INTRODUCTION
Pneumatization refers to the development of air-filled cavities or air cells in bones, which may exist in various locations of the skull, including the temporal bone.1-6 Five regions have been described in it: middle ear, mastoid apophysis, peri-labyrinth, petrous apex, and accessory.1,7,8
The pneumatization of the temporal bone performs important functions, such as protecting the inner ear from external air pressure changes, reducing the skull’s weight by acting as a buffer against external injuries, and enabling the exchange of gases from the blood mucus barrier in mastoid cavities, which provides stable pressure in the middle ear, a key function in the transmission of sound.9,10
The term pneumatized articular tubercle (PAT) of temporal bone, first introduced by Tindall and Matteson,11 refers to the accessory cells at the root of the zygomatic arch and the articular tubercle (AT), with the following radiological characteristics: 1) they form an asymptomatic radiolucent defect in the temporal zygomatic apophysis with a mastoid cell-like appearance, 2) they spread up to the AT without going beyond the zygomatic-temporal suture, 3) absence of increased volume or signs of zygoma destruction.
The cause of PAT is still unknown but may be similar to that of other pneumatized areas, such as mastoid apophysis, with the most popular theory for it being the resorption of the diploe by active invasion of the tympanic epithelium. Pneumatization of the mastoid apophysis is almost complete by the age of five, but air cells can develop into adulthood. The zygomatic apophysis cells are formed after age nine, but there is no certainty as to at what time they begin to form in the AT.1,8,12
PAT can be observed in orthopantomography, which was considered the initial method for examining AT due to its low cost and low radiation dose compared with tomographic imaging.1,2,4,11,13-24 However, the latter is not likely to overlap with anatomical structures as in conventional imaging, and they exceed the diagnostic accuracy in the evaluation of air spaces in the temporal bone.3,6,5,10,25,26
The roof of the temporal mandibular fossa (MF) is a thin sheet of bone separating the temporomandibular joint (TMJ) from the middle cranial fossa, with thickness ranging from 0.2 to 4.0 mm.27,28 This thickness difference may be due to the spatial resolution of the imaging method, the ratio of the image plane to the object being observed, the measuring tool used, the origin of the sample, and even by the conditions of the TMJ under study.28-30 In our practice, we have seen interrupted cortical fossa roof in multi-slice computed tomography (MSCT) images, suggesting the presence of fine channels or small cavities in the MF, as stated by Carter et al14 and Eckerdal et al.31 This possible anatomical variation will be called “discontinuity of the mandibular fossa” (DMF) in this study.
Identifying these anatomical variants is important because they form areas of minimal resistance in the temporal bone, possibly enabling the extension of tumors, inflammation, infection or fracture of the TMJ,1,6,12,16,32-35 and complicating surgical procedures in the joint.5,6,13 In consequence, the present study is aimed at evaluating PAT and DMF through CT, with a focus on their distribution by age, sex, and laterality.
METHODS
Sampling
This was a descriptive, retrospective, field study using a convenience sample of CT images from 200 patients: 151 females (75.5%) and 49 males (24.5%) requiring examination of maxillo-mandibular structures in the period January 2012-May 2013. As inclusion criteria, images showing both temporomandibular joints were used, excluding cases with facial abnormalities, pathologies, surgical procedures, or trauma in surrounding areas.
The patients were aware of their images being used for teaching and research purposes, so they signed an informed consent for this study, guaranteeing anonymity. Being a retrospective study, it was not deemed necessary to consult the institution’s Ethics Committee.
Procedures and techniques
Obtaining the tomographic images
All images were obtained in a 16-channel multi-slice CT scanner (Brightspeed, GE Healthcare, WI, USA), with patients in supine position and support for the skull, which was perpendicularly located by Camper’s plane towards the scanner’s table. Prior preparation of patient was not necessary. The images were obtained using the following parameters: slice width: 0.625 mm, pitch: 0.3 mm, 120 Kv, 100 mA, FOV for head, with bone tissue filter.
Analyzing tomographic images
Digital Imaging and Communications in Medicine (DICOM) images were analyzed by a single examiner-a maxillofacial radiologist with more than 15 years of experience in the field-using an Advantage Workstation (AW Volume Share 5, GE Healthcare, WI, USA) to obtain volumetric images in Multiplanar Reconstruction (MPR) and 3D, in order to assess the joints’ axial, sagittal and coronal planes. The observer was previously calibrated using 10% of the sample in order to define the criteria for the identification of PAT and DMF.
