INTRODUCTION
Despite the numerous campaigns of health authorities in Ecuador and other countries in the region, tooth decay remains a constant problem.1,2 This situation is generally solved by means of restorative interventions,3 with relatively high costs due to the required materials and human resources, in addition to the relative short life of these materials once placed in the patient’s mouth.4 Several studies have shown that the longevity of these materials largely depends on the oral hygiene of patients.5,6
It is therefore critical to modify the approach used to provide patients with comprehensive care once caries lesions occur.7 In this context, it is essential to accompany patients with constant reinforcement of oral hygiene procedures and techniques.8-12
This study aimed to evaluate the effectiveness of motivational talks on oral hygiene practices addressed to parents or guardians of children aged 5 to 8 years, and its relationship with the integrity of direct composite resin restorations, in a 24 months follow-up period.
MATERIALS AND METHODS
Study design and ethics
A descriptive, prospective, controlled, single-blinded study was carried out with prior approval of the Research Ethics Committee of Universidade Federal do Rio Grande do Sul in southern Brazil, with number 806,674 as part of a multicentric program led by this university, and registered following the CONSORT's recommendations (Consolidated Standards of Reporting Trials), identified as TRIAL: RBR-7JY2F7. An informed consent document was handed out to the persons responsible for each kid, in which they accepted their free and voluntary participation; signing this document was considered an essential requirement to participate in this study. Identification data and follow-up results for each child were stored and identified by participant.
Sample size and recruitment
Convenience sampling was used to establish the sample size after requesting participation of various schools. Participants were recruited as they arrived at the dental clinic in Cumbayá, Quito (Ecuador), where this study was conducted. Candidates were evaluated by a dentist trained in dental caries diagnosis, who oversaw the selection of participants-a process that lasted for about three months. Children aged 5 to 8 years with similar economic and cultural situations were thoroughly examined, considering their parents’ education level and their families’ income, until finding 31 children with teeth meeting the inclusion criteria (Table 1). Each parent or guardian was explained the methodology to be used, the benefit and possible risks of the treatment, as well as the parties’ commitment as described in the informed consent, which was duly signed by each child’s parent or guardian.
Table 1 Inclusion and exclusion criteria
| INCLUSION CRITERIA | EXCLUSION CRITERIA |
| Children aged 5 to 8 years whose parents accept their participation by signing an informed consent. | Children under 5 years and over 8, without an informed consent. |
| Kids with deciduous cavitated molar teeth, with the presence of antagonist and proximal tooth. | Deciduous molar teeth without occlusal and proximal contact. |
| Active caries with deep dentin involvement. | Active caries with enamel or pulp involvement. |
| Absence of clinical or radiographic signs of pulp lesion. | Presence of clinical or radiographic signs of reversible pulpitis, pulp necrosis, pulp exposure, fistula, edema, mobility not related to rhizolysis (root resorption), radiolucency at the furca region, periapical, or spacing of the periodontal ligament. |
| Presence of 2 mm of excess dentine between the pulp chamber and the floor of the cavity after caries elimination, radiographically determined. | Absence of 2 mm of excess dentine between the pulp chamber and the floor of the cavity after caries elimination, radiographically determined. |
All the deciduous molars were subjected to clinical and radiographic evaluation, verifying the presence of occlusal contact and active carious lesions involving deep dentine, as well as the absence of clinical diagnosis of reversible pulpitis, pulp exposure, fistula, edema, or mobility not related to rhizolysis (root resorption); radiographic absence of radiolucency at the furca region and periapical area; spacing of the periodontal ligament or presence of necrosis, and the existence of 2 mm between pulp chamber and cavity floor, radiographically determined.
In addition to meeting the inclusion criteria, the selection of the sample considered that the parents or guardians had the same economic and cultural situation, determined by their education level, family income, and the willingness to participate in the study. Thus, 31 participants and 46 deciduous molar teeth were included in the study.
