Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Suma Psicológica
versión impresa ISSN 0121-4381
Suma Psicol. vol.19 no.1 Bogotá ene./jun. 2012
Mónica Hattori-Hara
Universidad Autónoma de México, México
La correspondencia relacionada con este artículo puede ser dirigida a María del Rocio Hernandez-Pozo, correo electrónico: herpoz@unam.mx, o a Mónica Hattori-Hara, correo electrónico: saku678@yahoo.com.mx
Recibido: Enero 15 2012 Aceptado: Mayo 7 2012
Abstract
Elder population is becoming proportionally a larger segment of the total population and among their health problems, diabetes mellitus (DM) is one of their main causes of death and disability. In DM, self-management is the basis for a better control, which is why public policy makers and healthcare providers should have available analytic tools that allow them to discriminate among the best self-care interventions in diabetes for older patients. Even though there are several meta-analyses already that offer this kind of review, this article proposes the use of Mechner's behavioral contingencies language to compare different approaches. Three interventions were described with this notation and even though there were some limitations for this analysis due to the fact that some results were not comparable or not available in the original papers, this formal symbolic language demonstrated to be useful for making analytical comparisons visually accessible, providing a better understanding of the contingencies that are at play in the situation and giving the advantage of cutting across all natural languages.
Keywords: formal contingency language, diabetes mellitus, elderly, self-management, Mechner.
Resumen
Actualmente existe un incremento en la proporción de adultos mayores (AM) en la población en general. Dentro de los problemas de salud de este grupo, la diabetes mellitus (DM) es uno de los padecimientos que causa mayor muerte e incapacidad. En la DM el auto-manejo es la base para un mejor control, por lo cual los tomadores de decisiones en política pública y los proveedores de servicios de salud, deben contar con herramientas de análisis que les permitan discriminar entre las mejores intervenciones que mejoren el auto-cuidado del paciente diabético mayor. A pesar de que ya existen a la fecha varios meta-análisis que hacen este tipo de revisiones, este artículo propone el uso del lenguaje de análisis contingencial de la conducta desarrollado por Mechner para comparar diferentes aproximaciones. Tres intervenciones fueron descritas usando esta notación y a pesar de existir ciertas limitaciones para el análisis debido a que algunos componentes de los estudios no eran comparables o no estaban disponibles para su consulta en los documentos originales, éste lenguaje gráfico fue útil para hacer visualmente accesible el análisis comparativo entre estudios, proveyendo un mejor entendimiento de las contingencias en juego dentro de la situación, con la ventaja de traspasar la barrera del idioma.
Palabras clave: Lenguaje de análisis contingencial, diabetes mellitus, vejez, auto-manejo, Mechner.
Nowadays all over the world, there is a demographic phenomenon in which elder individuals are becoming an proportionally increasing component of the total population, in 1950 there were 205 millions people aged 60 years old or over throughout the world (8.11%), in 2000 this number increased to 606 millions (10%) and this group expanded to near 2 billions in 2005 (21%); this global trend in aging population is unprecedented, pervasive and an enduring demographic event that is having profound implications in many areas of human life (United Nations [UN], 2002).
The worldwide fertility and mortality decline and the life expectancy increase, underlie this phenomenon and draw attention to this specific segment of the population. Old age forces people to face many declining processes that can increase the risk of diseases development and it is at this period of life when cumulative results of unhealthy life style habits become apparent in the form of chronic health problems, which increase the demand of healthcare services (Frolkis, 1992; Rodríguez, 1998; UN, 2002; Velasco & Sinibaldi, 2001).
Among the chronic health problems, diabetes mellitus (DM) is one of the main causes of death and disability. The World Health Organization (World Health Organization [WHO], 2008) estimates that there are 180 million of people with this disease and this would increase to 366 million of people in 2030. According to the American Diabetes Association (American Diabetes Association [ADA,] 2001) and Latin American Diabetes Association (Latin American Diabetes Association [ALAD], 2008), diabetes affects one out of fve people over the age of 65, which is 20% of the elders. This means that among the elderly population diabetes is a growing problem and a large proportion of newly diagnosed diabetics belong to this group.
Two longitudinal studies, the Diabetes Control and Complication Trial (DCCT, 1993) and the United Kingdom Prospective Diabetes Study (Riddle, 2000) confrmed that maintaining the blood glucose near normal levels reduce or prevent acute and chronic complications of diabetes, this improvement of glucose control with its consequent risk decrease, would result in considerable health care cost reduction (ALAD, 2008) and substantial benefits in the quality of life of people with diabetes (Cárdenas, Pedraza & Lerma, 2005; Cochran & Conn, 2008; Leeman, 2006).