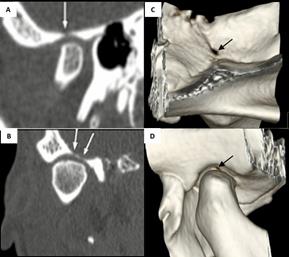
Data on each patient’s age, sex, presence or absence of PAT and presence or absence of DMF were recorded, as well as the laterality of the findings (unilateral or bilateral). PAT was verified in the presence of one or more hypodense images similar to mastoid cells, with no evidence of increased size in the anatomical structure nor destruction of the cortical (Figure 1), according to the criteria set forth by Tyndall and Mateson.11 DMF was verified in cases in which there was a hypodense zone at the center of the cortical, belonging to the fossa roof (Figure 2), confirmed with observations in the sagittal and coronal planes. As information was recorded for both TMJs, 400 joints were available.

Source: by the authors
Figure 1 Extension of the pneumatized articular tubercle of the temporal bone as seen in CT images. In A, B and C, pneumatization is limited to the tubercle. In D, E and F pneumatization goes on to the bottom of the mandibular fossa.
Source: by the authors
Figure 2 A. Sagittal view and B. Coronal view in CT images, showing (white arrows) the presence of discontinuity of the bottom of the mandibular fossa. Volumetric reconstruction in 3D, C. Endocranial view, D. Endocranial view, showing discontinuity (black arrows).
In addition, a literature review was conducted in PubMed and Google Scholar, in the search for possible series reporting the prevalence of PAT or DMF in the period 1980-2018, using the following key words: “articular eminence”, “pneumatization”, “articular tubercle pneumatization”, “zygomatic air cell defect”, and “zygomatic process”.
RESULTS
The distribution of the sample per age is shown in Table 1, with the highest percentage of patients in the group of 20- 29 years (n = 45, 22.5%). The average age was 41.6 ± 23.4 years. 19% of individuals had any of the studied variants, with 28 cases in females and 10 in males (Table 2). The frequency of PAT was 15.5%, with 21 cases (67.7%) in females and 10 (32.3%) in males. Concerning DMF, only seven patients showed the anatomical variant, with all being females (Figure 3).
Table 1 Sample distribution by chronological age
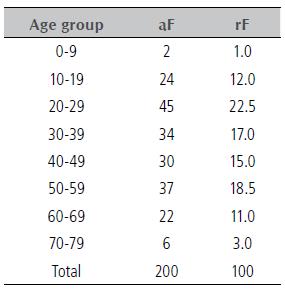
aF: absolute frequency, rF: relative frequency (%)
Source: by the authors
Table 2 Frequency of anatomical variants of the temporal component of the temporomandibular joint by sex
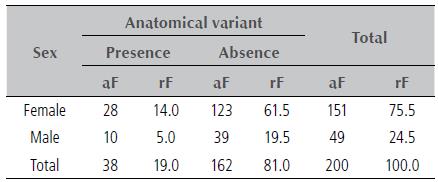
aF: absolute frequency, rF: relative frequency (%).
Source: by the authors
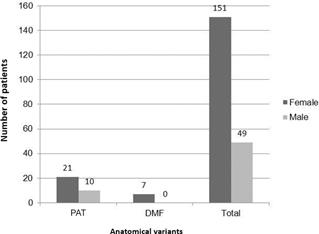
Figure 3 Distribution of pneumatized articular tubercle (PAT) and discontinuity of mandibular fossa (DMF) by sex
Table 3 shows the distribution according to the presence or absence of variants per age group. It shows that no patient under the age of 10 had any of the variants. PAT was verified in the age range of 10 to 79 years (average age 42.83 ± 21.27). DMF was verified in the age range of 20 to 79 years (average age 49.5 ± 18.44). Concerning uni or bilateral localization (Table 4), most cases with PAT were bilateral, while DMF occurred unilaterally.
