Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Avances en Enfermería
Print version ISSN 0121-4500
av.enferm. vol.28 no.2 Bogotá July/Dec. 2010
JOAN E. DODGSON1, AMANDA L. WATKINS2, MYUNGHAN CHOI3
1 PhD in Nursing from the University of Minnessota , Associate Professor of Nursing at Arizona State University College of Nursing & Health Innovation. Joan.Dodgson@asu.edu, Phoenix, Arizona, United States of America
2 MS, RD, IBCLC , RLC, Doctoral Student & Research Assistant Arizona State University College of Nursing & Health Innovation. Amanda.L.Watkins@asu.edu, Phoenix, Arizona, United States of America
3 PhD, MPH, APRN-B Assistant Professor, Research Arizona State University College of Nursing & Health Innovation Myunghan.Choi@asu.edu, Phoenix, Arizona, United States of America
Recibido: 2-06-10 Aprobado: 17-09-10
Abstract
Study objectives: (1) describe the existing supportive hospital breastfeeding practices in a major urban region and (2) determine if supportive hospital breastfeeding practices are influenced by hospital characteristics.
Methods: A cross-sectional telephone survey of all hospitals with maternity services (N = 21) in Maricopa County, Arizona (USA), was conducted between July 2009 and March 2010. This major urban county, which includes Phoenix, is the fourth largest city in the USA. Supportive breastfeeding practices were 12 maternity care practices consistent with WHO Baby Friendly Hospital Initiative Ten Steps. Hospital characteristics measured were professional breastfeeding services available, institutional ownership, number of births per year, births paid for by public funds, and the level of care provided. Descriptive and inferential statistics were conducted.
Results: The total number of supportive practices ranged from 5 to 10 (M = 7.52; SD = 1.53). Two practices were uniformly implemented; the remainder varied from low (> 25%) to moderate (50-75%) levels of implementation. 86% of hospitals had widespread use of supplements and provided gift bags containing formula. The number of Board Certified Lactation Consultants (IBCLCs) employed by a hospital was the only variable predicting higher levels of supportive practices. Facility ownership status was significantly correlated with the number of IBCLCs.
Discussion: The differences in supportive hospital practices among hospitals suggest the effectiveness of IBCLCs in changing practice; however, additional research is needed to further explore this thesis. Findings of this study, while unique to the community studied, were consistent with a number of findings reported by researchers around the globe.
Keywords: breast feeding, feeding behavior, postnatal care, hospitals
Resumen
Objetivos del estudio: (1) describir las prácticas de lactancia hospitalaria de apoyo en una gran región urbana y (2) determinar si las prácticas de lactancia hospitalaria de apoyo están bajo la influencia de características hospitalarias.
Métodos: entre los meses de julio de 2009 y marzo de 2010 se realizó una encuesta telefónica transversal en todos los hospitales con servicios de maternidad (N = 21) en el Condado de Maricopa, Arizona (USA). Este gran condado urbano, que incluye Phoenix, es la cuarta ciudad más grande de Estados Unidos. Las prácticas de lactancia de apoyo se refirieron a 12 prácticas de cuidados de maternidad acordes con los Diez Pasos e Iniciativas Hospitalarias Amigables para el Bebé de la OMS. Las características hospitalarias medidas fueron: servicios de lactancia disponibles, propiedad institucional, número de nacimiento al año, nacimientos pagados por fondos públicos, y el nivel de atención suministrado. Se realizaron estadísticas descriptivas e inferenciales.
Resultados: El número total de las prácticas de apoyo variaba de 5 a 10 (M = 7.52; SD = 1.53). Se aplicaron de forma uniforme dos prácticas; el resto variaba entre niveles de implementación bajo (> 25%) y moderado (50-75%). Ochenta y seis por ciento de los hospitales utilizan ampliamente suplementos y dan bolsas de regalo con leche de fórmula. El número de de Consultores de Lactancia Certificados (IBCLC por sus siglas en inglés) empleados por un hospital fue la única variable que predecía mayores niveles de prácticas de apoyo. El estatus de propiedad de la instalación estaba ampliamente relacionado con el número de IBCLC.
Discusión: Las diferencias en las prácticas hospitalarias de apoyo entre hospitales sugieren la efectividad del IBCLC en cuanto al cambio de prácticas; sin embargo, se necesita investigación adicional para explorar aún más esta tesis. Los hallazgos de este estudio, únicos para la comunidad estudiada, eran consistentes con varios de los hallazgos reportados por investigadores en todo el mundo.
Palabras clave: lactancia materna, conducta alimentaria, atención posnatal, hospitales (fuente: DeCS, BIREME).
Resumo
Objetivos do estudo: (1) descrever as práticas de lactância hospitalar de apoio em uma importante região urbana e (2) determinar se as práticas de lactância hospitalar de apoio são influenciadas pelas características hospitalares.
Métodos: entre os meses de julho de 2009 e março de 2010 foi realizado um questionário telefônico transversal em todos os hospitais com serviços de maternidade (N = 21) no Condado de Maricopa, Arizona (USA). Este importante condado, que inclui Phoenix, é a quarta maior cidade dos Estados Unidos. As práticas de lactância de apoio eram 12 práticas de cuidados de maternidade congruentes com os Dez Passos e Iniciativas Hospitalares Amigáveis para o Bebê da OMS. As características hospitalares medidas foram as seguintes: serviços de lactância disponíveis, propriedade institucional, número de nascimentos por ano, nascimentos pagos por fundos públicos, e o nível de atenção fornecido. Realizaram-se estatísticas descritivas e inferenciais.
