INTRODUCTION
Adolescence is a period of substantial emotional and physical changes, with many internal conflicts and an intense search for one’s own personal and social identity. The World Health Organization1 defines an adolescent as any person between ages 10 and 19. According to Colli2 in 1999, from the physical or biological point of view, adolescence encompasses the phase of anatomical and physiological modifications that transform the child into an adult. The term ‘puberty’ is used to refer to this whole process. From the psychological point of view, adolescence can be considered a period of changes mainly related to a search for identity and to the acceleration of intellectual development, as well as an evolution of sexuality.
In 1996, Fernandes and Marinho3 verified that, at the beginning of the 1980s, the Brazilian population consisted of 24% of adolescents, and by the year 2010 the authors estimated that nearly 36 million inhabitants were in this age group. According to the United Nations Children’s Fund (UNICEF),4 there are approximately 21 million adolescents in Brazil, representing 11% of the country’s population; as such, they are a significant segment of the population, with specific health care needs.
For Figueiredo et al5 in 2012, oral conditions represent one of the greatest health problems during adolescence. In spite of this, from the dental point of view, attention to the needs of adolescents is still lacking, especially in the behavioral aspect. Emotional and biological changes affect oral health not generally but in a specific way. Many lessons related to future behaviors and habits are learnt in this stage of life, and therefore it’s a crucial period for health care. This stage is the ideal time to develop a healthy lifestyle, consolidating the concept of self-care permanently. Because of the numerous transformations and discoveries taking place during adolescence, health care and hygiene habits are often neglected and considered of a minor importance.
Four national epidemiological oral health surveys have been conducted in Brazil, revealing the real health conditions of this population. Data from the Brazilian epidemiological survey SB Brazil 20036 exposed a dire landscape of adolescent oral health: about 14% of Brazilian adolescents have never been to the dentist. Alarmingly, the reason for seeing the dentist is usually the experience of dental pain, reported by almost one third of adolescents. The last epidemiological survey SB Brasil 20107 shows that advances have been slow and that the most common oral alterations in adolescents are caries, dental calculus, gingival bleeding, trauma, occlusal discrepancies, and fluorosis. Similarly, socioeconomic status was estimated, evaluating family income and schooling. This analysis confirmed the regional and social inequalities: the northern and northeastern states have lower socioeconomic status and schooling, as well as higher rates of oral alterations than the southern and southwestern states.4
Brazil has 16,27 million people in extreme poverty, and of these 53.3% reside in urban areas, representing 8.5% of the population. To establish the number of Brazilians living in extreme poverty, the government used preliminary data from the 2010 demographic census.8 The poverty line was established at US$50 per capita, considering the households’ monthly nominal yield. Therefore, any person living in a household with an income less than or equal to that value is considered extremely poor. In order to calculate the number of people with no income who are actually included in the poverty line, the Instituto Brasileiro de Geografia e Estatística (IBGE) also traced a line considering the following criteria: residence without a bathroom or with a collective bathroom, with no connection to the water distribution network, with no electric power, with at least one illiterate resident 15 years of age or older, with at least three residents up to 14 years of age, and at least one resident of 65 years of age or older.
According to Gambhir et al,9 oral diseases are among the most prevalent worldwide, and poor oral health conditions can have a significant impact on the quality of life of children and adolescents and harm the overall health of the individuals. In Brazil, caries is still an important public health problem, as stated in the latest epidemiological survey carried out by the Ministry of Health in 2010.7 This is because caries and periodontal disease are associated with social, economic, educational, and political conditions, beyond the conditions of the oral environment.10
Poorer people have worse dental and gingival conditions. The existing inequities, characterized by the higher prevalence of caries in poorer population groups, are persistent and reflect the deep social disparities in Brazil and their implications on the health of the population. It is then necessary to take steps to reduce the inequalities between and within countries, as proposed by the Commission on Social Determinants of Health.11
Dentistry has made great strides in recent decades; however, caries continues to affect the population early in life. Treatments often start in late stages, leading to the extraction of affected teeth. Today, early dental loss is known to be one of the main risk indicators for edentulism. This reality is a public health problem, evidencing the extreme importance of a medical specialty focused on the adolescent. Socioeconomic circumstances and family and individual conditions are known to interfere with the individual’s oral health status. According to the study conducted by Baldani et al12 in 2004, there is a significant correlation between income, housing, and schooling with dental caries.
