush head covered with toothpaste (approximately four times the recommendation for children).(51) Even for a well-documented dentist it is difficult to compete against advertising strategies that have been for so many years in the market, are widely distributed, invest so many resources, and suggest that all patients have the same needs and risks in oral health.
The frequency of daily toothpaste use has an impact on total fluoride intake;(64,65,66) in this regard, the EAPD in 2009(68) and the IDF (International Dental Federation)(84) in 2008 recommended using fluoride toothpaste twice a day, taking into account that children must spit during toothbrushing and rinse their mouth with some water after brushing to minimize swallowing; they also recommend maintaining supervision of children under 6 years and following the specific guidelines of national authorities for children under 3 years.(66,84)
Latin American countries’ regulations on the use of fluorides in dentifrices
Peru, Chile, Guatemala, Mexico, and the Mercosur Bloc (Argentina, Uruguay, Paraguay, and Brazil) have technical standards that set out the conditions for fluorides in toothpastes.(85,86,87,88,89,90)
In the case of Peru, Norma Técnica 2001 establishes that dentifrices with 1100 ppm of fluoride or more are suitable for children over 6 years and adults. They must have at least 600 ppm of soluble fluoride by manufacturing year and 450 ppm until expiration date. Toothpastes for children under 6 years must have 250 to 550 ppm fluoride concentration and at least 60% of soluble fluoride until expiration date, with a label including the “do not eat” warning. They must not include phrases that encourage eating the product and must have the phrase “children under 6 should use a small amount (size of a lentil) and must be supervised by their parents”. Dentifrices with 1100 ppm of fluoride or more should have the warning “not recommended for children under 6 years”. The advertisements of oral hygiene products should not suggest that the sole application or use of fluorinated agents guarantees the absence of tooth decay or controls the total development of bacterial plaque; and drawings or designs printed on the containers should not encourage product overuse.(89,90)
For its part, the Guatemalan standard sets 1003 ppm as a parameter for the concentration of total soluble fluoride if it is derived from MFP and 1086 ppm if it is derived from NaF, up to a maximum limit of 1500 ppm for both ingredients.(86)
The Mercosur Bloc (Argentina, Uruguay, Paraguay, and Brazil) has the “Technical Mercosur regulation on the list of substances that personal hygiene products, cosmetics, and perfumes must not contain, except under the conditions and restrictions laid down”, which indicates that toothpastes with 0.1-0.15% of MFP or sodium fluoride must include the following text on their labels: “children 6 years or younger: use an amount of the size of a pea under the supervision of an adult in order to minimize the risk of ingestion. If you receive a supplemental intake of fluoride from other sources, see your dentist or doctor”, unless it is already labelled as contraindicated for children (for example: “for adults only”).(88)
To the Mexican official regulation, the concentration of fluoride in toothpaste should not exceed 0.2% and should be lower than 0.05% in products for children under six years of age. It points out that dentifrices with a higher content of fluoride should be used in small quantities (“the size of a drop”) and under the supervision of an adult. The products of topical use included in this regulation must comply with the sanitary and commercial labelling requirements set out in NOM-137-SSA1-1995; dentifrices with a 1500 ppm concentration should include this text: “Children under 6 years should use 5 mm under the supervision of an adult. Avoid ingestion”. Dentifrices with a maximum concentration of 550 ppm should include the following text: “This toothpaste is recommended for children under 6 years; use 5 mm under the supervision of an adult. Avoid ingestion”.(85,87)