Resultados: O número total das práticas de apoio variava de 5 a 10 (M = 7.52; SD = 1.53). Aplicaram-se de forma uniforme duas práticas; o resto variava entre níveis de implementação baixo (> 25%) e moderado (50-75%). Oitenta e seis por cento dos hospitais utilizam amplamente suplementos e dão sacolas de presente que contêm leite formulado. O número de Consultores de Lactância Certificados (IBCLC pelas siglas em inglês) empregados por um hospital foi a única variável que predizia maiores níveis de práticas de apoio. O estado de propriedade da instalação estava amplamente relacionado com o número de IBCLC.
Discussão: As diferenças nas práticas hospitalares de apoio entre hospitais sugerem a efetividades do IBCLC quanto à mudança de práticas; contudo, é preciso fazer outras pesquisar para explorar ainda mais esta tese. Os achados deste estudo, únicos para a comunidade estudada, eram congruentes com vários dos achados mostrados por pesquisadores no mundo inteiro.
Palavras chave: aleitamento materno, comportamento alimentar, cuidado pós-natal, hospitais
INTRODUCTION
Worldwide the importance of supporting and promoting exclusive breastfeeding during an infants' first year of life is a major public health priority. Public health campaigns aimed at reaching this goal on a population level only have had moderate success, particularly in developed countries, perhaps due to the options readily available to many women in these more affluent countries. Many sociocultural factors have been identified as contributing to the wide spread use of breast milk substitutes, including marketing and the distribution of free formulas to hospitals, health care providers and new mothers. A major factor in women's successful initiation and continuation of exclusive breastfeeding is hospital maternity care practices. A solid and extensive body of research has been done on the nature of maternity care practices that are supportive of successful breastfeeding, not only during hospitalization but also beyond this period (1-5). Yet, hospital practices often do not meet these established international standards of care. The contextual factors affecting this situation remain less studied. The characteristics of the institutions offering maternity services may affect practices within that institution in ways that have not been well studied. The purpose of this study was to describe the existing supportive hospital breastfeeding practices in a major urban region and to determine if hospital characteristics are associated with their implementing supportive breastfeeding practices.
BACKGROUND
Breastfeeding provides infants with optimal nutrition and has many preventative health effects that have been well established by a large body of research. As the result of considerable local, regional and international promotion efforts, breastfeeding initiation rates have increased in many areas around the globe. However, the benefits of breastfeeding for mothers and infants are dose-dependent, highlighting the importance of exclusive breastfeeding for longer periods (ideally the first year of life) and directing public health efforts toward improving rates of exclusive breastfeeding and of duration. These efforts have not been as successful as they were expected. Unsupportive hospital practices often have been identified as contributing to early supplementation of foods other than breast milk and to early weaning. Conversely, hospital practices that are supportive of breastfeeding have been associated with increased rates of exclusive breastfeeding and later weaning times (1,6).
Professional hospital staffs' education about breastfeeding management has repeatedly been associated with higher breastfeeding rates and more supportive breastfeeding practices (4). Professional lactation support services provided by International Board Certified Lactation Consultants (IBCLC) have been associated with more supportive hospital practices (7, 8). Staffing standards for the adequacy of lactation services have been suggested (9), but no consensus has been reached.
Worldwide more than 15,000 hospitals have been certified as Baby Friendly by WHO (10). Although the Baby Friendly Hospital Initiative designation was established for individual hospitals, globally this designation affects breastfeeding initiation, exclusivity and duration on a community and national level (5, 6, 11, 12). In Taiwan, researchers demonstrated a dose-response relationship between the number of 10-step supportive breastfeeding hospital practices and breastfeeding initiation and exclusivity (13). Since the BFHI was implemented in Sweden in 1993, the 6 month breastfeeding rate increased from a pre-BFHI implementation rate of 58% in 1992 to 72% in 2000 (14). Likewise, Switzerland implemented the BFHI and has seen the national median duration of any breastfeeding rise from 22 weeks in 1994 to 31 weeks in 2003 (15). A 5-year follow-up assessment of BFHI designated hospitals in Brazil highlighted the importance of continued monitoring of these hospitals to maintain adherence to all the practices (16). Abrahams and Labbok (6) utilized country-level data to examine the relationship between BFHI implementation and trends in exclusive breastfeeding across 14 developing countries. Although changes in exclusive breastfeeding rates at 2 and 6 months were not significant, increases did occur after the BFHI implementation. The researchers suggest small sample sizes may have attenuated the results.
Although relatively few hospitals are Baby Friendly in the United States, several studies highlight the positive impact Baby-Friendly practices have had on breastfeeding exclusivity and duration (6, 12). Mothers who experienced 6 Baby-Friendly practices measured on the national Infant Feeding Survey (2005-2006) were 13 times more likely to be breastfeeding at 6 weeks than mothers who did not experience any of the Baby- Friendly practices (11). Merewood et al. (5) analyzed all breastfeeding data from US Baby-Friendly hospitals (N = 29) in 2001, both rates of initiation and exclusivity were higher in the BFHI hospitals than national, regional, and state rates regardless of sociodemographic factors commonly associated with lower breastfeeding rates. Rosenberg et al. (17) analyzed data from 57 hospitals in Oregon; they found breastfeeding rates at 2 days and 2 weeks postpartum increased with the implementation of the WHO 10 Steps. Conversely, a 5-year follow-up study of hospital breastfeeding policies in the Philadelphia area failed to show a significant increase in mean initiation rate after implementation of the BFHI (4).
