Introduction
Iodine is an essential micronutrient for human development, and its main function is to participate in the synthesis of thyroid hormones T3 and T4. The deficiency of this nutrient is associated with a low intake of foods containing iodine, such as fish, seafood, and iodized salt, which is the primary source to obtain this mineral (1,2). The World Health Organization (WHO) and the United Nations International Children's Emergency Fund (UNICEF) have been encouraging the policy of using iodinated salt around the world (3). In Brazil, salt iodination has been mandatory since the 1950s (4).
Despite the current policies, iodine deficiency is still a global public health problem. It is estimated that around 13% of the global population has been affected by diseases related to this micronutrient deficiency (5). Studies suggest that pregnant women are more prone to iodine deficiency, as their needs increase by more than 50% during pregnancy for developing the fetus, especially in the first trimester (6). Besides, a study conducted in Europe found that pregnant women from two-thirds of European countries were deficient in iodine (7). In this context, maternal iodine deficiency can lead to irreversible neurological diseases, mental retardation, and a lower intelligence quotient of the child, and increase the risk of miscarriage, pregnancy complications, infertility, hypothyroidism, endemic goiter, and cretinism (8-11).
To date, little is known regarding the prevalence of iodine deficiency in Brazil in women of childbearing age, and high heterogeneity has been suggested. A systematic review, published in 2015, identified only two studies in women of childbearing age with controversial results on the adequacy of excreted iodine levels (12). Prevalence studies are relevant because they reflect disease burden in society, supporting the definition of priorities for health policies or assessment of interventions. In health technology assessment, prevalence data could be used to estimate costs and make assumptions in decision-analytic models (13).
Regarding the prevalence, cross-sectional studies using probabilistic random samples conducted in the relevant geographical setting are the most appropriate study design. However, when performing such primary studies are not feasible, a systematic review of the existing available data may be the most appropriate approach to provide at least some indication of the probable magnitude of the problem and to achieve greater national representativeness (14). Therefore, this study estimates the prevalence of iodine deficiency and associated factors in women of childbearing age in Brazil.
Material and methods
This systematic review was performed following Meta-analysis Of Observational Studies in Epidemiology (MOOSE) (15) and Joanna Briggs Institute (16) recommendations; it was also reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (17). The protocol is available at OSF (18) and PROSPERO (CRD42020221605). This study is part of a larger study that evaluated deficiencies of vitamins A, B, C, D, and E, as well as calcium, iodine, iron, and zinc in women of childbearing age in Brazil.
Electronic searches were conducted in PubMed, LILACS, WHO, Capes' dissertations and theses (gray literature), and Scopus databases, including EMBASE, Medline, open access sources, scientific websites, and gray literature (19), from the inception date to May 2020. Additionally, reference lists of reviews and included studies were also searched. Complete search strategies are provided in the protocol (18).
Studies that fitted the following inclusion criteria according to the CoCoPop acronym were included: i) Condition: iodine deficiency; ii) Context: Brazil without the restriction of setting; iii) Population: women of childbearing age (15 to 49 years old), without restriction to diseases or status (e.g., non-pregnant, pregnant, and lactating). It is important to emphasize that predefined parameters to describe the condition and population were considered in this review. However, we included and analyzed subgroups of studies that reported the deficiencies of interest with different classifications (e.g., women aged 15 to 44 or pregnant teenagers) or other laboratory parameters.
In addition to the CoCoPop acronym, restrictions on study design were considered. Although cross-sectional studies correspond to the ideal and most common study design for reporting prevalence, several studies can report this variable, such as national surveys or longitudinal studies. Thus, all types of studies were included, except for reviews, letters, comments, reports, and case series. No language restriction was applied.
Two researchers independently screened the titles and abstracts of the retrieved studies, and in the second stage, full-text articles to identify relevant records. Discrepancies were solved in consensus meetings using another researcher as a referee. Finally, the selection process was conducting using spreadsheets.
Five researchers independently extracted the following data:
Study characteristics (type of study, analysis period, federative unit, characteristic of population (e.g., pregnant women), micronutrient deficiency, method of measurement and assessment, sampling, and funding;
Participant’s characteristics (ethnicity, comorbidities, medications or supplement, body mass index (BMI), age, education, per capita income);
Prevalence estimate (n / N (%)) to total population and subgroups.