In Colombia, the highest concentration of fluoride in cosmetic dentifrices must be 1500 ppm for use by adults and 500 ppm for use in children under 6 years; if mixed with other fluorinated compounds, the fluoride concentration should not exceed 1500 ppm.(91) The text: “Contains sodium fluoride” must be included in all labels and all toothpastes containing 0.1 to 0.15% fluoride. Unless it is already labelled as contraindicated for children, it must necessarily have the message: “children 6 years or younger: use an amount of the size of a pea under the supervision of an adult to minimize swallowing. In case of fluoride intake from other sources, see your dentist or doctor”.(92)
In Chile, the 1993 technical standard established that fluoride concentrations in dentifrices should not be lower than 1000 ppm or higher than 1500 ppm for use by adults, and that the toothpastes for children under 6 years should have a maximum concentration of 500 ppm.(93)
This regulation was amended in 2015 with outstanding changes, such as the recommendation to use toothpastes with 1000 to 1500 ppm fluoride concentrations in the group of children under 6 years.(94) The standard based this modification on the greater protective effect of high fluoride concentration toothpastes compared to the ones with low concentrations (less than 600 ppm).(2,94,95)
It also states that the concentration of fluoride ion in ppm and the total fluoride content should be stated in the containers and boxes of dentifrices.(94)
For children under 6 years of age it suggests that oral hygiene should be done by an adult, or at least under their supervision, controlling the amount of paste and making clear that the child should not swallow it. It explains that the paste should be spread across the dry brush not exceeding the size of a pea (approximately 0.5 grams), using a smaller amount in children who cannot appropriately spit toothpaste remains.(94)
For dentifrices with less than 1000 ppm it recommends removing the text “children’s toothpaste” or “for children under 6”, and for dentifrices with 1000 to 1500 ppm of fluoride, it suggests including the phrase “in children under 6, use an amount equal to or smaller than the size of a pea, with supervision by an adult to avoid swallowing’. It also states that toothpastes should not contain phrases encouraging consumption, such as “tastes great”. (94)
Table 1 shows the fluoride concentrations that should be used in adults and children, according to each country’s regulations.
Table 1 Recommended concentrations of fluoride in dentifrices according to regulations in Latin American countries
| Country | Concentration of fluoride in dentifrices for adults | Concentration of fluoride in dentifrices for children |
|---|---|---|
| Peru | From 1000 to 1500 ppm | Less than 600 ppm |
| Chile | From 1000 to 1500 ppm | From 1000 to 1500 ppm |
| Guatemala | From 1003 to 1500 ppm | |
| Mexico | No more than 2000 ppm | 500 ppm maximum |
| Colombia | 1500 ppm maximum | 500 ppm maximum |
The evidence suggests that for government bodies in Latin American countries,(85,86,87,88,89,90,91,92,93,94) as well as in territories of North America and Europe, the excessive supply of toothpaste in small children remains a concern.(96)
Bearing in mind that terms like “pea”, “drop”, and “lentil” may be misleading because they are not unequivocal measures and are open to different interpretations, Creeth et al(96) recommended to unify the terminology to indicate the amount of toothpaste with the size of a “pea”, because it has been shown that this term correlates very well with the amount of weight in grams stated by the regulations (0.25 g). De Moura et al(97) suggest that it also necessary to offer education on the prevalence of dental fluorosis through programs for maternal and infant health, including advice on the appropriate amount of fluoride toothpaste in early childhood, because it has been shown that children whose parents participated in these programs had less prevalence of dental fluorosis.
Characteristics of the dentifrice market in Medellín (Colombia)
Since commercial availability determines what patients do, we reviewed the information from a database developed by the research group Patología Oral, Periodoncia y Cirugía Alvéolo-Dentaria (POPCAD) of the Universidad de Antioquia School of Dentistry, which includes a list of dentifrices available between 2013 and 2014 in five branches of one of the city’s largest chain store, verifying the type of fluoride and the concentration stated on each product’s label. This information was entered in a Microsoft Excel® 2010 worksheet and analyzed with version 22.0 of the IBM SPSS® software in order to explore and summarize the findings (unpublished data).