Although the ‘ever breastfed' rate in Arizona is higher (76.5%) than the national average (73.9%), the overall breastfeeding report card score (62.0/100) devised by the Centers for Disease Prevention and Control (CDC) to rank states on “how breastfeeding is being protected, promoted, and supported in each state using five outcome and nine process indicators” is slightly lower than the national average (63/100) (8). There are no hospitals within Arizona with the BFHI designation, a contributing factor to the low breastfeeding report card score. Other contributing factors to Arizona's low score are higher (36.7%) than national rates (25.6%) of formula supplementation and the low number of state health department positions (1.5) dedicated to breastfeeding compared to the national average (79.79) (8). Breastfeeding exclusivity rates in Arizona (29.7% at 3 months; 11.9% at 6 months) fall far below national public health goals (40% and 17% respectively) and slightly below actual national rates (33.1%; 13.6% respectively) (8). A contributing factor to these low exclusivity rates may be the high rates of supplementation occurring in the hospitals and/or the high proportion of Latina women giving birth within the state (44%) (18), who often will not provide colostrum to their infants and begin breastfeeding after leaving the hospital; low exclusivity rates are frequently reported in this population (19, 20). In addition, pockets of much lower breastfeeding initiation rates also occur, especially in African American (28%) and indigenous (30%) women (21). However, because of the proportionally low numbers these women, population level data about their breastfeeding patterns have not been measured; the best source of information on these rates is data from the Women, Infants and Children's Supplemental Nutrition (WIC) public assistance programs.
Public health efforts to improve exclusive breastfeeding in Maricopa County have predominately driven by the state and county WIC public assistant programs that have a federal mandate to deliver nutrition information, education and food subsidies. Over the past 10 years, the WIC programs locally and nationally have made increasingly effective strides in promoting breastfeeding and supporting breastfeeding families. In Arizona, efforts have included peer support counselor programs, yearly mandatory staff training, and direct counseling with an International Certified Lactation Consultant (IBCLC) when available (22).
In Arizona, breastfeeding initiation rates have been increasing; however, looking a bit closer reveals these rates drop off dramatically in the early postpartum period and professional breastfeeding supports are below national levels. How hospital practices contribute to these outcomes is unclear. Hospital practices are heavily regulated and driven by economic concerns; until recently implementing supportive breastfeeding practices has been the result of internal institutional decision-making with each hospital determining policies and processes. Promoting and supporting breastfeeding families is a public health priority depending on these individual institutional practices. Community-level analysis is the only way to situate patterns in hospitals' implementation of supportive breastfeeding practices into the broader public health context. The aims of this investigation are to (1) describe the existing supportive hospital breastfeeding practices in a major urban region and (2) determine if supportive hospital breastfeeding practices are influenced by hospital characteristics.
METHOD
Design
A cross-sectional self-report telephone survey was conducted between July 2009 and March 2010, as part of a larger study aimed at describing available community-based lactation resources and associated breastfeeding rates within Maricopa County, Arizona (USA). Community- level data does not exist on breastfeeding supportive hospital practices in Maricopa County. This descriptive study design was chosen to begin to build an evidence-base about community-level breastfeeding practices and to inform program planners and policy makers.
Setting
Maricopa County, Arizona is located within a desert valley bordered by mountains on all sides; it includes the city of Phoenix and surrounding suburban communities. This major urban county is the fourth largest in the US (> 4 million people) (23). It is ethnically and socioeconomically diverse: Caucasian (58.8%), Latino (31%), African American (4.9%), Asian (3%), and indigenous peoples (2.2%). For citizens earning a household income equal to or less than 150% of the predetermined poverty threshold (i.e., $38,685 for a household of 4), state subsidized health care is available. Approximately, 52% of all Arizona births are paid for using public (government) funds, highlighting the large proportion of low income residents within the state (18). Otherwise, the US healthcare system is privatized with health care costs paid by third- party insurance providers.
Sample
All hospitals with maternity services (N = 21) in Maricopa County were identified using publicly available information. The person(s) identified as responsible for lactation services at each hospital was contacted and asked if study information could be sent for their consideration and for them to discuss participation in this study with their supervisors. A follow-up phone was scheduled to answer any questions that potential participants had and to ask if they would participate in this study. The response rate was 100%. Participants, who completed the telephone survey, were 15 registered nurses (RN) with IBCLC credential, 4 perinatal RNs, 1 registered dietitian and 1 IBCLC credentialed non-licensed staff. Two nurse managers, who did not provide direct breastfeeding services, self-selected to complete the survey.
Data collection [T3]
Approval from the Arizona State University Institutional Review Board Human Subjects Committee was obtained prior to data collection. Informed consent was verbal and occurred prior to data collection. Each institution was given a code number and identifying information delinked with the survey data to maintain confidentiality and minimize potential researcher bias. All surveys were completed by one member of the research team to maximize consistency in data collection. Follow-up phone calls were done by the same researcher to clarify ambiguous information and to complete missing data. All data are kept securely locked within the principal investigators office.