In diabetes, medical therapy alone is not enough to improve and maintain normal levels of blood glucose, in order to do that, it has to be combined with changes in life style habits and with effective patient education (Cornell & Briggs, 2004; Horton, Cefalu, Haines, & Siminerio, 2008), for this reason it is imperative that diabetic patient should get engaged with their self care.
Several studies have been conducted to examine self management enhancing programs (Ellis et al., 2004; Riveros, Cortazar-Palapa, Alcazar, & Sánchez-Sosa, 2005; Steed et al., 2005), but public policy and health care providers are not only interested in the investigations of how to improve self-care in people with diabetes, but also in the comparison between them, for searching the best interventions that should be selected for investment.
Analysis based upon a formal language tool for comparing interventions might be particular useful for specialist, given that it provides a synthetic way to portray relations among key elements, that avoids ambiguity associated to verbal descriptions and that could make evident relationships among variables that otherwise could not be revealed.
Introduction to the behavioral contingency language
Behavioral contingency language (Mechner, 2008b) is a system created and developed to portray the basic units and parameters of the contingency susceptible for manipulation or adjustment, by means of which certain behavioral effects could be produced. It consists of a set of abbreviations and symbols, which represents some units of analysis, its qualities and relations. This language is suitable for representing the contingencies investigated in psychological experiments in a formal graphical way.
Contingencies refers to an "if..., then" situation, where the "if" represents a behavior or an event and its consequences would be the "then" part. This means, a contingency is a situation in which two events are related to each other in a conditional way.
Therefore a contingency involves an act (A) with a consequence (C). The first part of the contingency also can be a time interval (t), but if there is an act, this act has to be performed by an agent (a) that would be represented by an arbitrary non capital letter. These are the four basic nouns for the analysis: acts, consequences, time and agents. Subscripts for these nouns, identifed with an arbitrary numeral indexed to a legend where the referenced entity is described or differentiated. Additionally superscripts are used to qualify attributes for the nouns, superscripts play the function of adjectives and adverbs (like: valence, magnitude, probability, duration or variability).
Like in normal language, in this notation verbs are needed to make sense to the ideas; there are four main verbs: consequate, prevent, predict and perceive.
Consequate, meaning to cause something, is the base of the contingency and would be represented by an arrow beginning in the precedent and finishing in the consequence
Prevent means avoiding something as a result of an act or time interval, this verb would be represented by a vertical arrow beginning in the first part of the conditional, and cutting a consequate horizontal arrow 
This verb has more sense if we remember that behavioral contingencies exist independently of the dynamic that could occur as a result of their existence, it means that the only existence of behavioral contingency could have an effect on the real behavior and this could change the action course of the agent behavior.
The other two verbs used in this notation are represented by the location of the agent that either perceives or predicts an agent, an act, or a consequence. The location for the agent performing the perception takes the lower lefit quadrant, meanwhile for prediction it takes the upper lefit one of the affected element. Additional elements of the language are the not symbol (a tilde) and a vertical bracket, this last meaning simultaneity of the elements that encompasses, for more detail see Mechner (2008a, 2008b, 2009, 2011).
This article proposes the use of Mechner's behavioral contingencies language, to analyze and compare three studies that evalúate interventions designed to improve diabetes self management in the elderly. By defining and establishing basic units across three studies and making relationships visually accessible, this tool offers a graphical comparison that makes the data visually accessible and allows understanding in an easy, fast and intuitive way the resources needed, the people involve and the results obtain in each intervention, simplifying comparison in function costbenefit analysis.
Method
This paper is a descriptive, theoretical and refexive work that analyzes and compares three interventions designed to improve self-management in the elderly by means of a behavioral contingency language developed by Mechner (2008a).
Sample
Three articles fulflling the inclusion criteria of being interventions aimed to improve diabetes self-management of people over sixty years old were selected to form part of the comparison exercise, taking care that they had some comparable features between them and some different properties to be illustrated by the Mechner's notation.
The Heisler & Piette (2005) article was chosen for being simple to translate and understand in behavioral contingency language for those that are unfamiliar with this kind of notation, Wilson & Pratt (1987) article is the only one that incorporates in the same article three groups to be compared and also three comparison times: pre, post and follow up measures, so multiple comparisons were illustrated in this case; finally the Siminerio, Piatt & Zgibor (2005) article allowed the opportunity to represent iterations of series of sessions with a specific length during the intervention.
Procedure
Articles that reported interventions in diabetes to improve self-care were looked up in specialized journal search platform databases: SAGE, PROQUEST and EBSCO host. The words used for the search were diabetes combined with self-care, self-management, or intervention. No exhaustive search was done because it was not the objective of this paper.
