INTRODUCTION
Post-treatment periapical disease (PPD) is defined as the onset or persistence of periapical pathology once an endodontic treatment has been completed.1 According to the literature, endodontic failure occurs in 38% of all cases on average,(2) requiring a secondary endodontic intervention. In this situation, there are two therapeutic alternatives: orthograde retreatment or endodontic microsurgery (EM)-indicated as a surgical alternative when retreatment fails or cannot be performed-.3 With a success rate ranging from 78 to 92%, EM can access periapical tissue with magnification, illumination, ultrasonic instruments, and regenerative retrograde filling materials.4,5
In Colombia, the mandatory health insurance plan (plan obligatorio de salud, POS), under Resolution 5857 of 2018,6 states that specialized dentistry includes “the excision procedure on an odontogenic lesion […] and other corrective endodontic procedures”, as a practice subjected to agreements by Health Maintenance Organizations (HMOs) (entidades prestadoras de salud, EPS).6 In order to promote a controlled practice, the Ministry of Health and Social Protection states that “All induced and mandatory activities, procedures, and interventions must design or adopt technical standards and healthcare guidelines for relevant diseases”,7a statement that validates the development of Clinical Practice Guidelines (CPGs), defined as evidence-based documents aimed at establishing the most appropriate health care procedures when dealing with a clinical condition.7,8
Evans et al (2012)9 published some EM standards, but methodologically speaking the document cannot be considered a CPG to be adapted nationwide, and therefore a de novo10,11 CPG needs to be developed for the surgical endodontic management of PPD (CPGEM).
That being said, in recognizing the prevalence of PPD2 and understanding the preservation of natural teeth as the main objective of dental specialties, the purpose of this study was to make evidence-based recommendations to support the practice and quality of EM as an effective treatment of PPD.
The final CPGEM document will be a product with an impact on dental schools, endodontics programs, practitioners, endodontic service providers, and especially on patients consulting health care reference centers for EM therapy because of PPD.
METHODS
The development of this document was approved by the Universidad Nacional de Colombia Ethics Committee (Minutes 20-15). The Guidelines Developing Group (GDG) was formed with an endodontist and two graduate students leading the projects within the Graduate Endodontics Program at the School of Dentistry (Posgrado de Endodoncia de la Facultad de Odontología Universidad Nacional de Colombia, PE- FOUN). The stages for the development of the document are shown in Figure 1, including the selection of “Microsurgical treatment of PPD” as subject, and the formulation of objective, scope, and 11 questions in either PICO (Patients-Inter-vention-Comparison-Outcome) or PECOT (Population-Exposure-Comparison-Out- come-Time).11
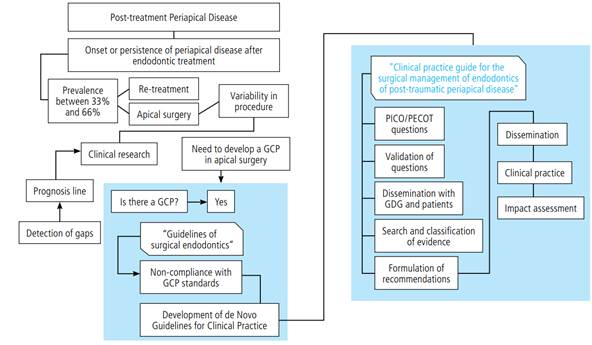
Figure 1 Algorithm representing the phases for the development of the CPGEM. Adaptation of the original in: Methodological directions for the creation of clinical practice guidelines with economic assessment in Colombia’s General Social Security System in Health. Final full version - Methodological Guidelines Update Group 2014-11
The methodology complied with the principles of clinical validity and reliability through a multidisciplinary review of each question and dissemination for correction and re-formulation by endodontic experts who served as consultants in CPG methodology10,11 and two PPD patients in need of EM seen at PEFOUN.
OUTCOME CATEGORIES
In accordance with the Grading of Recommendations Assessment, Development and Evaluation (GRADE),12 each question’s expected impact was quantified by identifying the outcomes, like this: 1. “critical”, for anesthetic effect, pain control, infection control, hemostatic effect, and treatment success or failure. 2. “significant but not critical”, for reduction of healing time.
