INTRODUCTION
Telemedicine refers to the provision of medical care with Information and Communication Technologies (ICTs) to conduct diagnostics, consider treatments, prevent diseases, and strengthen the network of professionals and research activities in rural and hard-to-reach communities.1,2 Similarly, in dentistry, an innovative method called tele-dentistry has been developed, providing clinical care through electronic dental records and remote ICTs as an opportunity to raise awareness, promote education and provide patients with professional services.3-6
This concept was first implemented in dentistry in 1997 by Cook,4 who used video conferencing for diagnosis and remote treatment consultations, and managed to exchange clinical information and images.7 Currently, this alternative is still in development as a promising tool to identify the presence of injuries and perform teleconsultation in school programs, rural areas, and areas with limited access through different devices such as smartphones, portable x-rays, social networks, and in various specialties such as endodontics, oral surgery, periodontics, and public health, proving to be more efficient and with high demand in the provision of health services, thus reducing inequality in dental clinical care.8,9
Globally, research projects like the ones conducted by Kale S, Kakodkar P, Shetiya SH10 in India assessed mothers’ abilities for health education regarding the diagnosis of tooth decay, using smartphone photographs, which were sent through a social network. Each child’s diagnosis was requested, with significant changes for mothers, who made improvements in the diagnosis of their children’s dental condition.
In Latin America, specifically in Brazil, Fonseca et al11 evaluated the correct diagnosis of the presence of oral lesions and diagnoses conducted remotely through digital images obtained with a cell phone, showing improved efficiency and higher demands in the provision of health services and a decrease in inequalities in dental clinical care.12,13 In Colombia, the concept of telehealth was implemented through Law 1419 of 2010, as a means of supporting the General System of Social Security in Health (Sistema General de Seguridad Social en Salud, SGSSS), in order to support health service providers in terms of equity in care, improved access to health services, and quality of life in vulnerable areas.14
However, the implementation and applicability of telehealth to date is still inconclusive because the development and application of these remote methods are recent, and therefore teledentistry is still unknown to many professionals, preventing the population from receiving the benefits of these practices. Therefore, a systematic review of the literature was conducted to determine the impact of teledentistry applications in various specialties in clinical practice based on available scientific evidence.
METHODS
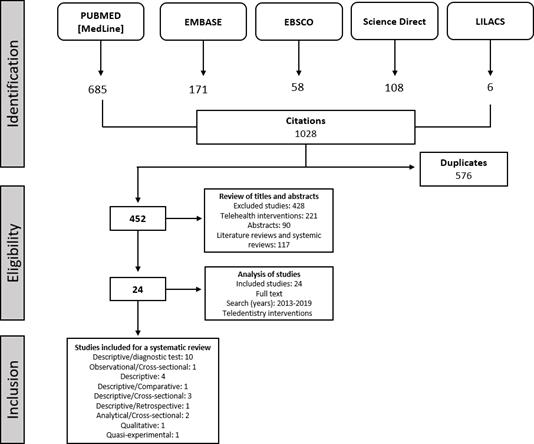
A systematic search of the literature was conducted to describe and summarize the information available on the applications of teledentistry, following the PRISMA-P guidelines (2015).15
Eligibility Criteria
Eligible studies were independently selected by two reviewers who used titles and abstracts, including descriptive analysis, cross-sectional studies and/or interventions in relation to teledentistry, published in the period 2013 to August 2019, available in full text in English, Spanish or Portuguese. Other study types, such as literature reviews, systematic reviews, or documents submitted as editorials or books were excluded.
Search Strategy
Eighteen bibliographic searches were carried out using the PubMed, EMBASE, EBSCO, ScienceDirect and LILACS databases from 2013 to August 2019. These searches were carried out through the combination of the following keywords: “teledentistry AND education distance”; “teledentistry AND health promotion”; “teledentistry AND oral health”; “teledentistry AND NOT telemedicine”; “teledentistry OR telehealth AND health promotion AND oral health”; “telehealth AND telemedicine AND teledentistry”; “teledentistry AND oral health”; “tele-medicine AND teledentistry”; “telemedicine AND oral health”; “teledentistry AND health promotion OR oral health”; “tele-odontología AND educación a distancia”; “teleodontología AND salud oral”. The search strategy was adapted for each database.
Selection of studies and data extraction
For the selection of studies, two authors examined the publications’ titles independently and in duplicate based on the eligibility criteria; then the abstracts were accessed, deciding which articles to include. In the second evaluation stage, the articles were obtained in full text and evaluated by the two authors, who agreed by consensus on the final inclusion.