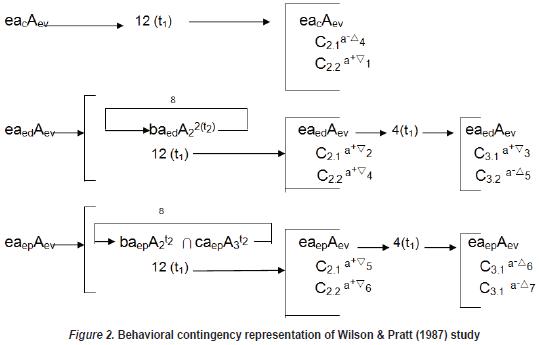
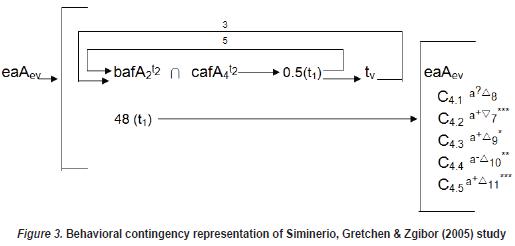
Three articles were selected for the analysis and the strategies used in these studies were translated to the contingency language.
For the translation agents, acts and time intervals were identifed in the articles, for each property common units were established for the three studies, for example for agents "a" was patients, "b" dietitian, "c" other health provider and "e" the evaluator; time was established as T1 = 1 week, so it could be easier to remember and compare among the fgures, in the first study for example, six weeks could be represented by 6(T1), in the second study twelve weeks could be represented by 12(T1) and its follow up with 4(T1).
Once common basic units were established, specific features were written in Table 1, for example, agent "c" for study three was specifically a certifed diabetes educator. The properties that could not be expressed in common units like, for instance, consequences, were defined separately and indicated in the Table too.
In the interventions, the human resources needed for it were established as the agents of the act and since the patients participated in the interventions, they were represented as agents too.
Following this steps and the suggestions of Mechner's articles (2008a, 2008b, 2009, 2011) the studies were translated to the behavioral contingency language. Finally the article was sent to two experts in the notation, which gave feedback to improve the figures.
Results
Heisler & Piette (2005) conducted the first study reported here; they implemented a peer support program using an interactive voice response (IVR) based platform to facilitate contact between peers. Forty older adults participated in this study (mean age=63.6, sd=7.8) with type 2 diabetes and poor glycemic control (A1C > 8%), they received training on how to use the IVR platform and were matched based on their diabetes related self-management needs. They were asked to contact their partner weekly during a six weeks period. The measures were diabetes care self-efficacy (C1.1), diabetes self-management behaviors (C1.2 which includes: medication, exercising, eating plan, checking blood sugar level and checking their feet for wounds or sores) and depression (C1.3). There were significant differences in the pre-post test evaluations of self-efficacy from 55.9 to 73.7 (p < .01), of self-management from 71.2 to 75.4 (p ≤.05), however there were not significant changes in depression 4.4 to 5.2 (p = .39).
This study is represented in the notational system in a very simple way. In fgure one Aev means the evaluations in two different times: Before and after the intervention (A ). The recycling arrow  shows that the intervention, that is: calling to their partners, is repeated a certain number of times, in this case it iterates a variable number of times (v) until the study is over, a total of 6 weeks (see Table 1). When A1 was over the changes between pre and post-evaluation in the three measures are said to be the consequence of the intervention. Here the asterisk (*) is used to indicate level of significance, in the same way it is used in the statistical notation for scientific papers. Also, this study shows that increases (Δ) in C1.3 were damaging or negative (-) for the agent "a", but this change was not significant.
shows that the intervention, that is: calling to their partners, is repeated a certain number of times, in this case it iterates a variable number of times (v) until the study is over, a total of 6 weeks (see Table 1). When A1 was over the changes between pre and post-evaluation in the three measures are said to be the consequence of the intervention. Here the asterisk (*) is used to indicate level of significance, in the same way it is used in the statistical notation for scientific papers. Also, this study shows that increases (Δ) in C1.3 were damaging or negative (-) for the agent "a", but this change was not significant.