Clinical interventions
The clinical procedures in all participants were performed by the same dentist who conducted the sample selection, who received in vitro and in vivo training and was previously standardized in the technique of caries removal and restorative treatment. The clinical intervention of the participants’ teeth was carried out during one restoration session. Once anesthetized and under absolute isolation, the cavities were accessed by means of high-speed carbide burs 1011/1012 (KG Sorense, Brazil). If required, decayed tissue was removed with sharpened dentine curettes (Maillefer, Brazil) and low-speed burs (SS White, USA), starting by the side walls and finishing by the pulp wall, until reaching remaining hard dentin tissue. Teeth with pulp exposure were excluded from this study. The endodontic treatment was then started.
After total removal of decayed tissue, a thin layer of calcium hydroxide cement (Dycal, Dentsply, Brazil)13 was applied on dentin tissue, followed by immediate full conditioning using 37% phosphoric acid (3M ESPE, USA) for 15 seconds on enamel and 7 seconds on dentine, rinsing and wiping the cavity.14 The adhesive system (Single Bond 2, 3M ESPE, USA) was then placed using an active technique and light curing for 20 seconds with a LED light lamp (Valo; manufactured in the United States) at a distance of 1 mm; increments of 2 mm of composite resin (Filtek Z350 XT Color A1B, 3M-Espe-USA) were added, light curing each as recommended by the manufacturer, until achieving final restoration. In the case of restorations involving proximal walls, a contoured metal matrix was used, adapted by means of wooden wedges. After removal of absolute isolation, initial polishing was done with plastic sanding strips for the interproximal sides (Microdont, Brazil) and abrasive tips for the occlusal side (Jiffy® Polishers, Spain). Final polishing was performed eight days later, following the same protocol and materials. As a control, a bite-wing X-ray was taken, verifying the absence of pathology; this was considered as the baseline.
All participants, parents and guardians were given dietary indications, as well as motivation and lessons in hygiene practices, by means of talks and the modified Bass brushing technique using didactic aids and a brushing model, and later in the participant’s mouth; each participant was given a dental hygiene kit with a toothbrush and toothpaste. During the evaluation period, each participant and their parents or guardians were reminded of the educational procedures every six months.
Assessment
The clinical evaluations of each participant were carried out by a single qualified and previously trained evaluator, different from the operator, in each of the 5 periods: at baseline and 6, 12, 18 and 24 months after the intervention. The clinical evaluation of the restorations was performed considering aspects such as aesthetics, fracture, retention, marginal adaptation, sensitivity, and surrounding caries, using a score of 1 to 5, where 1 was considered excellent and 5 very poor. The participants’ oral hygiene was assessed by the visible plaque index (VPI) and the gingival bleeding index (GBI), passing a periodontal probe along the surfaces of each tooth with a 45º inclination in gingival direction. These were interpreted as clinical signs of response to the motivation and education on oral hygiene offered to parents or guardians throughout the study.
The data were collected in specifically designed tables, following the protocols suggested by CONSORT, respecting confidentiality and anonymity by providing each participant with a code. The statistical analysis was carried out using the ANOVA test and Student’s t-test, using the STATA 13.0 software for Windows and comparing the groups in terms of primary and secondary variables, with 95% significance level.
RESULTS
Data from the 31 participants examined were analyzed every 6 months for two years: at baseline and in four subsequent evaluations. In the five analysis periods, 197 measurements were taken, distributed among 15 girls and 16 boys averaging 6.73 years in age, with a difference in the number of treated molars, which was 1.6 times greater in boys than in girls. 46 measurements were taken at baseline; however, 24 months later the measurements reduced to 30.
Concerning the included teeth, 48% were upper molars and 52% lower molars, and the measurements concentrated in the first mandibular molar (34.5%), followed by the second maxillary molar (26.4%).
The VPI decreased over treatment time, with an average of 21.3 at baseline, while at 24 months the average decreased to 8.6. It was also observed that a minimum mean (of 5.5) was reached at 18 months, compared with the other periods (Figure 1).
