Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Vitae
Print version ISSN 0121-4004
Vitae vol.21 no.1 Medellín Jan./Apr. 2014
LETTERS TO THE EDITOR
DRUG INTERACTIONS AND POSSIBLE SEROTONIN SYNDROME IN A PATIENT WITH FIBROMYALGIA
INTERACCIONES MEDICAMENTOSAS Y POSIBLE SÍNDROME SEROTONINÉRGICO EN UN PACIENTE CON FIBROMIALGIA
Patricia de Carvalho Mastroianni, PhD.1, Fabiana Rossi Varallo, PhD.2, Manuel Machuca, PhD in Pharmacy3
1 Assistant Doctor Professor at the Department of Drugs and Medications at the School of Pharmaceutical Sciences of the Universidade Estadual Paulista Júlio de Mesquita Filho – UNESP (Araraquara, SP , Brazil).
2 student at the Department of Drugs and Medications at the School of Pharmaceutical Sciences of the Universidade Estadual Paulista Júlio de Mesquita Filho – UNESP (Araraquara, SP , Brazil).
3 Clinical Pharmacist. Unit of Optimization of the pharmacotherapy. Sevilla-Spain
* Autor a quien se debe dirigir la correspondencia: patriciamastroianni@yahoo.com.br.
Recibido: 16 November 2013
Aceptado: 02 February 2014
DEAR EDITOR
Depression associated with fibromyalgia can be treated with selective serotonin reuptake inhibitors (SSRI) as fluoxetine, paroxetine or citalopram; or with serotonin–norepinephrine reuptake inhibitors (duloxetine or milnacipran) (1, 2). In patients with fibromyalgia, several meta-analyses have demonstrated the effectiveness of antidepressants, particularly the tricyclic antidepressant (TCA) amitriptyline, which reduce the pain, fatigue, depression, and sleep disturbances. Additionally, tramadol, pregabalin, and gabapentin are other treatment options.
Bruxism is a rare secondary effect related to drugs with potent serotonergic activity. However, the use of TCAs, SSRIs, and opioid analgesics have been associated to serotonergic syndrome (3, 4). The incidence of serotonergic syndrome is about 17% in patients with migraine, depression, anxiety and panic disorder (5); nevertheless, the incidence is still unknown in patients with fibromyalgia. The serotonergic syndrome is characterized by signs and symptoms of agitation, tachycardia, increased tension, tremor, fever, dyspnea, diarrhea, mental confusion, and insomnia (3-5). In this context, we report a possible drug-induced bruxism in a patient with fibromyalgia associated with depression.
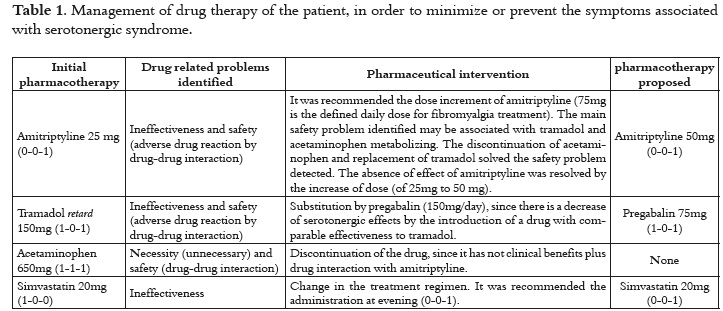
A complete and integral pharmacotherapy assessment of a 46 years old Caucasian woman diagnosed with fibromyalgia associated with depression was performed according with the Strand et al (2004) proposals (6). The medications used by the patient were: amitriptyline 25mg, (0-0-1); tramadol retard 150mg (1-0-1); acetaminophen 650mg (1-1-1); simvastatin 20mg, (1-0-0), and esomeprazole 20 mg, (1- 0-0). After six months of the treatment initiation, she reported gnashing of her teeth. The patient's drug related needs were comprehensively assessed and, once the problems were detected, a report was sent to her physician to propose changes in the pharmacotherapy, in order to minimize the negative clinical outcome (bruxism) experienced by the patient (table 1).
An unsatisfied pharmacotherapeutic problem of necessity was noted, since the patient had complained of pain that she tried to solve with the increase of acetaminophen dose. In order to understand and quantify her pain perception, an analgesic ladder of zero to ten was developed (zero intolerable pain and ten without pain). Patient reported pain perception between two-three. So, a potential drug-drug pharmacodynamic and pharmacokinetic interaction was identified among tramadol, acetaminophen and amitriptyline, which may be associated with the development of serotonergic syndrome. Thus, we proposed to the physician the discontinuation of acetaminophen and the replacement of tramadol by pregabalin (150mg/day) (table 1).
Patient's physician accepted the management of pharmacotherapy proposal. In the following days after suspension of acetaminophen, and the replacement of tramadol by pregabalin, the negative outcome was resolved. Regarding the pain treatment, the patient classified the symptom between seven-eight, according to analgesic ladder.
Data suggest that the patient experienced a serotonergic syndrome, since after the proposed pharmaceutical intervention the signs and symptoms reported by patient disappeared. The identification of serotonergic syndrome is primarily based on exclusion, and strong suspicion based on a patient´s current drug therapy.
Amitriptyline and tramadol are drugs with serotonergic action, which inhibit the reuptake of serotonin and noradrenalin. In addition, the main metabolic pathway of tramadol is through the CYP 2D6 enzymes, which may be partially inhibited by amitriptyline. Consequently, the tricyclic antidepressant may inhibit the metabolism of tramadol, interaction that can be a significant factor contributing to serotonin syndrome (7). Moreover, amitriptyline and acetaminophen compete for hepatic conjugation with glucuronic acid and sulfuric acid, delaying its elimination. Furthermore, the interruption of acetaminophen promotes the cessation of pharmacokinetic interaction.
A possible pharmacodynamic and pharmacokinetic interaction between amitriptyline, tramadol and acetaminophen may explain the bruxism as a clinical manifestation of serotonergic syndrome. The negative outcome was treated by the replacement of tramadol by pregabalin and by the discontinuation of acetaminophen.
REFERENCIAS BIBLIOGRÁFICAS
1. G oldenberg DL. Pharmacological treatment of fibromyalgia and other chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007; 21: 499–511. [ Links ]
2. M iquel CA , Campayo JG, Fórez MT , et al. Documento de Consenso interdisciplinar para el tratamiento de la fribiomialgia. Acta Esp psiquiatr. 2010; 38 (2): 108-120. [ Links ]
3. C hu J, Wang RY , Hill NS . Update in clinical toxicology. Am J Respir Crit Care Med. 2002; 166 (1): 9-15. [ Links ]
4. Jackson N, Doherty J, Coulter S. Neropsychiatric complications of commonly used palliative care drugs. Postgrad Med J. 2008; 84 (989): 121-126. [ Links ]
5. S chuman E. Serotonin toxicity revisited. Headache 2009; 49 (5): 784-785. [ Links ]
6. S trand LM , Cipolle RJ, Morley PC , Frakes MJ. The impact of pharmaceutical care practice on the practitioner and the patient in the ambulatory practice setting: twenty- five years of experience. Curr Pharm Des, 2004; 10 (31): 3987-4001. [ Links ]
7. N elson EM , Philbrick AM . Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother 2012; 46: 1712-6. [ Links ]