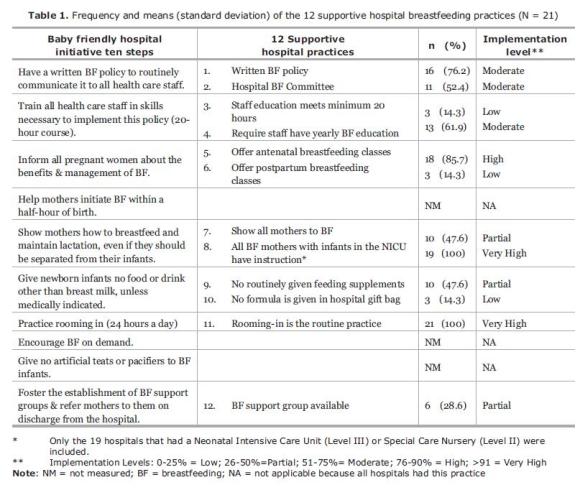
Supportive breastfeeding practices: Supportive breastfeeding practices were defined as 12 practices based on the well researched WHO Baby Friendly Hospital Initiative (BFHI) Ten Steps (listed on Table 1), which has become the ‘gold standard' for supportive hospital practices (6, 8, 24-27).
Participants answered yes or no to 12 questions, one about each of these practices. These 12 questions did not always mirror each of the BFHI Ten Steps exactly, which often contain more than one practice element in each step. Instead, survey questions reflected only one supportive practice element. Additionally, data were not collected on 3 (i.e., help mothers initiate breastfeeding within 30 minutes of birth, encourage breastfeeding on demand, and give no artificial teats or pacifiers to breastfeeding infants) of the BFHI Ten Steps due to the difficulty of obtaining accurate information about these practices on a verbal self report survey. Data needed to determine if these 3 supportive practices are not routinely collected by the surveyed hospitals, making any response to questions about these practices only guesses.
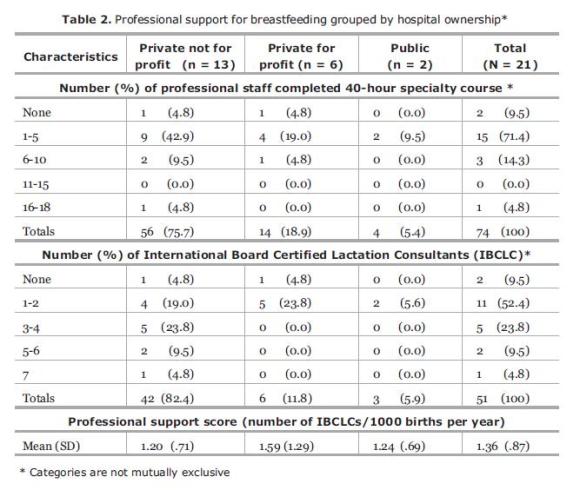
Hospital characteristics: Based on previous studies, data about hospital characteristics associated with breastfeeding practices [e.g., professional breastfeeding services available , institutional ownership status, number of births per year , percentage of births paid for by public funds and the level of care provided by the hospital (4)] were collected from public records or from participants. According to the CDC and other researchers, the professional breastfeeding support available to patients and maternity staff affects the quality of lactation services provided (8, 28). Professional support has been operationalized by the CDC as number of IBCLCs per 1000 live births (8). The number of births per year occurring in each of the 21 hospitals during 2009 was determined using Arizona State Department of Health data (18). Due to the high proportion of births within the County paid for by public funds, data were collected on this variable, as well. The number of IBCLCs, who provided direct lactation services (counseling and/or education) at each hospital, was provided by the participants. In addition, they provided the number of maternity nursing staff who had completed (at any time) either a local or national 40-hour lactation education course. These 2 variables were not mutually exclusive; IBCLCs who completed a 40-hour course were included in both categories, as it was not feasible to obtain more specific information from participants.
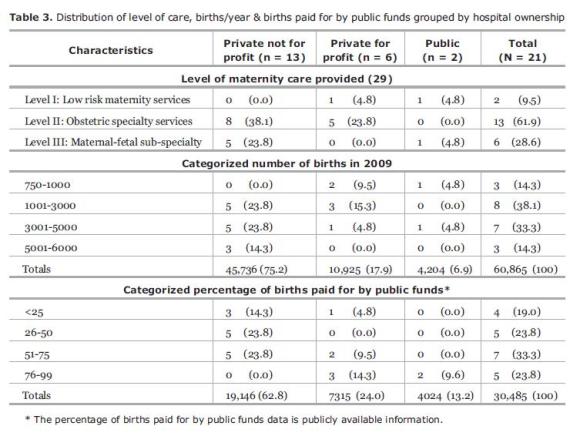
A few researchers have suggested that differences may exist among public and privately owned hospitals that affect implementation of supportive breastfeeding practices (5, 15). Four ownership categories were identified; public (funded by the federal government or by Maricopa County), private not-for-profit hospitals and private for-profit hospitals. Data concerning privately owned hospitals' legal status of a ‘for-profit' business or a ‘not-for-profit' service organization is public information. This variable was chosen because it has not been studied within the current context and it might affect supportive breastfeeding practices.
Level of maternity care services provided by a hospital refers to the categorization of hospitals according to the perinatal services provided, which is determined by a non-governmental organization: (1) Level I hospitals provide basic care for low-risk obstetrical patients and newborns, including caesarian sections, for 36 weeks gestation and greater; (2) Level II hospitals provide specialty care for low-risk and selected high-risk obstetrical and newborn patients from 32 weeks gestation; and (3) Level III hospitals provide intensive care services, as well as, all levels of obstetrical and neonatal care for all gestational ages (29).
Data analysis
Aim 1: The descriptive analysis of supportive breastfeeding practices included the frequency distribution along with the means and standard deviations of each of the 12 supportive breastfeeding practices. Using a strategy common in the literature (30), a variable of the level of implementation for each supportive practice was created categorizing the percentage of hospitals implementing each supportive practice: low (0-25%), partial (26-50%), moderate (51-75%), high (76-90%) or very high (91-100%) was created. Similar to other community-level studies (5, 15, 31), the supportive practices were summed for each hospital creating a ‘Supportive Breastfeeding Practices Score' (SBPS) for each institution.