In consequence, this study aimed to identify the socioeconomic level and the oral health profile (visible plaque, gingival bleeding, caries, and loss teeth) of adolescents living in an area of extreme poverty in the city of Viamão, Rio Grande do Sul, Brazil.
METHODS
This was an analytical transversal study in a sample of 205 adolescents living in Vila Augusta Meneghini, Viamão, Rio Grande do Sul. The city of Viamão is 23 km from the state capital and has a population of 239,000 inhabitants, while Vila Augusta has 2,000 people. The family heads are mostly garbage collectors. The locality has basic sanitation, lacks electric power, and suffers constant flooding due to the overflows of the Feijó creek, which crosses Vila Augusta. Violence and increased levels of drug use among young people are cited by locals as the biggest problems of this district.
The sample was obtained through home visits to 389 families (906 people), in which the youths’ parents or guardians signed a free and informed consent, responding to a questionnaire with socioeconomic information on the family head and general health data, such as daily sugar intake, number of daily meals, schooling, and home characteristics.
The oral health status of participating youths was assessed using the World Health Organization’s epidemiological survey codes and criteria.13 The oral examinations were performed by two trained examiners, using artificial light (common lamps of no specific trademark) and in the clearest area of the residences. The two examiners reached to an agreement on the diagnosis of each assessed adolescent (Figure 1). In calibrating the examiners, a percentage of disagreement of 15% was considered adequate, with a precision of 5% (± 5%) and a confidence level of 95%. This estimation of an 85% concordance index (Kappa) is considered almost perfect in the Landis and Koch classification.14
The visible plaque index (VPI) was measured, dental brushing was monitored (only by looking, without teaching specific brushing techniques), and gingival bleeding index (GBI) was observed, according to the Simplified Oral Hygiene Index (OHI-S) described by Greene and Vermillion15 in 1964, checking for bleeding points on the gingiva after brushing, at first sight. After dental prophylaxis and drying of the teeth with a gauze, the number of decayed, filled, and missing teeth was counted. Catheters and mouth mirrors No. 5 (SSWhite/Duflex) were used to perform the clinical examination.

Figure 1 Oral examination performed by two examiners in the clearest area of the residence, verifying the presence of visible plaque (VPI) and gingival bleeding (GBI) after dental brushing (photo by the author, 2017).
Home visits were scheduled for Saturdays, carried out by Community Health Workers (CHW) affiliated to the Augusta Meneghini Family Health Strategy (Estrategia de Salud de la Familia - ESF). The data collected were entered in a Microsoft Excel 2010 worksheet. Descriptive analyses were carried out for the demographic characterization of the population, by means of measures of central tendency (mode, median, and mean frequencies) and dispersion (standard deviation). The statistical analysis was carried out using Student’s t-test, considering a significance level of p ≤ 0.05, using the method of generalized linear models.
The project was approved by the Ethics Committee in Research of Porto Alegre’s Municipal Health Secretariat, with registration number 669 in the CEP and process No. 001.032690.11.8.
RESULTS
Of the 205 assessed adolescents, 83 were male (40.5%). The mean age of the sample was 13.8 years (standard deviation = 2.82), being individuals aged 10 to 19 years. Concerning socioeconomic variables, Table 1 shows that most adolescents come from families with an income of up to 1 minimum wage (53.2% of the sample). None belonged to families with an income of more than 5 minimum wages.