The selected articles were broken down in an evidence table (Table 1). The first reviewer extracted each full text, while the second reviewer independently verified the extracted data and resolved the discrepancies generated at this stage.
Table 1 Characteristics of included studies
| First author | Year | Country | Context | Population involved | Research design | Outcome (Area to evaluate) | Tool used |
|---|---|---|---|---|---|---|---|
| AlKlayb18 | 2017 | Saudi Arabia | Doesn’t report | Mothers | D | Oral health | Mobile app (iTeethey™) |
| Bhatts19 | 2018 | India | Rural area | Adults | C | Oral cancer / Cervical cancer | Interview |
| Birur20 | 2019 | India | Industrial zone | Adults | A | Oral cancer | Mobile app |
| Boringi21 | 2015 | India | University | Dental professionals and students | D | Knowledge and beliefs | Questionnaire |
| Daniel22 | 2017 | United States | Schools | Children | D | Tooth decay | Photographs |
| Almeida23 | 2017 | Brazil | University | Children and adults | DT | Dentoalveolar trauma | Photographs |
| Estai24 | 2017 | Australia | Rural area | Dentists, dental students, dental therapists, nurses | D | Tooth decay | Questionnaire |
| Estai25 | 2016 | Australia | Doesn’t report | Adults | DT | Oral diseases | Mobile app |
| Estai26 | 2016 | Australia | Dental clinic | Children and adults | DT | Tooth decay | Mobile app |
| Giradeau27 | 2017 | France | Prison | Prisoners | DT | Oral health | Camera (Soprocare®) |
| Haron28 | 2017 | Malaysia | Doesn’t report | Adults | DT | Oral cancer | Mobile device |
| Jung29 | 2018 | South Korea | University | Adults | DT | Tooth decay | Digital Fluorescence (QLF-D) |
| Kohara30 | 2018 | Brazil | University | Teeth extracted, Children | DT | Tooth decay | Mobile device |
| Martin31 | 2016 | United States | Doesn’t report | Dental Professionals | D | Telehealth | Questionnaire |
| McFarland32 | 2017 | United States | Rural area | Students in dentistry, oral health, and other health professions | D | Teledentistry | Questionnaire |
| McLare33 | 2016 | New York | Rural area | Children | D | Teledentistry | Teledentistry consultation |
| McLaren34 | 2016 | New York | University | Children | D | Dental treatments | Teledentistry consultation |
| Morosini35 | 2014 | Brazil | Prison | Adolescents | DT | Tooth decay | Photographs |
| Paixcao36 | 2018 | Brazil | Health centres | Teleconsulting | D | Teledentistry | Database |
| Puhorit37 | 2017 | India | Rural area | Children | DT | Tooth decay | Camcorder |
| Roxo38 | 2017 | Australia | Distance education | Dentists, nurses, dietitians | A | Oral cancer | Virtual course |
| Skandarajah39 | 2017 | India | Health centre | Adults | PB | Oral cancer | Mobile microscope |
| Van Hilsen40 | 2013 | United States | Doesn’t report | Teeth extracted | QE | Tooth decay | Midwest Caries IDTM (MID), Visual Photo Examination (CAM), Cross-polarization Optical Coherence Tomography (CP-OCT). |
| Vinayaga-moorthy41 | 2019 | India | Rural area | Adults | O | Oral cancer | Mobile App (WhatsApp) |
D: Descriptive; DT: Diagnostic Test; A: Analytical; CE: Quasi-experimental; O: Observational; C: Qualitative
Source: by the authors
The selected aspects for each article are classified by first author, country, context, study sample, study design, outcome, and tool used for the application of teledentistry.
Bias risk in individual studies
Bias risk was assessed according to each study type, verifying cross-sectional studies through a checklist by the Agency for Healthcare Research and Quality (AHRQ)16 and randomized clinical trials through the list of items for publication of the Cochrane Collaboration Tool.17
RESULTS
The search strategy identified 1028 articles, of which 24 were included in this systematic review (Figure 1). There were 23 cross-sectional studies and 1 intervention study. Each study is detailed in Table 1.
Most studies were conducted in the United States and India, as well as in countries in South America, Asia, and Oceania. As for population type, the rural area was predominant. In terms of the intervened population, eight studies were performed in adults, four in children, two in children and adults, and one in adolescents. Other studies were in students, dental professionals, and other health-related professions; there were in vitro studies (teeth removed), and studies conducted in prisoners and teleconsultation. Concerning the area to evaluate, eight studies indicated tooth decay as the main outcome, followed by oral cancer with six studies. Finally, in determining the tool used for each study, an application or a mobile device was used in eight studies.