Table 3 Frequency of anatomical variants of the temporal component of the temporomandibular joint by age group
| Age groups | Anatomical variant | Anatomical variant | Anatomical variant | Anatomical variant | Anatomical variant | Anatomical variant | Total | Total |
|---|---|---|---|---|---|---|---|---|
| PAT | PAT | DMF | DMF | Absence | Absence | |||
| aF | rF | aF | rF | aF | rF | aF | rF | |
| 0-9 | 0 | 0.0 | 0 | 0.0 | 2 | 1.0 | 2 | 1.0 |
| 10-19 | 6 | 3.0 | 0 | 0.0 | 18 | 9.0 | 24 | 12.0 |
| 20-29 | 7 | 3.5 | 1 | 0.5 | 36 | 18.0 | 44 | 22.0 |
| 30-39 | 5 | 2.5 | 1 | 0.5 | 27 | 13.5 | 33 | 16.5 |
| 40-49 | 4 | 2.0 | 1 | 0.5 | 26 | 13.0 | 31 | 15.5 |
| 50-59 | 4 | 2.0 | 2 | 1.0 | 32 | 16.0 | 38 | 19.0 |
| 60-69 | 4 | 2.0 | 1 | 0.5 | 18 | 9.0 | 23 | 11.5 |
| 70-79 | 1 | 0.5 | 1 | 0.5 | 3 | 1.5 | 5 | 2.5 |
| Total | 31 | 15.5 | 7 | 3.5 | 162 | 81.0 | 200 | 100 |
PAT: pneumatized articular tubercle; DMF: discontinuity of the mandibular fossa; aF: absolute frequency; rF: relative frequency (%)
Source: by the authors
Table 4 Frequency of anatomical variants of the temporal component of the temporomandibular joint per laterality
| Anatomical variant | Unilateral | Bilateral | ||
|---|---|---|---|---|
| aF | rF | aF | rF | |
| PAT | 15 | 48.4 | 16 | 51.6 |
| DMF | 6 | 85.7 | 1 | 14.3 |
PAT: pneumatized articular tubercle; DMF: discontinuity of the mandibular fossa; aF: absolute frequency; rF: relative frequency (%)
Source: by the authors
DISCUSSION
There are numerous air-filled cavities inside the skull in addition to the sinuses. These air cells or pneumatization may appear in different locations, including the temporal bone,1 where the cells are usually limited to the mastoid apophysis, peri-labyrinth and petrous apex, with rare cases of extensions to the squamous part.36
It has been noted that the development of air cells is preceded by the formation of bone cavities, a physiological process related to periosteal activity. The primitive bone marrow in these cavities differs in lax mesenchymal tissue, and the epithelium invaginates into this connective tissue, producing a mucous membrane which becomes atrophied, leaving a thin lining membrane adhered to the periosteum. The recession of this membrane and the sub-epithelial resorption of bone increase the air cells.1,16
The pneumatization process can be divided into three stages: 1) a childhood stage from birth to the age of two years, 2) a transitional stage from two to five years of age and 3) an adult phase. During the childhood stage, the air cells begin to be visible since the age of two years, in the transitional stage the mastoid undergoes a gradual increase with migration of cells to the periphery, becoming more noticeable over time due to the progressive calcification of their walls. Pneumatization stops in the adult phase.16 The pneumatization process usually begins prenatally during the 22-24 weeks of gestation. By week 28, the petrous apex begins to pneumatize, and the pneumatization pattern of the temporal bone is completed by the age of 10 years in females and 15 years in males.8
According to the literature reviewed for this study, PAT shows a prevalence of 1.90% in orthopantomography, varying from 1.03 to 3.60% in the reported series, in an age range of 6 to 90 years, with 32.32 years in average, showing a slight predilection for males and the bilateral form (Table 5). Concerning CT and CBCT findings, PAT prevalence was 27.68%, the age range was 5 to 85 years, with 38.45 years in average and bilateral cases being more common (Table 6).