Although the cut-off for assessing iodine deficiency was not considered an inclusion criterion in the current review, only studies evaluating similar cut-offs were grouped. Thus, for pregnant and lactating or non-pregnant women, the deficiency was considered when the median urinary iodine was lower than 150 and 100 μg/L of urinary iodine concentration (UIC), respectively (20).
The synthesis of the data was primarily done by meta-analysis. Transitivity assessment was performed by comparing the CoCoPop acronym for each study (population inclusion and exclusion criteria and subpopulation definitions). After identifying the important discrepancies, sensitivity analyses excluding the study in question were performed.
The data collected were transferred and analyzed separately in the software R v. 3.6.3 / R studio 1.2.5033 (21) to perform direct meta-analyses using the READR (22) and META packages (23). Direct proportion meta-analyzes were conducted using the inverse variance (base case) and GLMM (sensitivity analysis) methods (23). Additionally, Freeman-Tukey Double arcsine (PFT) (base case) and Logit (PLOGIT) transformation were considered (sensitivity analysis) in the fixed effects (base case) and random effects (sensitivity analysis) model (17,23) to calculate the weighted summary proportion. Although high heterogeneity was expected and, therefore, a random-effects model is recommended, a fixed-effects model could be preferred in prevalence meta-analyses; otherwise, the weighting will not consider the weight of the studies (24). Thus, analyzes were conducted by the two models, with potential differences being discussed. The meta-analysis result was given by the proportion combined with 95% CI and the list of proportions (expressed as a percentage). Their respective 95% CI was found in the individual studies included in the meta-analysis. Additionally, a Higgins inconsistency test (I2) with an estimator for tau2 was considered using the DerSimonian-Laird method (base case) and statistical adjustment by Hartung and Knapp to random model (sensitivity analysis).
A cumulative meta-analysis was performed to assess changes and trends over time and highlight emerging or decreasing conditions and their potential relationship with implemented public policies.
Sensitivity analyses were performed by the leave-one-out method. Subgroup and meta-regression analyses, considering the period of analysis, state, and region of Brazil, comorbidities, age, or status (not pregnant, pregnant, lactating), were planned to meta-analyses with at least ten studies. Alternative statistical methods were also used to validate the conclusions. The probability of publication bias would be assessed using rank tests (base case), linear regression, or method of moments (sensitivity analysis), with at least 10 studies by meta-analysis (23).
The JBI Assessment Checklist for studies reporting prevalence data (14) was used to assess the methodological and reporting quality of the studies included. This tool is considered with the greatest methodological rigor and completeness in most critical domains (25). It is also used in the absence of a valid tool for assessing the risk of bias in prevalence studies. The evaluation was done by two reviewers independently. In the absence of consensus, points of disagreement were resolved by the opinion of another investigator.
Data sharing and data accessibility
The data supporting this study’s findings are openly available in OSF at http:doi.org/10.17605/OSF.IO/J9QMH (18).
Results
Our systematic review identified seven studies on iodine deficiency (eight records, since one study was published twice) (S1 Figure and S2 Table are openly available in OSF repository(18)), comprising six cross-sectional studies and one prospective cohort (Table 1).
The studies were conducted between 2002 and 2017, in cities in the Southeast (n = 5), South (n = 1), and Northeast (n = 1) regions with women selected from obstetrical care (n = 4) or outpatient services (n = 3). Most studies did not report the sampling way (n = 5); however, it was identified or inferred that all studies used convenience sampling. All studies received some funding (Table 1).
Table 1 Description of the characteristics of the studies (n = 07) and participants included (n = 1,354), 2020.