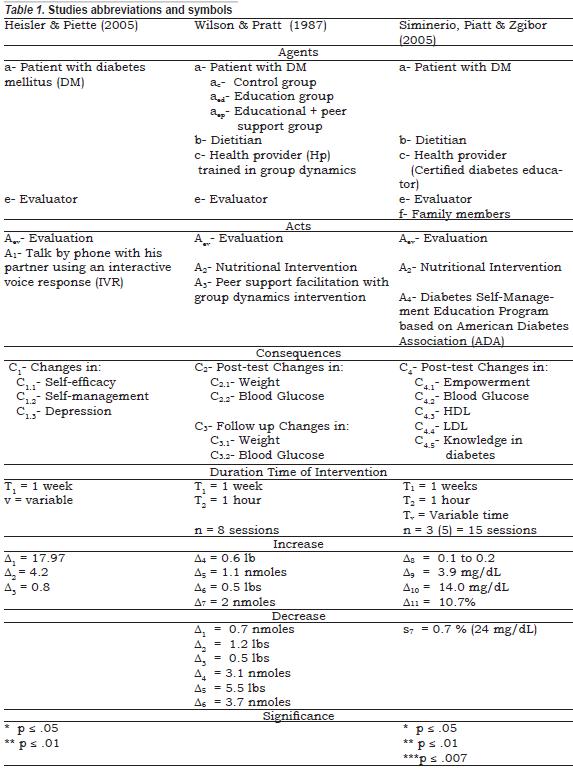
The second study by Wilson & Pratt (1987) assessed the impact of diabetes education and peer support interventions on weight loss and glycemic control in glycosylated hemoglobin (GHb) of 79 elders (mean age 68.2, sd = 7.2). Three not randomized groups were formed including: control (c), educational (e) and educational with peer support (ep) groups. This study had prepost evaluations and a follow up.
At the post-test (C2) the "c" group gained +0.6 lbs, the "ed" group just lost -1.2 lbs and the "ep" group had a moderate weight loss of -5.5 lbs. About the glycemic control there was a reduction of the GHb in the three groups, a very small in the "c" group (0.8 nmoles) and a moderate reduction on the intervention groups: "ed" group -3.1 nmoles and "ep" -3.7 nmoles. During the follow up (C3) there were no important reductions in any of the groups, so the authors concluded that "ep" facilitated reductions in weight and GHb levels at least on a short-term basis.
In this study each group was identifed by the subscript of the agent's letter (a). For the control group there were two evaluations (Aev) and for the others there were three: a pre-test, a post-test (C2) and a follow up (C3). Figure 2 shows differences in interventions for each group; in the first group no intervention is shown, in the second nutritional intervention is represented by A2, and in the third group, additional to A2 but with half the duration it was in group two (t2), a diabetes self-management educational program was delivered by agent c, here the ∩ symbol was used to mean that both interventions where carried out in this group.
As mentioned before, the authors of this study assumed different outcomes for each intervention, in terms of reductions in weight and in GHb levels. In Mechner's notation increase is represented by delta (Δ) but as far as the available published papers, there is no decrease symbol yet in the system, here it is suggested to represent it with the nabla symbol (∇), additionally arbitrary numeral subscribes were added to both symbols (Δ ∇) to been identifed and referenced in Table 1 for more detailed information of the change size.

In the first group an increase or stable value is expected in the post test; as shown in Figure 2, weight values increased as expected, but GHb levels did not varied the same way, therefore in this case we need more detailed information in order to compare the two scenarios, for example like in the first study significance differences could be helpful.
Siminerio, Piatt & Zgibor (2005) did the third study selected and represented in Figure 3, they implemented a chronic care model for improving diabetes care in a rural community that was implemented in three phases, for this article just the direct intervention with the population is discussed. There, 29 people participated with a mean age of 67, sd = 8.1 with diabetes mellitus type 2 and poor glycemic control (A1c > 7%).
The process included an initial evaluation of indicators of patient's diabetes control of fve elements: empowerment, hemoglobin A1c in mg/dL, high-density lipoprotein levels (HDL), low-density lipoprotein levels (LDL) and knowledge of diabetes. Then, family (f) and patients (a) participated in the intervention that consisted in a medical nutrition therapy supplied by a dietitian (b) and a diabetes self-management education program based on American Diabetes Association Standards guide 2005 provided by a certifed diabetes educator (c), this program consisted of three series of fve 2 hours group sessions, that is 30 hours total, the sessions were twice a week (0.5 * t1) but the time between series of sessions are undefined so here that time was represented as variable (tv).
Diabetes education program included goal-setting and behavioral change strategies on the following subjects: disease process, nutrition management, physical activity, monitoring, medications, how to prevent, detect and treat acute complications, risk reduction in the prevention of chronic complications, psychological adjustment, goal setting and problem solving.
The consequences derived from the intervention seemed positive for agent a, except for LDL (C4.4) which increased in 14 mg/dl (p = .01) and was quite ambiguous in regard to empowerment (C4.1) because it did not have a significant change. Positive changes were A1c which decreased in .7% (p = .007), HDL increased in 3.9 mg/dl (p = .05), and an increment of knowledge in diabetes in 10.7% (p = .003).