The GDG conducted a systematic search of literature in the period October 2015-October 2017 in the following databases: Science Direct, Medline via PubMed, Embase via OVID, Lilacs, SciELO via Bireme, Trip Database, as well as in the tables of content of endodontic journals. The search sought highly sensible answers to the questions asked, selecting secondary studies first, like meta-analysis (MA) and systematic literature reviews (SLR) and then primary clinical studies, like randomized controlled clinical trials (RCT), cohorts, and case controls, all with EM as subject.6
A search equation was explored for each question, and a first screening by title identified the abstracts to be evaluated. Differences between evaluators were resolved by a third evaluator, finally selecting the articles that were read in full text. For each selected publication, validity was determined according to methodological standards and relevance for answering the questions. Tools like Measurement Tool to Assess Systematic Reviews (AMSTAR)(13) for SLR and MA, and The Scottish Intercollegiate Guidelines Network (SIGN)(14) for clinical studies helped qualify the validity of each study. Finally, GRADE was used to rate the quality of the evidence and the strength of the recommendations, as high, moderate, low, or very low.12
On October 26, 2016, a consensus meeting with endodontic experts, professors, and members of scientific organizations disseminated the document and submited it for external evaluation, generating recommendations for the established outcomes. In the absence of scientific evidence for certain topics, good clinical practice points were considered when the desirable effects outweighed the undesirable effects, as “clinical common sense”.11
DISCUSSION
The construction of these CPGEM aimed to establish agreed, evidence-based behaviors in controversial topics that have a direct influence on the clinical outcome of EM as an alternative treatment of PPD.
There was unanimous consensus in the identification of PPD,15-16 with categories like pathological process,28-30 occurrence of intraoperative accidents,31,32 anatomical conditions,33,34 and existing restorations35 indicating the practice of EM generally accepted and clarified by experts and interns, all of whom understood the recommendations (questions 1 and 2).
As for the implementation of different anesthetic solutions (question 3), the evidence65,66 exclusively focuses on either inferior dental nerve block in symptomatic pulp pain or extraction of third molars. This shows the lack of evidence for anesthetic options in EM.
The use of magnification systems, ultrasound technology, and regenerative retrograde filling materials is common in EM; 4 however, access to such technologies is limited in the country (questions 4 and 6). The legalization of bioceramics in Colombia67 overcomes opportunity barriers in terms of use, dissemination and future production of knowledge to support the evidence.
As an intraoperative factor, bleeding control (question 5) is a fundamental step for EM success; however, the evidence is not conclusive or innovative. The exploration of new alternatives like laser beam or natural polysaccharides is not yet demonstrated by the available experience due to the limited access to these techniques or because of the little existing evidence.
The consensus, based on existing literature and experience, does not recommend using regenerative techniques in EM,54,55 as it increases costs and unnecessarily triggers periapical bone repair (question 7). As an additional contribution, the discussion also included the influence of the pre-surgical state of supporting tissue as a risk factor to EM failure.64
On the other hand, the pre-surgical use of analgesics and antibiotics does not establish an effect on the outcome. The American Endodontic Association highlights the indiscriminate use and lack of clarity in criteria.68 The consensus unanimously decided against presurgical medication (questions 8 and 9) in systemically stable patients.
Finally, the recommendation of pre-surgical CBCT imaging, as a predictor of success in EM, was considered a “good practice point”. Even though the evidence in this regard is still low, the sensitivity and information offered by a prior three-dimensional image was considered a step in the good direction before the surgical approach. In addition, the existence of time-dependent factors indicates the need to evaluate EM at periods longer than one year.
CONCLUSIONS
Carried out by a multidisciplinary team, the CPGEM can be considered a supporting reference tool for general dentists, endodontists, and patients in need of therapeutic decisions for PPD. It includes recommendations, good practice points, and healthcare barriers as a support to university units and reference centers promoting the practice of EM. The CPGEM contributes sufficient evidence on issues affecting decision-making, case selection and quality of procedure.