Table 1 Sociodemographic characteristics of 205 adolescents in conditions of extreme poverty living in Vila Augusta Meneghini, Viamão, Rio Grande do Sul, Brazil
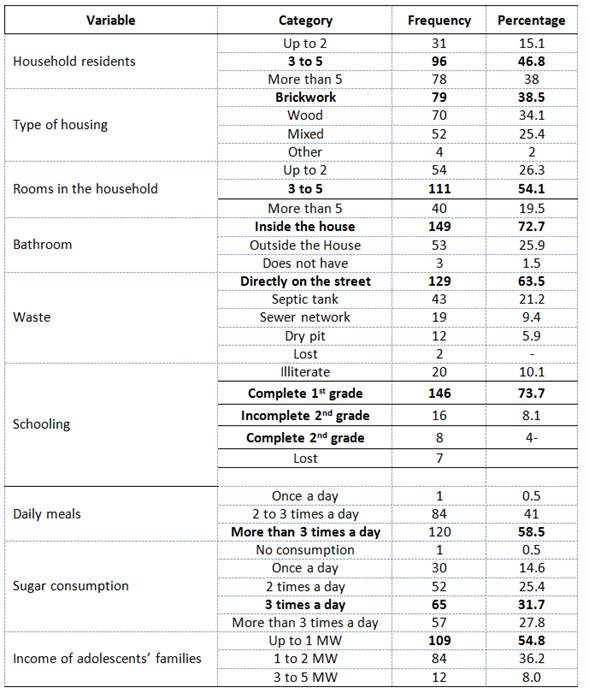
Table 1 also shows the characteristics of the homes where the adolescents live. As for the number of residents in the household, 46.8% live with 3 to 5 people. The types of housing most commonly informed by the adolescents were brickwork and wood, with 38.5% and 34.1%, respectively. 72.7% said that they have a bathroom inside the house, 25.9% outside of it and 1.5% do not have one. Similarly, more than 60% said that their homes’ waste goes directly to the street, while less than 10% indicated that the waste goes to the sewer network.
The study population of adolescents was characterized by living below the poverty line because their families survive with less than one minimum wage a month and most households have 3 to 5 residents in precarious situations. 10% of the sample was illiterate and more than 70% did not complete secondary school (Table 1).
Table 1 also shows that one of the teenagers has just one meal a day, while 84 have two to three meals a day (41%) and 58.5% feed more than three times a day. In terms of sugar consumption, Table 1 shows that just 1 teenager said not to eat sugar. The highest percentage of sugar consumption was 3 times a day (31.7%), while 27.8% reported consuming sugar more than 3 times a day.
Table 2 shows the oral health characteristics in terms of caries and periodontal disease. About 70% had visible plaque and almost 60% had gingivitis. The number of caries lesions ranged from 0 to 13, with an average of 1.9 per individual and a standard deviation of 2.82. In addition, there was an average of 0.52 restorations per teenager.
Table 2 Indicators of caries and periodontal disease of adolescents
| Descriptive statistics | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|
| Caries lesions | 0 | 13 | 1.90 | 2.28 |
| Restorations | 0 | 9 | 0.52 | 1.35 |
| Extractions indicated | 0 | 19 | 0.77 | 1.77 |
| Missing teeth | 0 | 12 | 1.74 | 3.78 |
| Lost teeth | 0 | 15 | 0.99 | 2.53 |
| Visible plaque | 0 | 18 | 1.20 | 2.87 |
| Gingival bleeding | 0 | 15 | I,30 | 1.89 |
Table 3 shows that there were no significant differences in average number of caries lesions among adolescents who received oral hygiene guidance or supervision and those who did not receive it. There was also no relationship between sugar consumption and family income.
Table 3 Comparison of the average number of caries lesions of adolescents
| Caries lesions | Mean* | Standard Error* | Standard Deviation* | p value* | ||||
|---|---|---|---|---|---|---|---|---|
| Guidance | No | 1.95 | 0.20 | 2.13 | 0.631 | |||
| Yes | 1.77 | 0.29 | 2.63 | |||||
| Supervision | No | 1.85 | 0.18 | 2.12 | 0.555 | |||
| Yes | 2.11 | 0.42 | 2.90 | |||||
| Sugar consumption | Once a day | 1.37 | 0.33 | 2.47 | 0.158 | |||
| 2 times a day | 2.44 | 0.40 | 2.64 | |||||
| 3 times a day | 1.63 | 0.26 | 1.56 | |||||
| More than 3 times a day | 1.96 | 0.32 | 2.46 | |||||
| Income | Up to 1 MW | 1.509 | 0.208 | 1.8448 | 0.075 | |||
| 1 to 2 MW | 2.298 | 0.3202 | 2.5354 | |||||
| 3 to 5 MW | 2.667 | 0.9472 | 3.2287 | |||||
* Student t-Test - Generalized linear models
Concerning tooth loss , table 4 shows that there were no significant differences by sex. It was found that those who had a monthly income of up to one minimum wage had average loss values relatively higher than those of other groups, although this difference was not significant (p = 0.341). In addition, there was no significant difference in the average number of lost teeth in relation to sugar consumption (p = 0.158).