Aim 2: Descriptive analysis of the hospital characteristics included frequency distribution of categorical variables, and means and standard deviations of continuous variables (number of births per hospital, births paid for by public funds, number of staff with specialized lactation education and number of IBCLC). The distribution of hospital characteristics were then grouped according the hospitals' ownership category. The national breastfeeding report card process outcome of number of IBCLCs per 1000 live births (Professional Support Score) was calculated for each hospital, creating a score that could be compared to national and state ‘Professional Support Scores'(PSS) (8). Means and standard deviations of the PSS were calculated for each hospital ownership category.
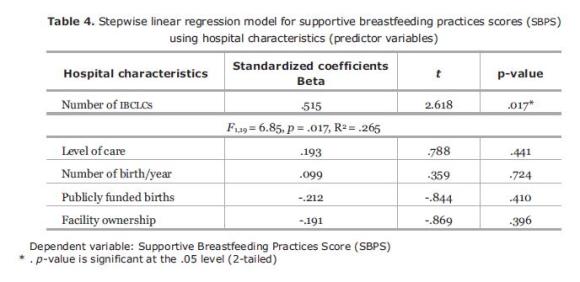
Stepwise linear regression was conducted to determine if hospital characteristics (predictor variables) significantly predicted SBPS (dependent variable). A stepwise method was chosen to draw the best-fit regression model given small number of predictors and this exploratory research. All of predictor variables (level of care, number of birth per year, births paid for by public funds, number of IBCLCs, and facility ownership) were entered simultaneously. The R2 was used rather than an adjusted R2 because the number of hospital characteristics entered in regression model was small (32). In addition, correlation coefficients using Pearson r were calculated to determine relationships between SBPS and hospital characteristics variables. The significance level was set at the .05 level. All data analyses were performed using SPSS (version 18) (33).
RESULTS
Aim 1: The total number of the 12 supportive breastfeeding practices (SBPS) implemented across hospitals varied considerably ranging between 5 and 10 with a mean of 7.42 (SD = 1.53). Two of the supportive breastfeeding practices–rooming-in and instructing breastfeeding mothers who have infants in the neonatal special care or intensive care unit–were standard practice (Table 1). Three support practices were ranked at the low level each having only 14.3% of the hospitals implementing these practices.
Aim 2: Characteristics of the professional support offered by publicly and privately owned hospitals varied considerably (Table 2). The trend across ownership categories was similar for professional staff that completed a 40-hours specialty course and the number of IBCLCs. The six for-profit private hospitals had the highest mean PSS; it exceeded the mean PSS reported by the CDC for Arizona state but fell far short of the national mean PSS. The other mean PSS for hospitals in Maricopa County did not mirror the state score.
Other hospital characteristics also differed based on hospital ownership (Table 3), with the 13 not-for-profit private hospitals serving the greatest number of women receiving publically subsidized care but this was 41.9% of their total number of births. Both publicly funded hospitals served far higher percentage (95.7%) of women receiving public assistance. Three of the 6 for-profit hospitals also provided care to high percentage of women receiving public assistance, although fewer women gave birth in these institutions. In 2009, the number of births occurring varied by institution from 750 at a public hospital to 5769 at a for-profit hospital. The majority (61.9%) of hospitals in this sample provided Level II maternity services.
Using the stepwise method, a significant model emerged (F1,19 = 6.85, p = .017, R2 = .265). Number of IBCLCs was the only predictor of supportive practice; 26.5% of the variance in the SBPS was explained uniquely by the number of IBCLCs (Table 4). We also sought residuals of the model to determine the difference between the observed values and those predicted by the regression equation. Standardized residuals indicate no outliers based on 3 standard deviations are identified by casewise diagnostics.
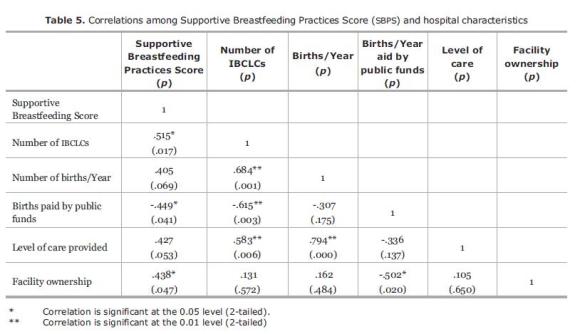
As shown in Table 5, SBPS was positively correlated with number of IBCLCs (r = .515) demonstrating that the higher number of IBCLCs employed by a hospital the greater number of supportive breastfeeding practices occurring in that hospital. A positive correlation occurred between SBPS and facility ownership (r = .438), demonstrating that private facilities were more likely to have higher SBPS. There were a significant negative correlation between SBPS and the births paid for by public funds (r = -.449), demonstrating that higher SBPS occur at hospitals that have fewer births paid for by public funds. All hospital characteristics were significantly correlated with the number of IBCLCs, except number of births/ year.
DISCUSSION
To improve the health of our children, breastfeeding promotion and support must occur on many social and political levels. Improving the quality of breastfeeding support practices in hospitals is only one of many strategies to accomplish this goal. By examining hospital breastfeeding support practices across Maricopa County a community-level picture of the similarities and differences in the type and amount of these supports available to childbearing women was possible. Although this cross-sectional view is by its nature temporal, it is the first attempt in Arizona to view hospital breastfeeding support practices in a more comprehensive context, which has public health implications for publicly funded program planning and policy development. This study was an initial and exploratory effort aimed at informing larger and more in-depth research into the issues suggested by the findings.