| Study | Study design | Inclusion period | Federative unit/Region | Setting | Funding | Characteristic / N | Comorbidities | BMI, kg/m2 (SD) | Mean age, years (±SD) |
|---|---|---|---|---|---|---|---|---|---|
| Morais 2020 (26) and Corcino 2019 (27) | PC | 2014-2017 | RJ / Southeast | Obstetrical care | FAPERJ; CNPq | Pregnant (1st and 3rd trimesters) / 196 | DM, HDP, TH | 24.5 (7.0) or 25.0 (6.6) | 27.0 (9.0) or 26.5 (4.9) |
| Souza 2020 (28) | CS | 2015-2016 | BA / Northeast | Obstetrical care | State of Bahia Research Foundation | High risk pregnancy / 241 | DM, HDP, Cardiac disease | Not reported / Most of women: BMI adequate | 28.6 (7.2) |
| Saraiva 2018 (29) | CS | 2014-2017 | RJ / Southeast | Obstetrical care | FAPERJ; CNPq | Pregnant / 244 | Not reported | 24.9 (6.4) | 26.5 (5.0) |
| Mioto 2018 (30) | CS | 2012-2016 | SP / Southeast | Obstetrical care | FAPESP; CAPES | Pregnant / 273 | None | 26.2 (4.9) | 28.1 (6.5) |
| Ferreira 2014 (31) | CS | 2008-2009 | SP / Southeast | Outpatient | FAPESP | Pregnant and non-pregnant / 191 | Autoimmune diseases and mild goiter | Not reported | Pregnant: 25.7 (5.6); Non-pregnant: 28.5 (5.0) |
| Marino 2009 (32) | CS | 2002-2003 | SP / Southeast | Outpatient | FAPESP | Autoimmune thyropathies / 4 | Not reported | Not reported | 32.3 (2.3) |
| Soares 2008 (33) | CS | NR | RS / South | Outpatient | Incentive Fund to Research and Events of the Hospital de Clínicas de Porto Alegre, RS; CAPES | Pregnant / 147 | Not reported | 27.5 (5.3) | 26.8 (6.4) |
BA: Bahia, BMI: body mass index, CAPES: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, CNPq: Conselho Nacional de Desenvolvimento Científico e Tecnológico, CS: cross-sectional; DM: diabetes mellitus, FAPERJ: Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro, FAPESP: Fundação de Amparo à Pesquisa do Estado de São Paulo, HDP: hypertensive disorders of pregnancy, NA: not applicable, PC: prospective cohort, RJ: Rio de Janeiro, RS: Rio Grande do Sul, SD: standard deviation, SP: São Paulo, TH: thyroid disorders.
In total, 1,354 participants were included, mainly pregnant women (n=1,292), with normal body mass index and with a mean age between 25.7 and 32.3 years old. No study reported prevalence in lactating women. Some comorbidities reported were diabetes mellitus, hypertension, mild goiter, and autoimmune thyropathies. The presence or absence of medication use was not reported in any included studies; however, Ferreira et al. (31), Morais et al. (26), and Souza et al. (28) reported the use of a nutritional supplement, regardless of the presence of iodine. In Mioto et al. (30), all participants did not use a nutritional supplement.
Ethnicity, education, and income per capita were not reported by most studies, except Souza et al. (28), who said most of the participants had high school (55.4% to 62.2%) and one to two minimum salaries per capita (54.4% to 73.9%) (Table 1).
The detailed methodological quality of the studies is presented in Table 2. All studies have at least one ‘No’ answer, which suggests a poor reporting or methodological quality.
The main questions with “No” answers were about “sampling way” since most studies used convenience samples. “Description of subjects and setting” due to the absence of a report of ethnicity, medicine use, nutritional supplement use, comorbidities, BMI, educational level, or per capita income of the participants. “Appropriate statistical analysis”, once most studies did not report the number of participants with events or total number observed (only prevalence in percentage). And “response rate” due to inappropriate sample size. The questions with “Yes” answers were about sample frame, appropriate coverage, and valid methods used to identify the nutritional deficiencies.
Table 2 Methodological quality assessment, considering Joanna Briggs Institute tool to prevalence studies.
| Studies | |||||||
| Questions | Morais 2020 (26) and Corcino 2019 (27) | Souza 2020 (28) | Saraiva 2018 (29) | Mioto 2018 (30) | Ferreira 2014 (31) | Marino 2009 (32) | Soares 2008 (33) |
| 1 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2 | No a | Unclear b | No a | No a | No a | No a | Yes c |
| 3 | No d | No d | Unclear e | Unclear e | Unclear e | Unclear e | Unclear e |
| 4 | No f | Yes | No f | No f | No f | No f | No f |
| 5 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7 | NA g | NA g | NA g | NA g | NA g | NA g | NA g |
| 8 | No h | No h | No h | No h | No h | Yes | Yes |
| 9 | No i | No i | No i | No i | No i | No i | No i |
1.Was the sample frame appropriate to address the target population? 2.Were study participants recruited in an appropriate way? 3.Was the sample size adequate? 4.Were the study subjects and setting described in detail? 5.Was data analysis conducted with sufficient coverage of the identified sample? 6.Were valid methods used for the identification of the condition? 7.Was the condition measured in a standard, reliable way for all participants? 8.Was there appropriate statistical analysis? 9.Was the response rate adequate, and if not, was the low response rate managed appropriately?