Table 4 Relationship of dental loss with sex, monthly income, and sugar consumption
| Dental loss | |||||
|---|---|---|---|---|---|
| Mean* | Standard Error* | Standard Deviation* | p value* | ||
| Sex | Female | 0.967 | 0.089 | 1.683 | 0.158 |
| Male | 0.711 | 0.093 | 2.015 | ||
| Income | Up to 1 MW | 0.963 | 0.132 | 2.170 | 0.341 |
| 1 to 2 MW | 0.786 | 0.129 | 1.406 | ||
| 3 to 5 MW | 0.500 | 0.250 | 0.674 | ||
| Consumption of sugar | Once a day | 0.867 | 0.232 | 1.167 | 0.869 |
| 2 times a day | 0.980 | 0.195 | 2.627 | ||
| 3 times a day | 0.862 | 0.157 | 1.609 | ||
| More than 3 times a day | 0.772 | 0.155 | 1.488 | ||
* Student t-Test - Generalized linear models
DISCUSSION
The population of participating adolescents was characterized by living below the poverty line because their families survive with less than one minimum wage per month and most have 3 to 5 residents per household in precarious conditions. This reflects the reality of 16,27 million people living in extreme poverty, according to the latest census of the Brazilian Institute of Geography and Statistics.8 In their study, Rigo et al in 201116 found that the number of rooms in a house is a factor associated with tooth decay, i.e. living in better, larger residences with 6 rooms or more was considered a protective factor for tooth decay in schoolkids.
In consonance, Moreira et al in 200717 claim that the residence of individuals reflects their socioeconomic condition, and that along with the territory where one lives, it can influence both general and oral health. Thus, to characterize a population and its health problems, it is necessary to take this space into account.18 The present study showed a slight similarity among the residences, most of which are of brickwork (38.5%) and wood (34.1%). Most of the residences had bathrooms inside the house, and 63.5% of families throw the waste directly to the street. It can then be said that most surveyed adolescents live in precarious conditions, with high household density and in residences lacking basic sanitation. According to the latest census of the Brazilian Institute of Geography and Statistics,8 Vila Augusta had a high rate of violence, linked to drug trafficking and various crimes (such as thefts and robberies), committed mainly by adolescents and youths from the community. Other vulnerabilities include a large number of precarious houses, squatting, and constant rotation of the population as families often leave the area due to imminent risks.
The conditions found in the studied community reflect some findings of the literature; for instance, an inadequate diet and physical inactivity are important causes limiting the health of a population. Less than 50% of the surveyed adolescents practice some kind of physical activity, and nearly 60% have more than three daily meals associated with sugar consumption. These data corroborate those of Levy-Costa et al19 in 2005, who investigated family budgets, finding out that sugar consumption in families with lower income was 50% higher than that observed in families with higher income. Tomita et al,20 in 1999, claimed that the socioeconomic level influences the preference for sugar, and this in turn is associated with prevalence of dental caries in deciduous dentition.
On the other hand, there are high levels of dental caries among the study population, with nearly 2 decayed teeth per adolescent in average. Some studies have shown a direct relationship between the level of caries prevalence and social indicators in populations with low income and low schooling levels. Viana et al,21 in 2009, analyzed schooling levels and family income in relation to dental caries, finding out that individuals with incomplete primary school and monthly family budgets lower than 5 minimum wages had worse oral conditions in relation to caries. For Granville-Garcia et al,22 the socioeconomic conditions have a big influence on variables such as time for tooth brushing, number of daily brushings, latest dental visit, and reason for consultation.
