At the global level, there are many challenges and opportunities for pharmaceutical personnel (professionals, technologists and technicians), mainly for those working at the outpatient pharmacies (Pharmaceutical Retail Establishments, in the context of the Colombian health system). Overall, Colombian outpatient pharmacies have limited their activities to selling medicines, while the World Health Organization (WHO) and the International Pharmaceutical Federation (FIP) have promoted their evolution toward a more patient-oriented practice. This focusing ranges from the procurement and supplying of medicines to pharmaceutical care services, oriented to ensure the best treatment for patients. Therefore, outpatient pharmacies play an important role in the improvement of pharmacotherapy and patient outcomes, promoting rational use of medicines and reducing healthcare costs 1. This kind of results have been gradually demonstrated in other countries 2. In that way, in Colombia there is a considerable need to create outpatient pharmacies which allow us improve outcomes for patients care, increase access to healthcare system care (specially for vulnerable populations) and, to provide specific-medication tools for reach successful therapies. By including patient education, it is possible to ensure the best health outcomes, to improve patient satisfaction and to enhance cost‐effectiveness relationship.
The process of using outpatient drugs involves an interaction between the patient, the doctor and the pharmacist. There is evidence that greater collaborative between the health care professionals can improve patient care. Joint training and collaborative networking should encourage increased integration, which has gradually been strengthened in an increasing digital world, mainly with the incorporation of Information and Communication Technologies (ICT) and initiatives such as Health 2.0 3. This promotes the emerging of new Information Systems (IS), more accurate, user friendly, agile, simple and practical to use. At the same time, it would build more possibilities for communication, that can be used to incentivize a relationship between health professionals and patients. In addition, the pharmaceutical personnel needs training in the ICT integration as a tool for the outpatient pharmacies and health care communication networks.
The main objective of pharmaceutical care is to identify, prevent and resolve all deviations that cause unfulfillment of therapeutic purpose. It also evaluates health problems, taking into account the need, effectiveness and safety of medicines 4. In consequence, the pharmaceutical care should include activities such as pharmacotherapeutic follow-up, dispensing, patient education and counseling 5; all contribut to get the best health outcomes for the patients. Additionally, pharmacists have expertise (knowledge, skills, and practices) in the safe and effective use of medicines, which are needed to provide an improved service 6, promote a rational use of drugs and improve communication with the patient and therapeutic adherence. Finally, these strategies optimize pharmacotherapy and prevents adverse events. However, these competencies are not enough, particularly when there is a lack of training in different areas of undergraduate courses 7. Hence, continuing education programs can play a vital role in the growth of pharmaceutical education and in the strengthening of these competencies. Some countries are implementing this kind of educative programs for outpatient pharmacists as obligatory and lifelong learning programs to improve pharmacy care services 8.
Worldwide, there is evidence that demonstrate the effectiveness and relevance of pharmaceutical interventions, all focused on the combination of ICT, continuing education programs, and network support between outpatient pharmacists and other health professionals. For example, the use of protocols and electronic information systems in the setting prescribing and dispensing, additionally with courses on-line dispensing by pharmacists 9. Another intervention evaluated the impact of a prescriber focused on individualized patient education and information in dispensing to reduce the meperidine use. The intervention was associated with a statistically significant reduction in meperidine use, the monthly number of patients declined by 12%, prescriptions by 10% and number of tablets dispensed by 13% 10. In the same way, those electronic information systems are used for opioid prescribing and pain management, which process contributed the determination of the appropriate intervals between clinic visits by stratifying patients (11).
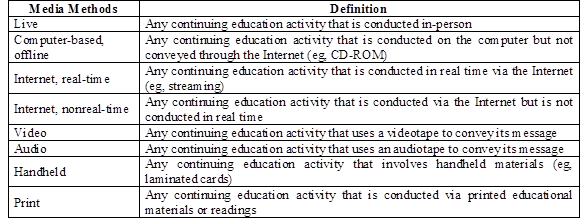
A systematic review summarized the effects of the media methods that were used. This shows their impact in continuing education programs that provide outpatients pharmacy services and methods to evaluate the effectiveness of these programs (Table 1). According to this review, that included 19 articles mainly conducted by developed countries, only 2 studies found that the continuing education program was ineffective or partially effective. However, most studies used non-robust, non-validated, and non-standardized methods to measure the effectiveness of the interventions. Most studies were oriented to the effect of continuing education programs in modifying the understanding and skills of pharmacists, and only one study evaluated the benefits of the program for patients or customers. The authors concluded that there is not enough evidence to support which media methods are the most effective and that it is needed to intervene with robust, standardized and validated methods 8. Then, some challenges are still dormant, among them there are programs of continuing education, evaluation and continued implementation, which have innovative approaches supported by ICT and that are oriented at the outpatient pharmacies in the Colombian context with the purpose of achieve an interdisciplinary work.
Pharmaceutical personnel have the competencies required to contribute to the quality in the use of drugs, to minimize medication errors and to help outpatients to have a better manage of their medicines. Continuing education, communication and relationships are the keys to improve collaboration and, consequently, to achieve optimal medication management. Although much remains to be investigated on this issue, now there exist more opportunities and training. Continuing education, outpatient pharmacy, care processes and services will consolidate pharmacists within the health systems. These tools according to their knowledge and the availability of the resources, will allow them to collaborate with other professionals to support the patients in the most appropriate way. On the other hand, the supplying of high-quality and affordable healthcare services are increasingly difficult challenges, probably, due to the complexities of healthcare services and systems and because of the lack of knowledge of facilitators for the implementation of diverse pharmaceutical interventions in the context of Primary Health Care