Table 5 Incidence of pneumatized articular tubercle (PAT) of the temporal bone observed in orthopantomography, as reported in the literature
| Year | Author | Sample | PAT (%) | Age range | Mean age | Sex | Laterality | ||
|---|---|---|---|---|---|---|---|---|---|
| Female(%) | Male(%) | Unilat(%) | Bilat(%) | ||||||
| 1985 | Tyndall & Matteson11 | 1061 | 28(2.6) | 15-74 | 32.5 | 15(53.6) | 13(46.4) | 5(17.9) | 23(82.1) |
| 1986 | Kougar et al13 | 784 | 8(1.8) | 32-69 | 45.9 | 7(87.5) | 1(12.5) | 4(50.0) | 4(50.0) |
| 1999 | Carter et al14 | 2734 | 40(1.5) | 17-83 | 49.6 | 20(50.0) | 20(50.0) | 32(80.0) | 8(20.0) |
| 2001 | Hoffman et al15 | 1084 | 20(1.8) | 77-87 | 43.2 | 11(55.0) | 9(45.0) | 16(80.0) | 4(20.0) |
| 2005 | Orhan et al1 | 1006 | 19(1.8) | 11-90 | 36.6 | 12(63.1) | 7(36.9) | 12(63.1) | 7(36.9) |
| 2006 | Orhan et al16 | 1049 | 17(1.6) | 7-16 | 11.2 | 8(47.1) | 9(52.9) | 10(59.0) | 4(41.0) |
| 2009 | Yayuz et al2 | 8107 | 83(1.0) | 10-75 | 26.9 | 41(49.4) | 42(50.6) | 56(67.5) | 27(32.5) |
| 2010 | Srikanth HS et al17 | 600 | 15(2.5) | 20-50 | 30.2 | 8(53.3) | 7(46.6) | 9(60.0) | 6(40.0) |
| 2012 | Park et al18 | 1400 | 31(2.2) | 9-55 | 27.5 | 9(29.0) | 22(70.9) | 24(17.4) | 7(22.6) |
| 2012 | Gadda et al19 | 400 | 11(2.7) | 18-65 | 33.9 | 5(45.4) | 6(54.5) | 1(9.1) | 10(90.9) |
| 2012 | Patil et al20 | 7755 | 141(1.8) | 19-75 | 36.9 | 50(35.4) | 91(64.5) | 107(75.8) | 34(24.1) |
| 2012 | Zamaninazer et al4 | 2600 | 94(3.6) | 6-81 | 27.40 | 59(62.8) | 35(37.2) | 70(74.5) | 24(25.5) |
| 2013 | Gupta et al21 | 800 | 46(5.7) | 4-60 | 31.43 | 17(36.6) | 26(63.4) | 16(34.8) | 30(65.2) |
| 2014 | Srivahsa et al22 | 1688 | 50(2.9) | 7-18 | 13.86 | 27(54.0) | 23(46.0) | 38(76.0) | 12(24.0) |
| 2015 | Kishore et al23 | 2500 | 63(2.5) | 19-78 | 37.40 | 25(39.6) | 38(60.3) | 44(69.8) | 19(30.1) |
| 2016 | Nagaraj et al24 | 600 | 16(2.7) | 10-59 | 25.00 | 6(37.5) | 10(62.5) | 11(68.7) | 5(31.2) |
| Total | 37991 | 750(1.9) | 6-90 | 32.32 | 359(47.8) | 388(52.1) | 497(66.2) | 250(35.7) |
Unilat: unilateral; Bilat.: bilateral
Source: by the authors
Table 6 Incidence of pneumatized articular tubercle (PAT) of the temporal bone observed by computed tomography methods, as reported in the literature
| Year Author | Sample | Method | PAT (%) | Age | range | Mean Age | Sex | Laterality | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Female(%) | Male(%) | Unilat (%) | Bilat.(%) | |||||||
| 2011 | Miloglu et al3 | 514 | CBCT | 41(8.0) | 5-62 | 30.6 | 25(61.0) | 16(39.0) | 31(75.6) | 10(24.4) |
| 2013 | Ladeira et al5 | 658 | CBCT | 140(21.3) | 11-85 | 43.0 | - | - | 76(54.3) | 64(45.7) |
| 2014 | Bronoosh et al25 | 225 | CT | 43(9. 5) | 8-67 | - | 24(55.8) | 19(44.1) | 24(55.8) | 19(44.1) |
| 2015 | Ilguy et al26 | 111 | CBCT | 73(65.8) | - | 48.8 | - | - | 31(27.9) | 42(72.1) |
| 2017 | Shamshad6 | 100 | CT | 12(12.0) | 18-65 | 34.9 | - | - | 8(66.6) | 4(33.3) |
| 2018 | Khojastepoor et al10 | 327 | CBCT | 251(76.7) | 9-65 | 30.5 | 112(44.6) | 139(55.4) | 76(30.3) | 175(69.7) |
| 2018 | Presente estudio | 200 | CT | 31(15.5) | 10-79 | 42.8 | 21(67.7) | 10(31.2) | 15(48.3) | 16(51.6) |
| Total | 2135 | 591(27.6) | 5-85 | 38.4 | - | - | 261(44.1) | 330(55.8) |
CBCT: cone beam computed tomography; CT: computed tomography; Unilat: unilateral; Bilat.: bilateral
Source: by the authors
In comparing the results obtained in the present study with previous studies using tomographic imaging methods, it was found out that the frequency of PAT was close to that reported by Shamshad et al6 (12%), higher than that reported by Miloglu et al3 (8%) and Bronoosh et al25 (9.6%), and lower than the values observed by Ladeira et al5, Ilgüy et al26 and Khojastepour et al10 (21.3%, 65.8%, 76.7% respectively). Concerning mean age, it was similar to that found in the studies by Ladeira et al5 and Ilgüy et al26 (43.0 and 48.9 years respectively). The minimum age observed for the anatomical variant was close to that reported by Ladeira et al5 (11 years), Bronoosh et al25 (8 years) and Khojastepour