With regard to unhealthy gingival conditions, 70% of participating adolescents have visible plaque and 60% suffer from gingivitis. Although Chambrone et al23 in 2010 observed that the prevalence of gingival diseases does not depend on socioeconomic status and is directly associated with poor oral hygiene, some other studies claim that the prevalence of gingival bleeding is associated with socioeconomic conditions.24
In order to provide healthcare to adolescent patients, surgeon dentists should not consider the clinical procedures alone, as this is not sufficient to modify the youths’ habits and to restore their biopsychosocial well-being.25 Compostella,26 in 1984, claimed that dentists should not treat adolescents like adults nor as children; the dental professional must be aware of their dependence and independence crises, and thus show proper behavior when adverse behaviors arise. The author suggests that dentists must show firmness to demonstrate authority, but never authoritarianism in dealing with any situation. The interpersonal relationship between the adolescent patient and the professional must be established through dialogue and respect.
The obtained data suggest that most adolescents did not receive any type of dental care, although the Augusta Meneghini Basic Health Unit in Vila Augusta has two dentists. It has been observed that, in dealing with adolescents from less privileged social classes, the public health system fails to provide universal dental care. This has been advocated by the General Coordinator for the Health of the Adolescent and Youth, of the Ministry of Health, which deals with issues related to youth and adolescents aged 10 to 24 years, in terms of health promotion, protection, and recovery.27
The situation becomes even more serious when overall tooth loss is considered, not reaching the extreme situation of edentulism. In this study, the average was 1 tooth per adolescent, the same proportion found in the 2004 National Epidemiological Survey.6 The present study included 205 adolescents aged 13 years in average, most of them female. In relation to tooth loss, there was no significant difference between genders, suggesting that the difficulty in keeping oral health in adolescence does not depend on gender. It could be then perceived that personal appearance does not seem to be a concern for the studied adolescents, since teeth were not considered as a resource to look more beautiful, for social acceptance, or self-esteem. This contradicts all the literature; Baldwin28 pointed out in 1980 that a large number of studies have documented the health effects of attractiveness in interpersonal relationships and that appearance is key to success in relationships. The author cites several works that clearly show the concern of adolescents with appearance and its relationship with self-image and self-esteem.
Caries distribution is heterogeneous; there are differences among regions and social groups, and the experience of this disease is more severe in population groups subjected to social marginalization.29 This study found that the socioeconomic conditions of these adolescents are related to dental losses, in addition to biological processes. Loosing dental units is perhaps the worst consequence of this disease, due to its functional or aesthetic consequences. The high level of tooth loss affects not only the functionality of dentition, which can create masticatory and speech problems, but also the quality of life and the individual’s self-esteem and socialization.30)
Capra,31 in 1982, calls to mind that health is a multidimensional phenomenon involving physical, psychological and social aspects in an interdependent manner. Based on this concept, the importance of oral health for the studied adolescents should involve all these dimensions: the physical aspect, because they express “pain” and the need to be able to “chew well”; the psychological aspect, evident in the importance of personal appearance: “to be more attractive for girls”, “not to be called a toothy”, “to have beautiful teeth to kiss”; and the social aspect, as they put it: “because of bad breath, they need to keep personal distance”. Therefore, we believe that the knowledge acquired and accumulated by dental surgeons for so many years should be transmitted through health education and interdisciplinary work.
The present study also showed the great need to adapt public health policies in the studied region, as the needs of young people are not being met, and this population groups is being neglected. Because of the precariousness of the system, it should be noted that the effective participation of young people in the formulation of public policies is critical for a real commitment of all those involved in guaranteeing the right to health.
It is important to mention that the work in the community has been fruitful, as it has helped us have a picture of the real needs of adolescents and to understand the real motivations that drive them to seek dental care. This knowledge may lead to effective health education programs to achieve the long-desired goals in oral health, regardless of the youths’ socioeconomic status.
Finally, the present study had strengths and limitations related to working in a context of social vulnerability that produces passive, dependent adolescents and families, with low self-esteem levels. These young people and their families referred to the shortcomings in their historical-social condition as negative aspects. This cycle has installed itself in a circular and almost inevitable way, reinforcing the condition of misery, not only in the material but also the affective dimension. Also, the care provided to these young people was gratifying to the professionals in charge of the study because we know that for them it is extremely difficult to overcome the situation of abandonment.











 text in
text in 