Results of cross-sectional studies
In total, seventeen (70.8%) of the 24 evaluated studies mentioned teledentistry as an alternative method in rural areas, health centers, and prisons for diagnosing and treating oral diseases such as oral cancer, tooth decay, and dentoalveolar trauma through different means such as applications and mobile devices: iTeethey™, WhatsApp, Remote-I, mobile microscope, digital fluorescence (QLF-D), Soprocare photo camera®, teledentistry consultations, and clinical photographs by dentists, specialists and health professionals such as nurses and nutritionists. Similarly, one study identified knowledge and beliefs about teledentistry from college in students and dental professionals, and six studies assessed the applicability and use of teledentistry for health promotion and disease prevention during consultation, through questionnaires, interviews and databases in children, mothers and other adults.
Results of intervention studies
One quasi-experimental study was found, which evaluated and compared the visual and infrared detection methods to identify early non-cavitated ex vivo demineralization through three tests to detect occlusal demineralization: Midwest Caries ID™ (MID), visual photographic examination (CAM), and cross-polarization optical coherence tomography (CP-OCT) on teeth removed 1 to 2 weeks apart. The teeth were then sectioned, and each lesion’s depth was confirmed, reporting that MID and CP-OCT were helpful in detecting the presence of demineralization, though not in the depth of the injury. It also did not present diagnostic values such as CAM for use in teledentistry.
Bias risk analysis
Of the included studies, 95% had moderate to high bias risk. Table 2 shows the bias risk analysis for observational studies only. On the other hand, the only intervention study was considered to have low bias risk as shown in Table 3.
Table 2 Quality assessment according to the Agency for Healthcare Research and Quality (AHRQ)
| Author | Source of information (survey, records, review) | Inclusion and exclusion criteria | Time period evaluated | Consecutive population | Reports other aspects of participants | Quality assessment | Exclusions of participants in the analysis | Assessment and control of confounding variables | Data collection response rate | Handling missing data in the analysis | Clarity in follow-up |
| Purohit, et al (2017) | + | + | + | + | - | - | - | - | + | - | N/A |
| Estai, et al (2015) | + | - | - | + | - | - | - | - | + | - | N/A |
| Roxo, et al (2017) | + | + | + | + | - | - | - | - | + | - | N/A |
| Paixao, et al (2018) | + | + | + | + | - | - | + | - | + | - | N/A |
| Vinayagamoorthy, et al (2019) | + | + | + | + | - | - | - | - | + | - | N/A |
| Giraudeau, et al (2017) | + | + | + | + | + | - | - | - | + | - | N/A |
| Boringi, et al (2015) | + | - | - | + | + | - | - | - | + | - | N/A |
| Estai, et al (2016) | + | - | - | + | + | - | - | - | + | - | N/A |
| Skandarajah, et al (2017) | + | - | - | + | + | - | - | - | + | - | N/A |
| McLaren, et al (2016) | + | + | + | + | + | - | - | - | + | - | N/A |
| Kohara, et al (2018) | + | + | + | + | + | - | - | - | + | - | N/A |
| Bhatts, et al (2018) | + | + | + | + | + | - | - | - | + | - | + |
| Daniel, et al (2017) | + | + | + | + | - | - | - | - | + | - | N/A |
| Martin, et al (2016) | + | + | + | + | + | - | - | - | + | - | N/A |
| Jung, et al (2018) | + | + | + | + | - | - | - | - | + | - | N/A |
| Haron, et al (2017) | + | - | - | + | - | - | - | - | + | - | N/A |
| McLaren, et al (2017) | + | - | + | + | - | - | - | - | + | - | N/A |
| de Almeida, et al (2017) | + | - | + | + | - | - | - | - | + | - | N/A |
| Birur, et al (2019) | + | + | + | + | - | - | - | - | + | - | N/A |
| Alklaybsa, et al (2017) | + | + | + | + | - | - | - | - | + | - | N/A |
| Estai, et al (2016) | + | + | + | + | - | - | - | - | + | - | N/A |
| Morosini, et al (2014) | + | + | + | + | - | - | - | - | + | - | N/A |
| McFarland, et al (2017) | + | + | - | + | - | - | - | - | + | - | N/A |
+ Yes: Meets the assigned item - No: Does not meet the assigned item N/A: Not applicable
Source: by the authors
Table 3 Quality assessment according to Cochrane Collaboration
| Author | Random sequence generation | Concealing the assignment | Blinding participants and staff | Incomplete results data | Selective reports | Other bias |
|---|---|---|---|---|---|---|
| Van Hielsen, et al (2013) | + | + | + | + | - | N/A |
+ Yes: Meets the assigned item - No: Does not meet the assigned item N/A: Not applicable
Source: by the authors
DISCUSSION
The concept of teledentistry includes the combination of the use of computers, telecommunications technology, digital diagnostic imaging services, devices and software for oral health analysis and monitoring, through diagnosis and treatment recommendations in the distance.42 All the aforementioned aids have been used in fields such as care, education, and public health due to easy access to remote areas, and reduced time and costs for patients.43