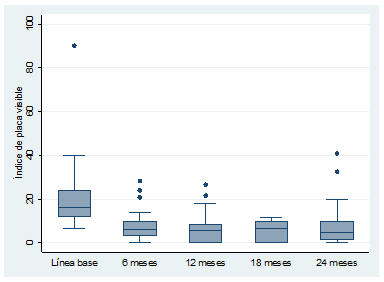
Figure 1 Visible Plaque Index boxplot. [Traducción de figura: Visible Plaque Index Baseline 6 months 12 months 18 months 24 months]
With respect to GBI, the baseline starts with an average of 5.2, reducing to 1.5 at 24 months, similar to what was observed with the VPI. The minimum value of gingival bleeding index was reached at 18 months, with an average of 0.7 and p = 0.000. On the other hand, the Student t-test shows a significant difference of p = 0.2019 for VPI and p = 0.6243 for GBI when correlating the periods assessed against baseline data, but not among the evaluation times in both variables (Figure 2).
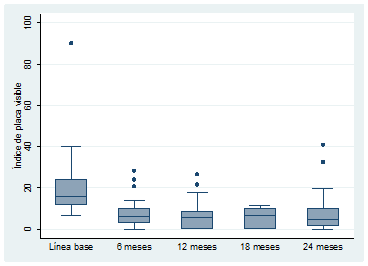
Figure 2 Gingival Bleeding Index boxplot. [Traducción de figura: Gingival Plaque Index Baseline 6 months 12 months 18 months 24 months]
On the other hand, considering the dental surface involved and the clinical indicators established by the International Dental Federation (IDF) for restorations, the increase in failure percentage becomes evident as the number of surfaces increases in direct relation with the time of the restoration in mouth (p = 0.05). The statistical analysis by Student’s t-test helps compare the averages of surfaces between baseline and 24 months, showing that failure percentage increases when two surfaces are involved, more significantly on the occlusal-mesial surface (Table 2).
Table 2 Percentage of failure per technique according to surface
| Technique | Surface | Average failure | Standard error | Standard deviation | Confidence interval at 95% | Student’s t-test | p value | |
|---|---|---|---|---|---|---|---|---|
| Aesthetic | Occlusal-distal | 42.86% | 0.2020 | 0.5345 | -6.58% | 92.29% | -2.1730 | 0.0420 |
| Occlusal-mesial | 57.14% | 0.2020 | 0.5345 | 7.71% | 106.58% | -2.1183 | 0.0525 | |
| Fracture and retention | Occlusal-distal | 42.86% | 0.2020 | 0.5345 | -6.58% | 92.29% | -2.1730 | 0.0420 |
| Occlusal-mesial | 57.14% | 0.2020 | 0.5345 | 7.71% | 106.58% | -3.2404 | 0.0059 | |
| Marginal adaptation | Occlusal-distal | 42.86% | 0.2020 | 0.5345 | -6.58% | 92.29% | -3.1980 | 0.0045 |
| Occlusal-mesial | 57.14% | 0.2020 | 0.5345 | 7.71% | 106.58% | -3.2404 | 0.0059 | |
| Surrounding cavities | Occlusal-distal | 42.86% | 0.2020 | 0.5345 | -6.58% | 92.29% | -3.1980 | 0.0045 |
| Occlusal-mesial | 42.86% | 0.2020 | 0.5345 | -6.58% | 92.29% | -2.4303 | 0.0291 | |
DISCUSSION
It is clear that motivational talks and education on hygiene techniques have an influence on the longevity of restorations, represented by the VP and GB indexes. In this context, our results highlight the need for the dental training centers in Ecuador to incorporate caries risk analysis (and its control once the disease has started) in the teaching-learning processes,15-18 by means of procedures of hygiene and elimination of biofilm both at the dentist’s office and at home.1,2,19,20
The results of the present study show deterioration of restorations over time, agreeing with the findings by other authors18 and demonstrating the influence of the oral conditions where the restored tooth is on the restorative material used, as well as its integration with the dental structure as a mechanism to prevent the viability of remaining bacteria and their progression towards the pulp.21-25 All this in addition to the failures caused by the aging of the restoration and the properties of the restorative material,26 which in this study was observed by considering the five clinical criteria used, showing that the deterioration of the restoration was the least frequent, suggesting that the restorative technique was properly and carefully performed.