et al10 (9 years), suggesting that pneumatization begins before puberty. As for the maximum age, it was slightly higher than that verified by Miloglu et al3 (62 years), Bronoosh et al25 (67 years) and Shamshad et al6 (65 years) and lower than that observed by Ladeira et al5 (85 years). In terms of sex, most reports, including the present study, show a predilection for females. Bilateral cases were most frequently observed in this and in all studies consulted. Concerning the variations found compared to other studies, these may be due to the source of the sample (dental clinics or other health centers), the age composition of the sample, the criteria for assessing PAT, the ethnic origin of selected patients,6 as well as the type and brand of the tomographic equipment.
The various reports on PAT prevalence seem to reflect the impact of the imaging method used for observation; thus, the frequency of PAT observed in tomographic studies is undoubtedly higher than that found in orthopantomography (Tables 5 and 6), and while PAT is visible in the latter, the least superficial mean portion of AT can only be observed in CT or CBCT, which probably influences the number of cases identified through them.
PAT should be differentiated from other types of radiolucency in the zygomatic arch, including aneurysmal bone cyst, hemangioma, giant cell tumor, eosinophilic granuloma, fibrous dysplasia, and metastasis. While PAT can be incidentally detected in X-rays as asymptomatic radiolucent images of non-expansive characteristics, all the other conditions present a painful increase in size and radiographically show a destructive appearance.3,5,12
It has been reported that the correlation between actual bone thickness and that shown by CT is high for structures of one millimeter or more, while those with dimensions below the spatial resolution of the equipment show a progressive difference between such thicknesses. Also, in clinical situations, the inclination of the bone wall varies in relation to the image plane, demonstrating that the combination of a bone wall with less than one millimeter in thickness and an inclination of 35° results in an image bigger than the actual thickness.29,30 In such circumstances, over-estimation would risk overlooking the presence of DMF. Moreover, it should be noted that the discontinuity of the cortical is a very thin bone that cannot be observed due to the size of the voxel;28 therefore, future research should seek the characterization of this possible anatomical variant of the temporal bone, as well as the influence of imaging parameters and the type of CT scanner used.
The importance of identifying these anatomical variations is that if bone thickness is reduced by the air cells or there is a discontinuity in the cortical, the extension of pathological processes in the TMJ would be facilitated due to the lower resistance in the area, so that tumors in the mastoid process and the ear could spread into the joint, while otitis or mastoiditis, as they involve the joint, would result in ankylosis of the joint.1,5,28 On the other hand, it has been found that the presence of air in the TMJ may be associated with acute fracture of the temporal bone,25,32,33 because surgical procedures performed on a temporal bone with such variations, as well as those performed on the mandibular bone component of TMJ or related soft tissues, could be complicated by unintended penetration of instruments, which may result in dural leakage, brain-spinal fluid leakage, intracranial infection or hemorrhage.3,10,12,25 It has also been noted that an extensive PAT could be a contraindication for tuberclectomy or tubercleplasty.3,25
In conclusion, CT helped identify PAT and DMF, studied anatomical variants with areas of minimal resistance that can facilitate the spread of pathologies and lesions of the TMJ to the median cranial fossa, as well as contraindicate a number of surgical acts that while altering their integrity could establish the aforementioned communication.