Two teledentistry methods are practiced nowadays: store and transmit and/ or videoconferencing. However, its implementation is minimal, and a more frequent use of this modality in the diagnosis of pathological conditions is suggested.44
Pentapati et al evaluated the reliability of an intraoral camera in teledentistry for the detection of oral diseases through an examiner who was trained and calibrated in an intraoral camera to take videos of the oral cavity, against clinical examination to evaluate cavities, bacterial plaque, calculus, dental wear, and fluorosis in children, reporting significantly higher values with the use of the intraoral camera than with clinical examination (p = 0.001), by means of the Spearman correlation coefficient.45
Similarly, Purohit et al evaluated the reliability of videography to detect tooth decay among 12-year-old schoolchildren in a rural Indian region through clinical examinations using the decayed, missing and filled teeth index (DMF-t) and a standardized video recording of the oral cavity. Sensitivity (0.86) and specificity (0.58) values were calculated for videographic evaluation of tooth decay, and concordance was evaluated using the Bland- Altman graph, concluding that teledentistry can be used as an alternative for dental cavity detection and for consultations in remote or hard-to-reach areas.37
Torres-Pereira et al evaluated the applicability of telediagnosis in oral medicine through the transmission of clinical images by email to two specialists, using two clinical hypotheses for each case, which were compared with the biopsy results, showing that in 80% of cases at least one specialist provided the correct diagnosis, showing that the use of information technology provides an acceptable rate of correct diagnoses, thus supporting its application as a tool for detecting oral diseases.46
Regarding users’ satisfaction with the use of applications and mobile devices in teledentistry, Estai et al evaluated users’ acceptance of a teledentistry model using Remote-I, a store and transmit telemedicine platform, to assist in the detection of oral diseases transmitted directly from the application to the server, finding out that users showed optimism towards the use of the teledentistry system, and positively evaluated the items in terms of content and quality of service.24
However, to achieve efficiency and quality standards in teledentistry, it is necessary to adequately train professionals and insist in instant response to avoid careless service, educating dentists in the practice of teledentistry, including information on legal, ethical and technological implications, as well as clinical methods for patient care.
The findings of this systematic review show that, while the use of teledentistry is recent, there are some studies evaluating the knowledge, perceptions, and attitudes in teledentistry among dental students, general dentists and specialists, as well as the use of applications, mobile devices and intraoral cameras for oral health education and diagnosis of oral diseases such as tooth decay, periodontitis, and oral cancer, as well as the adherence to recommendations provided by dentists. This provides an important source of information and advice for health policy makers, service managers and clinicians, resulting in increased access to health services and dental consultation.47
Most evaluated studies have multiple limitations, and even though this review was limited to the use of teledentistry in recent years, there appears to be scarce use of this technology. This review found out that there are only a few studies that help identify good quality standards, since most studies did not show prior evaluations, and there was only one experimental study, showing that the degree of scientific evidence is currently poor.
Similarly, while teledentistry has a high potential for addressing needs in the rural population or in remote areas, the findings of this review show that more than half of the evaluated studies were performed in urban areas rather than rural environments, or did not report the location where they were conducted, and most studies were developed in the U.S., Europe, Asia and Australia. This may be due to economic factors (financing), poor access to networking in rural areas, or because the studies are in their pilot stage; it is therefore necessary to conduct further studies with a significant sample and related follow-up studies in Latin American countries.
CONCLUSION
This review helped determine the impact of teledentistry in different dental areas. However, most revised studies showed limitations in terms of short-term use of teledentistry and low level of evidence due to the methods and results obtained. It is therefore necessary to conduct further studies to evaluate the efficacy and follow-up of teledentistry services for consultation, diagnosis, and recommendations in dental treatment, as it may be a viable alternative in the reduction of time, transfers, and costs.