Note the places in which each "t" is, duration of the session is written as a characteristic of each intervention, the span between sessions is written following the intervention as 0.5t1 which means they meet twice a week, this iterates fve times (number of sessions), after finishing the set of fve sessions an unspecifed time pass before a new fve sessions series began again, this intervention was along one year (48 weeks).
Discussion
The discussion of the articles was developed under the basis of the results found, the behavioral contingency language is a useful tool and as is detailed below, its main contribution used in this article was the access to general data in a visual and simple way, making easier the comparisons, exposure and understanding of the structure, resources and benefits reached with each intervention.
For the three studies, there are pre, posttest evaluations, the pre evaluations were not developed in detail in any study but the post evaluations were. The reason for this was to simplify the diagrams, by handling the post-test evaluations in terms of magnitude change and providing more detail whenever levels of significance per kind of intervention were available from the original studies.
Levels of significance were a key factor for interpreting the results of the evaluations, because they allow examining the impact of the interventions. Leading our conclusions under the idea that changes between pre, post-test evaluations are given by the intervention, magnitude of changes informed whether interventions were useful or not.
In Table 1, it can be seen that there are symbols shared between interventions, this was done in purpose for simplify the comparison between studies. As follows, the comparison between the used symbols will be described. Note that in this article two symbols that are not presented in Mechner's language, but that could be helpful in representing psychological issues are proposed, first , as written before, the representation of the significance of the difference between evaluations is suggested by using asterisks. The second symbol proposed here, is the one that represents decrease; it is suggested to use nabla (∇), since the Mechner's symbol for increase is delta (Δ).
For the agents note that letter "a" represents in all studies the elder patient with diabetes mellitus, in the second study there are three groups of agents "a", each one with a different intervention, this situation was represented with the subscript of each agent "a"; ac represents the control group, aed represents the group that only received education and aep represents the group that received education plus peer support. As can be seen in the three diagrams of the studies, "a" is always the agent of the pre, post-evaluation and following up, but in the intervention "a" is not always the only agent. In the first study it can be seen that the patients are the only ones who participated in the intervention by giving peer support among them, here "a" are the agents of the action.
In the second intervention; the second group ("aed") and the third group ("aep") participated in the interventions done by the dietitian ("b") and just the "aep" group participated in the intervention done by another health provider ("c"). Similar situation happened in the third intervention, with the difference that in this one the family members of "a", represented by letter "f" participated too.
Talking about persons implicated in the intervention as seen in the diagrams, we can say that the first study is very convenient, in one hand it almost does not need the health providers participation, this would make cheaper the program theoretically, on the other hand an intervention in which the patient is the support for other patients gives additionally advantages for this age group of patients, for example elder adults feel useful when helping others, they get the opportunity of mutual sharing experiences, to enhance feelings of well being and satisfaction and this activity could provide additional meaning and challenges for them (Whittemore, Rankin, Callahan, Leder, & Carroll, 2000), even more, being satisfed with the support given to others in the elderly had been associated with subsequent future health, heightened self-esteem and self-efficacy and improved quality of life (Ostir, Simonsick, Kasper, & Guralnik, 2002).
Reciprocal peer support program, in which the patient gave and receive peer support, had good results and if it is carefully designed and implemented, it could be a powerful way to help patients with chronic diseases, and a potentially low-cost, fexible procedure to supplement formal health care sup port (Heisler, 2007).
In the other two studies, the interventions included medical and nutritional aspects taught by a dietitian (A2), in the second group of the second research, patients not only received dietitian lessons but also received peer support dynamics given by a trained health provider (A3), in this group the decreases in weight and blood glucose were greater than in the other groups, this suggests that facilitating peer support in group format interventions makes it more efficient. A probable explanation could be that agents "a" had a more passive role in group one than in group two, this agrees with the conclusion of Norris, Engelgau & Narayan (2001), that educational interventions that involved patient collaboration should be more effective than didactic interventions in improving glycemic control, weight, and lipid profles, particularly in the short term; and that psychosocial interventions offered in a group format are a promising addition for diabetes education.
In the third study, patients participated in nutritional education (A2) and diabetes self-management education (DSME) (A4). In the DSME program, the patient had to participate actively in the sessions because this kind of program was designed to be a collaborative process through which people gain the knowledge and skills needed to modify behavior and successfully self-manage the disease and its related conditions (Magwood, Zapka, & Jenkins, 2008). This study had the additional advantage that the family could participate in it; in the study the authors did not emphasize this aspect, but it could be an important element and it can be easily perceived when the study is translated to the behavioral contingency language. Gallant (2003) in his review of empirical studies that had examined the relationship between social support and chronic illness self-management, found a positive relationship between them.