Eleven toothpaste brands were reported, with 45 references and different types of fluoride (Table 2); the concentrations most commonly used are those of 1450 ppm (44.4%), followed by 1100 ppm (22.2%), 1100/350 ppm (7.4%) and the ones lower than 1000 ppm (5.6%). Ramírez et al identified that, in the municipality of Frontino, Antioquia, conventional toothpastes contain fluoride at concentrations of 1504 ± 387 ppm,(34) similar to the toothpastes sold in the country as a whole, with fluoride concentrations ranging from 1100 to 1500 ppm.(98)
Table 2 Types of fluoride and frequency of use in the dentifrices most commonly sold in the city of Medellín, Colombia
| Type of fluoride | Frequency | Percentage |
|---|---|---|
| Tin fluoride / sodium fluoride | 5 | 9.3% |
| Sodium fluoride | 36 | 66.7% |
| Monofluorophosphate | 10 | 18.5% |
| Monofluorophosphate/sodium fluoride | 2 | 3.7% |
| Fluoride-free | 1 | 1.9% |
| Total | 54 | 100.0% |
Seven references of toothpastes especially designed for children were found, with labels warning that they should be used by children over 6 years, but whose presentation, smell, and taste are attractive to younger kids. Of these products, 42.9% were fluoride-free, 42.9% had NaF and 14.3% had MFP; the concentrations most commonly used are 0 ppm (42.9%), followed by 500 ppm (28.6%), 995 ppm (14.3%) and 1100 ppm (14.3%). These concentrations are similar to those found by Baez- Quintero et al in 17 dentifrices for kids sold in major supermarkets in Bogotá.(99)
Thus, the Colombian technical standard does not clarify the amounts of excipients as do the Ministries of Health of Peru and Chile with their technical standards indicating that “toothpastes for children must not contain flavorings, sweeteners, or colorants encouraging improper intake”.(89,94)
The various presentations of self-applied topical fluorides show differences in fluoride concentrations, volumes, and indications for use, so dentists must be familiar with them, in order to have a better criterion at the time of recommending them. The fulfillment of regulations in Colombia has not been sufficiently studied, and there are few studies evaluating dentists’ knowledge on dentifrices and recommendations of use;(4) and while some studies seek to assess caregivers or school educators in this regard, the role of the dentist has been neglected as a critical source of information for the community.(100,101,102,103)
Arrieta et al(102) demonstrated that dentists and dental auxiliaries of the local hospital at Cartagena de Indias have a poor level of knowledge and practices about dental fluorosis-a situation that has an impact on the orientation provided to the children’s caretakers-. In that same year, a similar situation was described by Ramírez et al(101) in a joint study with the Medellín Mayor’s Office: people were confused because of the different messages sent by dentists and auxiliaries about fluoride, fluorosis, and toothpaste use. The information caregivers received about the kinds of dentifrice children should use evidenced the variety of criteria that local professionals had at the time to recommending children’s toothpaste, as well as their relationship with commercial brands.
CONCLUSIONS
The anti-caries effect of dentifrices in children is subjected to changes related to the type and concentration of fluoride in these toothpastes. In the caseofchildren with active caries, highconsumption of sugar, or high plaque rates, conventional fluoride toothpastes should be used (1000-1500 ppm F), but when fluoride may have an adverse effect in terms of intake by small kids exceeding the permitted limits, one can use low-concentration fluoride toothpastes, implementing educational strategies that allow monitoring and proper control of dosage, concentration, and frequency of toothbrushing- variables that are of concern in several countries, including some Latin American nations-. In Colombia, the local market responds to the criteria of the regulation for dentifrices use, although the situation can be improved if the packages include explanatory information on the concentrations of bioavailable fluoride, the recommended amount and frequency of use according to age, and the risk for caries and fluorosis, indicating dosage by means of a photo like the one by the ADA, in order to improve safety in the use of these products in children. Finally, taking into account the particular landscape of prevalence of fluorosis in the country, the question is whether it would be reasonable to modify the regulations following the Chilean example, suggesting the use of a single term such as “pea” for a better correlation to the weight in grams of the amount of toothpaste indicated for children under 3 years of age.











 text in
text in 