The descriptive analysis of the breastfeeding supportive practices (Aim 1) illustrated the wide variations in the number and types of practices present among the surveyed hospitals. These wide variations have been found by other researchers surveying at the community, state and national levels (2, 6, 34). None of the hospitals met the BFHI standard; only one hospital implemented 83.2% of supportive practices. The reasons why hospitals in Maricopa County are not practicing evidence-based standards of care for breastfeeding mothers is unknown, highlighting the need for additional investigation.
Rooming-in and assisting breastfeeding mothers who have infants in an intensive or special care unit were the only two universally implemented supportive breastfeeding practices. Over the past ten years, rooming-in has become the standard of care in maternity units driven by consumer demand and hospital economics. The nature and quality of the assistance provided to breastfeeding mothers who have infants in intensive or special care nurseries was not assessed and it is well acknowledged that these mothers will need assistance (35); therefore, it is difficult to determine the usefulness of this finding beyond the need for further research.
Rosenberg et al. (17) found that having a hospital policy was the only step that was independently associated with breastfeeding rates: “Hospitals with comprehensive breastfeeding policies are likely to have better breastfeeding support services and better breastfeeding outcomes” (p. 110). It is surprising that only two-thirds of the hospitals had specific standards in place, given new national hospital accreditation standards that included specific breastfeeding related hospital outcome indicators (36).
Increases in exclusive breastfeeding rates have been associated with the level of maternity staff education in many studies worldwide (7, 17, 30, 35, 37). Although the private hospitals had many staff who had completed a 40-hour course in lactation management, overall most hospitals did not meet the minimum 20-hours of lactation education for all maternity nursing staff (38). This suggests that the level of care for breastfeeding mothers is dependent on who is providing care on a specific shift and will vary from person-to-person and shift-to-shift, which contributes to the lack of consistency often reported by postpartum women and which is required to meet the standard of care (17, 30). Many other researchers have found that the supportive practices associated with this step were among the least implemented (16, 17). The BFHI Step 2 requires all health care staff to be educated a minimum of 20 hours on lactation management; however in this study data were gathered on maternity nursing staff only.
A long contentious issue for proponents of BFHI is the free formula provided to hospitals and to mothers in the form of discharge gift bags (39). Implementing the Ten Steps requires that no supplementation be given to breastfed infants and no infant formula be distributed to mothers in gift bags (40). Unfortunately, both of these practices were widespread among the surveyed hospitals. This is not a new or an unusual finding (5, 16, 22, 30). Ten years ago researchers reported WIC participants in Arizona who had received gift bags containing formula from upon discharge from the hospital were significantly more likely to have shorter durations and less exclusive breastfeeding (22). The negative effects of providing early supplemental feedings on duration and exclusivity rates have been established by numerous studies, prompting national public health efforts to educate health professionals and to promote exclusive breastfeeding from birth (8). Obviously progress has been slow, raising questions about why practices have not changed when the evidence is clear. It is a simple question within a complex context, which remains to be answered.
Currently consumers of maternity care have no way to discern implementation of supportive breastfeeding practices independent of a hospital's advertising, expectant mothers have a lack of accurate information and the responsibility for determining if hospital practices are congruent with their preferences. Even in areas with hospitals that have had the baby-friendly certification, researchers have reported inconsistencies in maintaining these supportive practices (4, 16).
Examining the relationships among the five hospital characteristics and the total number of supportive breastfeeding practices (Aim 2) provided meaningful in-sights that extended previous understanding about community-level supportive practices in Maricopa County and suggested additional variables that researchers might want to consider when examining community-level practices. Facility ownership was used to categorize the remaining four hospital characteristics, which allowed differences in these variables to become clearer, particularly patterns related to distribution of births per year subsidized by public funds. A negative correlation existed between the number of IBCLCs employed by a hospital and the births paid for by public assistance. Additionally, facility ownership was positively correlated with the total number of supportive breastfeeding practices implemented in hospitals. Viewed together these results suggest perhaps that a different standard of breastfeeding support exists for women receiving public assistance. The possibility of 2-tiered practice standards needs further research, highlighting the importance of taking the broader community perspective when seeking to change practice.
The Professional Support Score (PSS) has been reported by the CDC as the single most important indicator of the level of supportive breastfeeding practices (8, 11). The PSS for hospitals in Maricopa County were lower than the national level (8). Although the private not-for-profit hospitals employed the greatest number of IBCLCs, they had the lowest PSS indicating the lowest ratio of IBCLCs to number of births. Only the private for-profit hospitals had PSS that were higher than the state PSS. Perhaps the for-profit hospitals are more concerned with offering services desired by higher income women, who tend to breastfeed more often. It is unclear how the ratio of IBCLCs is affected by health care costs and hospital budgets; however, a cost-benefit analysis would need to be done taking hospital ownership into consideration.
Importance of IBCLCs in affecting positive institutional changes in supportive breastfeeding practice was suggested by the significance of this variable in the regression model. In addition, it was further supported in the positive correlation with number of supportive breastfeeding practices. This is consistent with the findings of other researchers, who reported that number of staff available for teaching new mothers was significantly associated with hospitals that had implemented high levels of supportive practices (30, 41). IBCLCs are making a difference within the institutions where they work. Using results from CDC's Infant Feeding Study, researchers have suggested a few population-based guidelines (including the PSS) related to the adequacy of professional breastfeeding support services (8, 11). More specific recommendations about adequate professional lactation services for level III hospitals were reported by Manel and Manel (9). However, the question of what constitutes adequate professional support services for a community has not been sufficiently addressed.