NA: not applicable; a - Not reported, convenience sampling was considered; b - Cluster sampling, but it is not reported if random or convenience; c - Reported convenience sampling; d - Morais et al. and Souza et al. estimated a target sample of, respectively, 276 and 203 participants, whereas in the current review it was estimated 369 to a prevalence of 40%; e - A target sample size was not reported; f - Most of studies did not reported ethnicity, medicine use, nutritional supplement use, comorbidities, body mass index, educational level and / or income per capita; g - Not applicable, since the methods is automated highly replicable; h - Not reported numerator (n) or denominator (N) of prevalence; i - All studies presented a response rate below 369 participants to pregnant women and 174 to non-pregnant women.
The prevalence of iodine deficiency was reported to total participants and some subgroup analyses and ranged from 16% to 62%. The subgroup analysis considered the following conditions, different gestational trimester (28,30), UIC cut-off (28,29,31), age range, parity, BMI, hypertension, diabetes mellitus, urban or rural areas, income in minimum salaries, the number of people in the household, education level, type of house, iodized salt intake, consumption and storage of table salt, salt storage areas nearby cooker, use of industrial seasoning, use of a nutritional supplement, cassava intake, and salt-restricted diet (28).
Statistical difference (p < 0,05) in the prevalence of iodine deficiency between these subgroups was identified only for hypertension (Yes: 61%; No 39%) and salt-restricted diet (Yes: 56%; No: 44%) (28). No meta-analysis for these subgroups was possible since most of them were reported in the same study (28), or when two or three studies reported the same subgroup, a different UIC cut-off was considered (28-31).
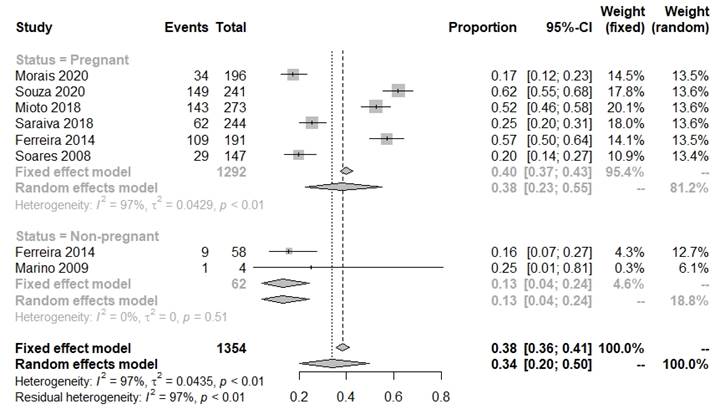
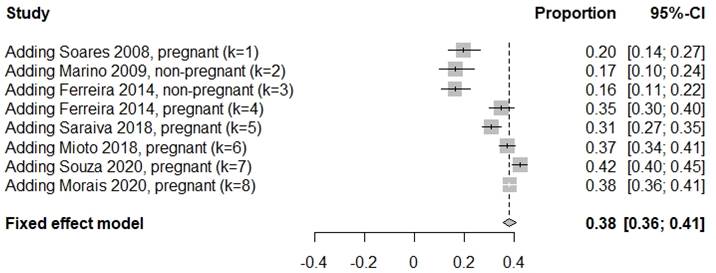
In the meta-analysis for the base case, an overall prevalence of 38% (95% CI 36%-41%) was identified, 40% (95% CI 37%-43%) for pregnant women and 13% (95% CI 4%-24%) for non-pregnant women (Figure 1). The cumulative meta-analysis considering the year of publication, showed an increasing trend, with recent studies presenting a higher prevalence of iodine deficiency among pregnant women (Figure 2).
Sensitivity analysis by the leave-one-out method was not able to reduce heterogeneity (96%-97%), and the overall prevalence ranged from 33% to 42% (S3 Table is openly available in OSF repository (18). Even the exclusion of Marino et al. (32) ENT#091;39% (95% CI 36%-41%)ENT#093; and the subgroup of non-pregnant women from Ferreira et al. (31) ENT#091;40% (95% CI 37%-42%)ENT#093;, which were the only studies that presented analyses for non-pregnant women, were not able to reduce heterogeneity or significantly change the prevalence estimate. Sensitivity analyses with alternative statistical methods identified prevalence values ranging from 34% to 42% (S4 Table is openly available in OSF repository(18).
