Pharmacist-led patient education on antiretroviral therapy: is it enough to improve adherence?*
The Acquired Immunodeficiency Syndrome (AIDS) became a manageable disease after effective control of HIV replication through antiretroviral therapy (ART).
The problem to be faced now is non-compliance to ART, which can be associated mostly to adverse effects, complexity of pharmacotherapy and lack of knowledge about the disease and the medication1.
A pharmacotherapeutic follow-up was conducted with a 58-year-old man with HIV under ART for 12 years, and non-compliance to ART. He had a medical history of partial blindness due to ocular Herpes Zoster, and hospitalizations due to pneumonia.
Six meetings were realized within seven months. The first one consisted of anamnesis and consultation of medical record to verify drug dispensing data, and clinical and laboratory characteristics. Instruments to evaluate adherence, compliance and quality of life were also applied (Table 1), and the patient was classified as non-compliant according to the instrument SMAQ3 by frequently forgetting to take the medication and to administrate it improperly.
The main complaints related to the ART were headache, difficulty to swallow the medication and gastrointestinal discomfort.
A care plan was proposed, targeting to solve problems related to the therapy, and to improve the knowledge regarding the disease and the therapy itself through educational interventions.
After the second meeting changes were made to the therapy, aiming to improve effectiveness and eliminate gastrointestinal discomfort. A daily medication diary was proposed according to the patient's routine to help and incentive the intake of medicines. It reinforced posology and drug information and was monitored till the end of the intervention.
Table 1 Characteristics of lifestyle, clinical records, quality of life, adherence and posology
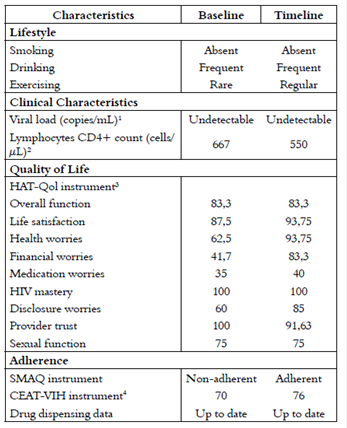
1Viral load is considered undetectable when there is <50 copies of virus/mL of blood
2The disease is considered controlled when CD4+ cell count is >350 cells/μL
3Dimensions accessed by HAT-Qol. Linear 0-to-100 scale, where 0 is the worst score possible and 100 is the best score possible
4Linear 17-to-89 scale, where 17 is the worst score possible and 89 is the best score possible
During the educational interventions, the patient reported having none previous understanding of the benefits and risks of the therapy and the importance of adherence. This misunderstanding used to lead him to take all the medication together during weekends, and to take it daily without scheduling.
On the last meeting the same instruments and parameters of the first were verified, as well as intervention feedback. The patient reported that the acquired knowledge during the interventions helped him to understand the disease, the importance and mechanism of medication and the need to be compliant. He also correlated the improvement on his quality of life to the interventions.
The patient was classified as compliant on the last evaluation of SMAQ2 and enhanced a higher score on CEAT-VIH3, which evaluates adherence. The score of the HAT-Qol4 instrument also had positive changes, especially on the dimension “Health Worries”, what evidences that the interventions had a positive impact on quality of life (Table 1).
He changed the medicines administrations as recommended, but continued with the problems to swallow the medication and gastrointestinal discomfort.
The patient was receiving six different drugs, including three protease inhibitors (PI) (Table 2), which are known for causing gastrointestinal toxicity. In this way the gastrointestinal discomfort might had been related not only to adverse effects of medication but also to daily pill burden1. Elimination of some drugs could have solved it and also eliminated omeprazole, which was being used for gastrointestinal protection.
Recommendations were done to the medical team during the follow up, but due to the history of poor compliance and serious history of opportunistic disease and uncontrolled AIDS, no drugs were switched over. A study conducted by Kelly DV et al (2013) showed that physicians believed that the most important pharmacist function was to help improving patient adherence, but rated functions in which the pharmacist made recommendations to physicians regarding modification of a patient's drug therapy as least important. This shows that sometimes physicians do not see how the pharmacists could work and how advantageous this cooperation could be, as improvement in adherence is highly related to modifications on pharmacotherapy5. Although individual interventions can positively impact on adherence, simplification of drug treatments among all strategies has probably the greatest impact6.
Table 2 Pharmacotherapy
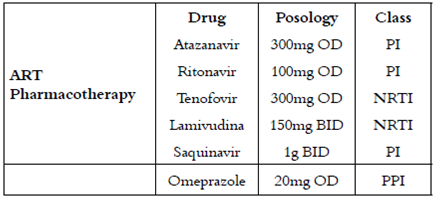
PI: protease inhibitor, NRTI: nucleoside reverse transcriptase inhibitor, PPI: proton pump inhibitor
One possible reason for the medical team refusal for drug replacement is that the patient was receiving double-boosted PI regimen (ritonavir, saquinavir and atazanavir), which have a high degree of antiviral efficacy and biodisponibility. Their effective viral suppression discourages the development of resistance with occasional missed doses, making them the most forgiving regimen7.This would explain why he had already satisfactory levels of CD4+ count and HIV viral load, and therefore the achieved global health improvement did not transform into measurably better immunological and virological outcomes.
Also, it has been shown that antiretroviral drug resistance might not be a major determinant of clinical disease progression8, so it could have been better to keep hold to a partial compliant efficient regimen than risking switching it.
Although the pharmacotherapeutic follow up improved self-care and awareness regarding the therapy, interventions seeking to simplify ART and strengthen cooperation between pharmacists and physicians might have a better impact on adherence, especially on symptomatic patient.