Comparing results of the three studies, changes from the pre to the post tests are apparent. On study one there was an increment in depression which had a negative valence for "a" but this change did not have a significant value; the other results evaluated were positive and significant for "a", which qualifes this intervention as positive for patients.
On the second study, results represented in Figure 2 suggest that there were positive changes for "a" in the intervention groups at least on a short-term basis, but it is difficult to say what happens for a long-term perspective. In the posttest for the no intervention group condition, just a small decrease in blood glucose was found, but in all post intervention evaluations, measures decreased in a moderate way. At all the follow up results, increases were found, except in weight of group aed. By looking at the size of the changes at Table 1, it can be seen that the increase in weight was similar to the one of the control group, and increases in blood glucose levels were smaller than the decreases in glucose after the interventions (see Table 1), these changes would suggest that the interventions had positive effects on the diabetes management indicators if and only if these changes were significant at the clinical or statistical levels. Unfortunately this information was not provided by the authors.
These results indicate that peer support intervention had better results at short-term, this agrees with the meta-analysis done by Norris, Lau, Smith, Schmid & Engelgau (2002), in which they concluded that a self-management education program improves blood glucose at immediate post-test and that benefits decline over a period of 1-3 months once the intervention ceases.
For the third study, results of the post-test show that there were many positive and significant changes for agent "a", in this example it is particularly useful the use of valence symbols to identify which direction changes are positive for the patients. For example, the LDL (C4.4) increased in a significant way, which was negative for the patient, this indicates that it is necessary to examine what happened at the intervention that affected this value in a negative way.
About the duration, the number of sessions, the length of each session and the time interval between evaluations, in the fgures one, two and three, program duration was represented with 6(t1), 12 (t1) and 48(t1) respectively (t1 = 1 weeks), it can be seen that the first study is the shortest, it lasted six weeks, the second was twice larger than the first study and the third intervention was four times the length of the second. In the first study there were no number of sessions, instead the numbers of calls a patient made to his peer was reported, regardless its length. At the second study there were 8 sessions of 2 hours each, this time was clearly distributed on different activities depending on the group (aed two hours of educational information, aep one hour of educational information and one of peer support activities), at last the third study had 15 sessions of two hours each one, which consisted of educational information and diabetes education without a fxed timetable.
If the three interventions had been an equivalent improvement in self-care for diabetes, other indicators that could be useful for evaluating them are the length of the intervention and the number of sessions involved, these features are visibly illustrated by means of adopting the method of Mechner's contingency notation. If the duration of the intervention or the number of trials are shorter or smaller, in both cases without losing its efficacy, it would imply that the particular type of intervention is a more effective one. Among these studies, it is not possible to conclude which one had the best result, because the measures were different, nevertheless it can be argued that the first study had the best time span (had the shorter duration), giving the patient an active role and that it had a positive impact, at least over the indicators provided by the study.
A disadvantage of the first study was that the period of time that lasted this study, did not allowed to take a glycosylated hemoglobin, that is, one of the best objective indicators for diabetes control, this indicator is the average of three months blood sugar level (Pérez & Ubaldo, 2008), and was given in the other two studies that were of larger duration, the solution for this could have been taking this indicator in a follow up evaluation after three months of the initial evaluation.
Conclusion
Diabetes Mellitus is a challenging problem for society, in special for older adults. In the absence of a cure for this progressive condition, prevention of complications by optimizing metabolic control, becomes the main purpose in its treatment, as well as improving quality of life and functional capacity through better diabetes self-management while keeping acceptable costs.
To achieve this aim, it is required to know which interventions are more useful, and which are not, and even more, which elements of the interventions could be changed in order to improve them. This means that understanding the relationship between interventions and outcomes, requires attention in the emergent evidence about important features of effective intervention programs.
Mechner's notation system is useful for identifying the agents that are needed as part of the intervention design, the elements of each intervention, the duration and the iteration of the sessions, among other characteristics. This graphic identification helps the specialist to compare the evidence of different studies in a clear form, and with that, public health decision makers and program planners could be guided to understand better diabetes, and to take prudent decisions about assessment, planning, and implementation of interventions.
In this article, the lack of similar indicator measurement prevented us to make a conclusive comparison among studies, although two studies used the level of blood glucose, which is an objective standardized indicator of diabetes control, the glucose levels reported in the studies were measured with different techniques, and reported using different units of analysis that did not allowed proper comparison between them.
So when using this notation, the selection of articles to be analyzed had to be made in a very careful way, remembering that not only comparable elements are needed in order to generate appropriate and clear conclusions, but also statistical elements or at least clinically sound differences in outcomes should be readily available. For example for the second study all the elements were comparable, but significance of the changes would have enriched the comparison intra-study.