Limitations
Self-report surveys have some inherent methodological weaknesses that limit generalizability, even when the complete population is surveyed. Every attempt was made to interview the person most knowledgeable about lactation practices; in most cases, this was an IBCLC. However, in a few instances, ‘gatekeepers' within institutions may have limited information that was shared or given politically correct answers. Some data collected from participants required gathering information from medical records, but most of the survey questions relied on participants' knowledge and understanding of the supportive breastfeeding practices in their hospital. No attempt was made to validate participants' responses beyond clarifications of incomplete data, which may have affected the accuracy of these data.
Although it was beyond the scope of this study to determine breastfeeding rates associated with the measured hospital practices, increasing the number of supportive breastfeeding practices within a hospital repeatedly has been associated with increases in breastfeeding rates (8, 17, 42, 43). Future studies are needed to link breastfeeding outcomes to specific supportive practices.
CONCLUSION
The findings of this study, while unique to the community studied, were consistent with a number of findings reported by other researchers around the globe. Consistent patterns have emerged in the research concerning the best practices for promoting and supporting successful breastfeeding. The significance of professional staff with the IBCLC credential in improving the quality of hospital breastfeeding support practices was supported and it suggests the creation of more formal standards for hospital lactation services need to be developed and implemented.
ACKNOWLEDGEMENTS
Authors would like to thank Jeanne Stanger, CNM for her assistance during the early stages of this manuscript. We would also like to express our appreciation to those who took time out of their busy work days to complete the surveys.
REFERENCES
(1) Chalmers B, Levitt C, Heaman M, O'Brien B, Sauve R, Kaczorowski J. Breastfeeding rates and hospital breastfeeding practices in Canada: a national survey of women. Birth. 2009; 36(2):122-132. [ Links ]
(2) Dodgson JE, Allard-Hale CJ, Bramscher A, Brown F, Duckett L. Adherence to the ten steps of the Baby-Friendly Hospital Initiative in Minnesota hospitals. Birth. 1999; 26(4):239-247. [ Links ]
(3) Duyan Çamurdan A, Özcan S, Yüksel D, Pasli F, Sahin F, Beyazova U. The effect of the baby-friendly hospital initiative on long-term breastfeeding. Int J Clin Pract. 2007; 61(8):1251-1255. [ Links ]
(4) Kovach AC. A 5-year follow-up study of hospital breastfeeding policies in the Philadelphia area: a comparison with the ten steps. J Hum Lact. 2002; 18(2):144-154. [ Links ]
(5) Merewood A, Mehta SD, Chamberlain LB, Philipp BL, Bauchner H. Breastfeeding rates in US baby-friendly hospitals: results of a national survey. Pediatrics. 2005; 116(3):628-634. [ Links ]
(6) Abrahams SW, Labbok MH. Exploring the impact of the Baby-Friendly Hospital Initiative on trends in exclusive breastfeeding. Int Breastfeed J. 2009; 4:6. [ Links ]
(7) Castrucci BC, Hoover KL, Lim S, Maus KC. A comparison of breastfeeding rates in an urban birth cohort among women delivering infants at hospitals that employ and do not employ lactation consultants. J Public health Manag Pract. 2006; 12(6):578-585. [ Links ]
(8) Centers for Disease Control and Prevention. Breastfeeding Report Card-United States, 2009. [internet] Atlanta:Centers for Disease Control; 2009 [May 13 2010]. Available from: http://www.cdc.gov/breastfeeding/data/reportcard/reportcard2009.htm [ Links ]
(9) Mannel R, Mannel RS. Staffing for hospital lactation programs: recommendations from a tertiary care teaching hospital. J Hum Lact. 2006; 22(4):409-417. [ Links ]
(10) Unicef. The Baby Friendly Hospital Iniatiative. [internet] Geneva: Unicef; 2009 [May 5 2010]. Available from: http://www.unicef.org/nutrition/files/BFHI_2009_s1.pdf. [ Links ]
(11) DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics. 2008; 122: 43-49. [ Links ]
(12) Declercq E, Labbok MH, Sakala C, O'Hara M. Hospital practices and women's likelihood of fulfilling their intention to exclusively breastfeed. Am J Public Health. 2009; 99 (5): 929-935. [ Links ]
(13) Chien L, Tai C, Chu K, Ko Y, Chiu Y. The number of Baby Friendly hospital practices experienced by mothers is positively associated with breastfeeding: a questionnaire survey. Int J Nurs Stud. 2007; 44(7):1138-1146. [ Links ]
(14) Hofvander Y. Breastfeeding and the Baby Friendly Hospitals Initiative (BFHI): organization, response and outcome in Sweden and other countries. Acta Paediatr. 2005; 94 (8):1012-1016. [ Links ]
(15) Merten S, Dratva J, Ackermann-Liebrich U. Do baby-friendly hospitals influence breastfeeding duration on a national level? Pediatrics. 2005; 116(5):702-708. [ Links ]
(16) De Araujo MFM, Schmitz BAS. Reassessment of baby-friendly hospitals in Brazil. J Hum Lact. 2007; 23 (3):246-252. [ Links ]