However, the failures at the interface were the most frequent, showing a clear association between the characteristics of the material, its composition and fatigue25 and the characteristics of the oral environment where it is located12 (directly related to the presence of bacterial plaque, established by the VPI), which were decisive for the presence of marginal failures of restorations,1 especially in those where the number of restored dental surfaces involved proximal surfaces.27,28 Due to its organic composition, the dentine found at the superficial surface of the gingival wall is more susceptible to deterioration by the action of the existing acids in the dental biofilm,26 possibly causing pulp lesions, which in this study were few in number and limited to cavities covering two surfaces, as corroborated by the initial radiographic analysis.
It is clear that the training in teeth brushing offered to parents or guardians reduces VPI and GBI in the participating children, directly influencing the quality of the performed treatments and highlighting the importance of involving patients and their caregivers in the restorative process, by means of education and motivation in oral hygiene techniques.27-29
The surgical protocol for lesions in deep dentine traditionally taught in dental schools in Ecuador is based on a correct clinical and radiographic diagnosis,12-14 followed by the total removal of decayed tissue, placing or not a base cavity or pulp protector, depending on the case, as well as a restorative material.29,30,31,32 The high demand of patients entering these restorative circles can be seen in epidemiological studies conducted in Ecuador,32 where caries prevalence in deciduous teeth in children aged 6 to 8 years is about 79.8%, suggesting the influence of oral hygiene as a determinant factor for the presence of secondary caries33 and indicating that the presence of dental biofilm has a direct relationship with the deterioration of the restoration and its interface,5,34 affecting its durability and even the vitality of the pulp-dentin complex. 23,32-34
The prior assessment by the dental professional and the subsequent motivation offered to the patient are effective tools in convincing the patient that the restorative procedures alone are not enough to treat the disease, since no restorative material can be considered as the right treatment for tooth decay, despite the excellent properties or techniques used to eliminate the disease.
Despite all the strategies developed by different health agencies worldwide, tooth decay remains one of the most common problems among school children.(24, 25) Minimally invasive therapies have been widely accepted21,26,27 as they seek to preserve dental tissue; however, when the lesion is already established and compromises dentin tissue, operative treatments are the appropriate therapy.13,23,28
The teaching in our dental schools is still based on operative procedures as a control and treatment tool, which merges with the imaginary of the general population that considers that a treated tooth does not require additional care. This study aimed to intervene in this imaginary, raising awareness among parents or guardians on oral hygiene as a fundamental tool for the maintenance of restorations, in accordance with other studies that highlight the need for constant mentoring,12,29) using oral hygiene devices1,2,12,29,30 and fluorinated elements.24-26
One of the limitations of the present study is the use of a small sample, probably related to the fact that parents or guardians downplay the maintenance of deciduous teeth, in addition to the strict standardization of participants in terms of economic and cultural level, considering the parents’ educational level and family income. Therefore, new similar studies need to include different economic and cultural groups.
Several reports show the association between motivation and maintenance of restorations; however, no study has conducted a 24 months follow-up, probably because of the difficulties of conducting prolonged mentoring due to sample loss, associated with the fact that parents or guardians usually downplay the maintenance of deciduous teeth, as evidenced in the present study despite the constant motivation provided.
It is necessary to propose a restructuring of the teaching methodology and the operative protocols within dental schools as training centers, promoting the prior analysis of patient’s risk as the first process before conducting any surgical procedure, in conjunction with the motivation of patients and their caregivers in oral hygiene procedures and care, seeking to break the rooted paradigms and the imaginary of our patients. All this leads to thinking about the need to carry out similar studies, both in design and methodology, including different economic and cultural groups.











 text in
text in 