This paper illustrates how the contingency language was used to compare three studies aimed to improve diabetes control for elderly patients. This analytic technique allowed to highlight specific aspects of interventions, outcomes and time features involved.
The translation of interventions in a common formal contingency language is an important tool that could be used for specialist to select the best procedures according to a wide set of factors at hand that might influence the decision making process for a specific population, based on theoretical knowledge, cost, impact of the intervention in a degree of details tailored to specific interests or perspectives. But it should not be forgot that Mechner's proposed language is an instrument for representing the data of the studies in a squematic way and not a technique for judging among them, so it may be necessary to construct a table to have access to more detailed information, as we did in the present analysis.
One of the principal limitations of this approach is the number of people that are able to use it, since it is a symbolic language, it requires to be learned, that is how to write and read it, at the beginning this could be complex (as it is for any other ability), but once is learned it opens up a different way to see and weight the influence of events, based on the contingencies involved.
If this notation could be used for a more extensive community, communication between professionals could transcend idiom barriers and also it could be enriched with new propositions for expressing other kind of relationship. By now the contingency language as other symbolic language such as mathematics, is a powerful tool for analysis of behavior and it may be possible to extend its use to other non-behavioral areas, as long as they refer to contingencies (Mechner, 2008), under other framework its usage may be limited.
Acknowledgments
We want to give thanks Doctor Francis Mechner and Laurilyn Jones for the comments and feedback that they gave to us for improve the fgures of this paper, despite this, all the responsibility of any mistake or miss is ours, the articles authors.
References
American Diabetes Association. (2001). Diabetes and the Elderly. Clinical Diabetes, 14, 176, retrived from http://dx.doi.org/10.2337/diaclin.19.4.176. [ Links ]
Asociación Latinoamericana de Diabetes (2008). Guía de diagnóstico, control y tratamiento de la Diabetes Mellitus tipo 2. Washington: Organización Panamericana de la Salud. [ Links ]
Cárdenas, V., Pedraza, L., & Lerma, C. (2005). Calidad de vida del paciente con diabetes mellitus tipo 2. Ciencia UANL, 8, 351-357. [ Links ]
Cochran, J., & Conn, V. (2008). Meta-analisys of Quality of Life Outcomes Following Diabetes Self-Management Training. The Diabetes Educator, 34, 815-823, retrieved from http://dx.doi.org/10.1177/0145721708323640. [ Links ]
Cornell, S., & Briggs, S. (2004). Newer Treatment Strategies for the management of Type 2 Diabetes Mellitus. Journal of Pharmacy Practice, 17, 49-54, retrieved from http://dx.doi.org/10.1177/0897190003261308. [ Links ]
Diabetes Control and Complications Trial Research Group (1993). The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-De-pendent Diabetes Mellitus. The New England Journal of Medicine, 329, 977-986, retrieved from http://dx.doi.org/10.1056/NEJM199309303291401. [ Links ]
Ellis, D., Naar-King, S., Frey, M., Templin, T., Rowland, M., & Greger, N. (2004). Use of Multisystemic Therapy to Improve Regimen Adherence Among Adolescents with Type1 Diabetes in Poor Metabolic Control: A Pilot Investigation. Journal of Clinical Psychology in Medical Settings, 11, 1746-1747, retrieved from http://dx.doi.org/10.1023/B:JOCS.0000045351.98563.4d. [ Links ]
Frolkis, V. (1992). Syndromes of aging. Gerontology, 38 (1-2), 80-86, retrieved from http://dx.doi.org/10.1159/000213310. [ Links ]
Gallant, M. (2003). The Influence of Social Support on Chronic Illness Self-Management: A review and directions for Research. Health Education & Behavior, 30, 170-195, retrieved from http://dx.doi.org/10.1177/1090198102251030. [ Links ]
Heisler, M. & Piette, J. (2005). "I Help you, and you help me". Facilitated telephone peer support Among Patients With Diabetes. The Diabetes Educator, 31, 869-878, retrieved from http://dx.doi.org/10.1177/0145721705283247. [ Links ]
Heisler, M. (2007). Overview of Peer Support Models to Improve Diabetes Self-Management and Clinical Outcomes. Diabetes Spectrum, 20, 214-221, retrieved from http://dx.doi.org/10.2337/diaspect.20.4.214. [ Links ]