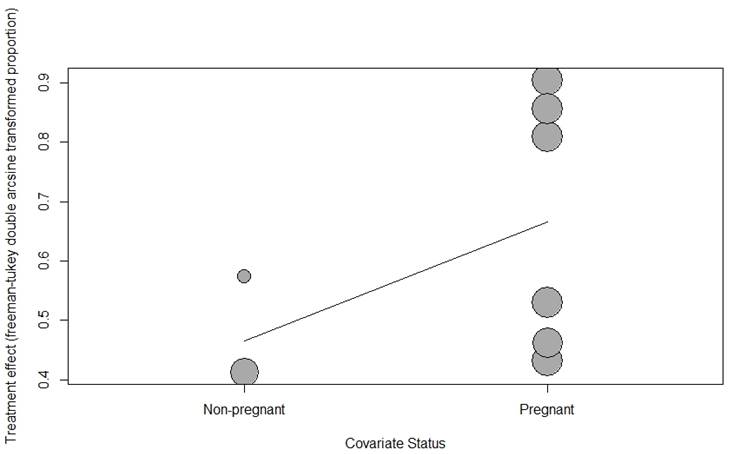
Meta-regression analyses were conducted using the following variables: the year of publication, age, and status (pregnant or non-pregnant). Corroborating the results of subgroup analyses, the status of pregnant or non-pregnant explained the heterogeneity identified in the meta-analysis (p <0.001) (Figure 3). Meta-regression or subgroup analyses to other variables were not possible due to poor reporting of participant characteristics. Furthermore, it was not possible to perform statistical and visual analyses of publication bias for any meta-analysis, as the methodological requirements for its performance were not met (i.e., at least 10 studies per meta-analysis and different prevalence estimates and samples).
Discussion
In this systematic review, seven studies assessing the prevalence of iodine deficiency were identified, especially in pregnant women. In pregnant and non-pregnant women, a prevalence of 40% and 13% iodine deficiency, respectively, were identified. Although several meta-analyses answered questions related to iodine deficiency (e.g., neonatal and maternal adverse events (34), iodine intake (35), average iodine concentration in milk (36,37) or urine (38), effect supplementation (39,40), among others), to our knowledge it is the first review to report the prevalence of iodine deficiency in women.
A meta-analysis conducted for the Brazilian population identified a prevalence of iodine deficiency of 5.1% for the general population, especially school children; and only two studies in pregnant women were identified (12). Recently (2020), a systematic review without meta-analysis assessed the implications of iodine deficiencies according to gestational trimesters and found 11 studies, none conducted in Brazil, and concluded that the second and third trimesters were the most affected by iodine loss (41). Our review identified five studies in pregnant women, and two of them reported results according to gestational trimesters. Although it was not possible to conduct a meta-analysis, these two studies reported similar prevalence between the gestational trimesters, ranging from 36% to 53%. Our findings differ significantly from the other reviews identified (12,41), mainly concerning the studies included, which may be due to the search date, the use of a more comprehensive search strategy, and the extensive manual and gray literature search.
All studies showed low methodological or reporting quality, which leads to less confidence about the findings, mainly due to inappropriate sampling methods and reduced sample size. This scenario seems common in observational (42,43), including prevalence studies. The studies with better quality were Marino et al. (32), Soares et al. (33), and Souza et al. (28). However, the three studies presented limitations regarding the sampling method, sample size, or response rate. Most studies presented small samples for the identified prevalence estimates (13% to 40%) and did not report a random probabilistic sampling, specific methods used in cluster sampling, or a minimum number of included participants. Therefore, whether by the convenience sampling technique or by the low response rate, the studies were limited in precision and representativeness of the target population.
In addition to the low-quality, high heterogeneity was identified, which decreased, even more, the confidence of the findings. This increased heterogeneity suggests that the studies should not be included in the same meta-analysis because they represented different iodine evaluations or participants (e.g., age, ethnicity, educational status, per capita income, or sociodemographic factors). Most of the studies did not report the characteristics of the participants, which precluded the conduction of a robust analysis to explore heterogeneity and identify possible associated factors.