(17) Rosenberg KD, Stull JD, Adler MR, Kasehagen LJ, Crivelli-Kovach A. Impact of hospital policies on breastfeeding outcomes. Breastfeed Med. 2008; 3(2):110-116. [ Links ]
(18) Arizona Health Status and Vital Statistics [database on the Internet]. Arizona Department of Health. 2008 [cited 2010.]. Available from: http://www.azdhs.gov/plan/report/ahs/ahs2008/pdf/1b28.pdf. [ Links ]
(19) Gill SL. Breastfeeding by Hispanic women. JOGNN. 2009; 38(2):244-252. [ Links ]
(20). Newton KN, Chaudhuri J, Grossman X, Merewood A. Factors associated with exclusive breastfeeding among Latina women giving birth at an inner-city baby-friendly hospital. J Hum Lact. 2009; 25(1):28-33. [ Links ]
(21) Arizona Bureau of Women's and Children's Health. Women's and Children's Health Needs Assessment Data. In: Health BoWsaCs, editor. Phoenix: Arizona Department of Health; 2010. [ Links ]
(22) Haneuse S, Sciacca J, Ratliff M, Alexander D, Rivero ME. Factors influencing breastfeeding rates among Arizona WIC participants. Am J Health Behav. 2000; 24(4):243-53. [ Links ]
(23) State and County QuickFacts [database on the Internet]. US Census Bureau. 2009 [cited 2010.]. Available from: http://quickfacts.census.gov.ezproxy1.lib.asu.edu/qfd/states/04000.html. [ Links ]
(24) Barnes M. The Baby-Friendly Hospital Initiative: the challenge of implementing change. Birth. 2003; 12(3/4):63-8. [ Links ]
(25) Murray EK, Ricketts S, Dellaport J. Hospital practices that increase breastfeeding duration: results from a population-based study. Birth. 2007; 34(3):202-11. [ Links ]
(26) Perez-Escamilla R. Evidence based breastfeeding promotion: the Baby-Friendly Hospital Initiative. J Nutr. 2007; 137(2):484-7. [ Links ]
(27) Saadeh R, Arke J. Ten steps to successful breastfeeding: a summary of the rationale and scientific evidence. Birth. 1996; 23(3):154-60. [ Links ]
(28) Thurman SE, Allen PJ. Integrating lactation consultants into primary health care services: are lactation consultants affecting breastfeeding success?. Pediatr Nurs. 2008; 34(5): 419-425. [ Links ]
(29) Arizona Perinatal Trust. Certification of Perinatal Services. [Internet] [May 29 2010]. Available from: https://azperinatal.org/Certification.html. [ Links ]
(30) Grizzard TA, Bartick M, Nikolov M, Griffin BA, Lee KG. Policies and practices related to breastfeeding in Massachusetts: hospital implementation of the Ten Steps to Successful Breastfeeding. Matern Child health J. 2006; 10(3):247-263. [ Links ]
(31) Martens PJ, Phillips SJ, Cheang MS, Rosolowich V. How baby-friendly are Manitoba hospitals? The Provincial Infant Feeding Study. Can J Public Health. 2000; 91(1):51-57. [ Links ]
(32) Miles J, Shevlin M. Applying Regression and Correlation Thousand Oaks. CA: Sage Publications; 2001. [ Links ]
(33) SPSS. (Statistical Software). 18 ed. Chicago IL: IBM; 2010. [ Links ]
(34) Tiedje LB. Toward evidence-based practice. Adherence to the ten steps of the Baby-Friendly Hospital Initiative in Minnesota hospitals. MCN Am J Matern Child Nurs. 2000; 25 (4):222. [ Links ]
(35) Castrucci BC, Hoover KL, Lim S, Maus KC. Availability of lactation counseling services influences breastfeeding among infants admitted to neonatal intensive care units. Am J Health Promot. 2007; 21(5):410-415. [ Links ]
(36) The Joint Commission. Specifications Manual for the Joint Commission National Quality Core Measurements (Contract No.: 2010A2). [Internet] [May 29 2010]. Available from: http://manual.jointcommission.org/releases/TJC2010A/ rsrc/Manual/TableOfContentsTJC/Perinatal_Care_v2010 A2.pdf [ Links ]
(37) Coutinho SB, de Lira PI, de Carvalho Lima M, Ashworth A. Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet. 2005; 366:1094-1100. [ Links ]
(38) World Health Organization, UNICEF. Baby-friendly Hospital Initiative: Revised, updated, and expanded for integrated care. Geneva: World Health Organization; 2009. [ Links ]
(39) Merewood A, Fonrose R, Singleton M, Grossman X, Navidi T, Cook JT, et al. From Maine to Mississippi: hospital distribution of formula sample packs along the Eastern Seaboard. Arch Pediatr Adolesc Med. 2008; 162(9):823-827. [ Links ]
(40) Merewood A, Philipp BL. Becoming baby-friendly: overcoming the issue of accepting free formula. J Hum Lact. 2000; 16(4):279-282. [ Links ]
(41) Grossman X, Chaudhuri J, Feldman-Winter L, Abrams J, Newton KN, Philipp BL, et al. Hospital Education in Lactation Practices (Project HELP): Does clinician education affect breastfeeding initiation and exclusivity in the hospital? Birth. 2009; 36(1):54-59. [ Links ]
(42) Merewood A, Patel B, Newton KN, MacAuley LP, Chamberlain LB, Francisco P, et al. Breastfeeding duration rates and factors affecting continued breastfeeding among infants born at an inner-city US baby-friendly hospital. J Hum Lact. 2007; 23(2):157-64. [ Links ]
(43) Philipp BL, Malone KL, Cimo S, Merewood A. Sustained breastfeeding rates at a US baby-friendly hospital. Pediatrics. 2003; 112(3):234-236. [ Links ]