Horton, E., Cefalu, W., Haines, S., & Siminerio, L. (2008). Multidisciplinary interventions: Mapping New Horizonts in Diabetes Care. The Diabetes Educator, 34, 78S-89S, retrieved from http://dx.doi.org/10.1177/0145721708321148. [ Links ]
Leeman, J. (2006). Interventions to improve Diabetes self-management: utility and relevance for practice. The Diabetes Educator, 32, 571-583, retrieved from http://dx.doi.org/10.1177/0145721706290833. [ Links ]
Magwood, G., Zapka, J., & Jenkins, C. (2008). A review of Systematic Reviews Evaluating Diabetes Interventions. Focus on Quality of Life and Disparities. The Diabetes Educator, 34, 242-265, retrieved from http://dx.doi.org/10.1177/0145721708316551 [ Links ]
Mechner, F. (2008a). Behavioral contingency analysis. Behavioral Processes, 78, 124-144, retrieved from http://dx.doi. org/10.1016/j.beproc.2008.01.013. [ Links ]
Mechner, F. (2008b). Applications of the language for codifying behavioral contingencies. retrieved from http://mechnerfoundation.org/pdf_downloads/Applications%20of%20BCA.pdf. [ Links ]
Mechner, F. (2009). Behavioral Contingency Analysis. A formal language for the analysis of complex situations. retrieved from http://mechnerfoundation.org/pdf_downloads/Behavioral%20Contingency%20Analysis.pdf. [ Links ]
Mechner, F. (2011). Why behavior analysis needs a formal symbolic language for codifying behavioral contingencies. European Journal of Behavior Analysis, 12 , 93-104. [ Links ]
Norris, S. L., Engelgau, M. M., & Narayan, K. M. (2001). Effectiveness of Self-Management Training in Type 2 Diabetes A systematic review of randomized controlled trials. Diabetes Care, 24, 561-587, retrieved from http://dx.doi.org/10.2337/diacare.24.3.561. [ Links ]
Norris, S. L., Lau, J., Smith, S. J., Schmid, C. H., & Engelgau, M. M. (2002). Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care, 25, 1159-1171, retrieved from http://dx.doi.org/10.2337/diacare.25.7.1159. [ Links ]
Ostir, G., Simonsick, E., Kasper, J., & Guralnik, M. (2002). Satisfaction with support given and its association with subsequent health status. Journal of Aging and Health, 14, 355-369, retrieved from http://dx.doi.org/10.1177/08964302014003003. [ Links ]
Pérez, E., & Ubaldo, V. (2008). Guía para el paciente y el educador en Diabetes (4a. ed.). México: Editorial Independiente. [ Links ]
Riddle, M. (2000). Managing Type 2 Diabetes Over Time: Lessons From the UKPDS. Diabetes Spectrum, 13, 194-200. [ Links ]
Riveros, A., Cortazar-Palapa, J., Alcazar, F., & Sánchez-Sosa, J. (2005). Efectos de una intervención cognitivo-conductual en la calidad de vida, ansiedad, depresión y condición médica de pacientes diabéticos e hipertensos esenciales. International Journal of Clinical and Health Psychology, 5, 445-462. [ Links ]
Rodríguez, F. (1998). La vejez y la muerte. Anales de Psicología, 14, 127-135. [ Links ]
Siminerio, L., Piatt, G., & Zgibor, J. (2005). Implementing the Chronic Care Model for Improvements in Diabetes Care and Education in a Rural Primary Care Practice. The Diabetes Educator, 31, 225-233, retrieved from http://dx.doi.org/10.1177/0145721705275325. [ Links ]
Steed, L., Lankester, J., Barnard, M., Earle, K., Hurel, S., & Newman, S. (2005). Evaluation of the UCL Diabetes Self-Management Programme (UCL-DSMP): A Randomized Control Trial. Journal of Health Psychology, 10, 261-276, retrieved from http://dx.doi.org/10.1177/1359105305049775. [ Links ]
United Nations (2002). World Population Aging: 1950-2050. Retrived from http://www.un.org/esa/population/publications/worldageing19502050. [ Links ]
Velasco, C., & Sinibaldi, G. (2001). Manejo del enfermo crónico y su familia. México: Manual Moderno. [ Links ]
Whittemore, R., Rankin, S., Callahan, C., Leder, M., & Carroll, D. (2000). The peer advisor experience providing social support. Qualitative Health Research, 10, 260-276, retrieved from http://dx.doi.org/10.1177/104973200129118408. [ Links ]
Wilson, W., & Pratt, C. (1987). The Impact of Diabetes Education and Peer Support upon Weight and Glycemic Control of Elderly Persons with Noninsulin Dependent Diabetes Mellitus (NIDDM). American Journal Public Health, 77, 634-635, retrieved from http://dx.doi.org/10.2105/AJPH.77.5.634. [ Links ]
World Health Organization (2008). Diabetes. retrieved from http://www.who.int/dietphysicalactivity/publications/facts/diabetes/en/. [ Links ]