Souza et al. (28) identified higher prevalence in participants with hypertension or salt-restricted diet; however, they included small sample size, impeding finding statistical difference with other subgroups. In pregnant women or hypertensive patients could be tempting to propose nutritional policies for universal preconception iodine supplementation (28). Nevertheless, the evidence on the effect of supplementation is still limited: two systematic reviews with a meta-analysis, which included 17 and 37 publications, respectively, identified conflicting results (39,40). The first review identified that iodine supplementation improves some maternal thyroid levels and may benefit aspects of cognitive function in school-age children (40). In contrast, the second one found that most studies showed no effect of supplementation with iodine on free thyroxine or thyroid-stimulating hormone and child cognitive, language, or motor scores (39). Both authors groups agreed with the need for further studies since the current evidence lacks methodological rigor.
In Brazil, a policy in force since the 1950s made mandatory salt iodination throughout the country (Decree No. 39,814, of 1956 (4)), which gained strength with the Ministry of Health Order No. 2,362, of December 1, 2005 (44) with the restructuring of the National Program for the Prevention and Control of Iodine Deficiency Disorders - DDI, called Pró-Iodine. It defined federal, state, and municipal responsibilities, including monitoring the iodine content of salt for consumption and the impact of iodination on the population. The policy showed to be successful for most of the population; nevertheless, in the current review, the subgroup with salt intake restrictions presented higher prevalence, which demonstrates the existence of groups at risk for iodine deficiencies with no specific national nutritional policies. However, even participants without hypertension or salt restriction presented iodine deficiency (39%-44%) (28).
Although iodine-containing supplement intake did not have conclusive evidence on their benefits for cases of iodine deficiency (39,40), supplements containing iodine are contraindicated to individuals on salt-restricted diets, evidencing the need for safe and effective strategies for this population. In Europe, a different approach to salt iodination and iodine supplementation seems to have contributed to reducing or eradicating iodine deficiencies in the population. They iodinate animal feed combined with the encouragement of consumption of milk and dairy products. However, this practice is not regulated in most European countries (45,46).
Otherwise, prenatal supplements in the pharmaceutical market contain several vitamins and minerals in their formulations, besides iodine. Therefore, criteria and caution should be done when prescribing them since overdose of some nutrients can occur, leading to adverse drug events. This hypothesis may explain the prevalence of iodine deficiency observed in the current study. In Brazil, iodine is available as a supplement containing iodine as part of the National Health Service strategic component (powder containing 90 mcg of iodine) and in the basic component as a Lugol solution (iodine, 20 mg / mL + potassium iodide, 40 mg / mL), used in the Schiller test (47) in the Brazilian National List of Essential Medicines (Rename). It is important to highlight that experts warn that the concentration of iodine in Lugol is high, and iodine excess is associated with impaired thyroid function (48). Thus, more robust evidence on effective and safe strategies is needed, considering the specificities of all population subgroups (e.g., hypertensive, pregnant women).
In this setting, our findings highlighted the complexity of the management of high-risk pregnant patients (e.g., hypertensive women) who need close monitoring during prenatal and the use of best evidence to back up the process of decision making. Thus, the primary healthcare level must identify them and articulate care transitions to specialized services when necessary (49). This approach promotes health conditions, pharmacological and non-pharmacological treatments and improves the mother and fetus safety.
A limitation of this study is that missing studies could exist, as with any systematic search. However, an extensive grey literature search was conducted to find unpublished studies and a manual search that found studies not retrieved by electronic search. Although proportional, many studies have been identified by manual search, which can be seen as a limitation of the search strategy. Our review could identify studies not covered by recent systematic reviews with similar questions, suggesting that several studies do not adequately create their titles and abstracts or are indexed incorrectly, making their retrieval challenging. Another limitation was the absence of a robust analysis of potential associated factors of iodine deficiency due to poor reporting and small meta-analyses (studies and participants). Finally, our systematic review assessed the iodine deficiency by UIC; however, other studies could evaluate the prevalence of goiter or determination of serum levels of thyroid-stimulating hormone and thyroglobulin.
Conclusion
Although this systematic review has identified studies with poor methodological and reporting quality, a higher prevalence of iodine deficiency was confirmed in pregnant women (40%) compared to non-pregnant women (13%), reinforcing the importance of national nutritional policies monitoring iodine status in these subgroups. Future studies should consider random probabilistic sampling, appropriate sample size, and pre-defined subgroup analysis to adequately inform prevalence of iodine deficiency and associated factors in women of childbearing age (non-pregnant, pregnant, and lactating) and to support health policies.