Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Avances en Enfermería
versão impressa ISSN 0121-4500
av.enferm. vol.33 no.1 Bogotá jan./abr. 2015
https://doi.org/10.15446/av.enferm.v33n1.48670
http://dx.doi.org/10.15446/av.enferm.v33n1.48670
Anxiety and depression symptoms in family members of ICU patients
Síntomas de ansiedad y depresión en familiares de pacientes en la UCI
Sintomas de ansiedade e depressão em familiares de pacientes na UCI
Maria Kourti1, Efstathia Christofilou2, George Kallergis3
1 RN, BSc, MSc, PhD. Faculty of Nursing, University of Athens, Intensive Care Unit, "Laiko" General Hospital of Athens. Athens, Greece. e-mail: nursemak@yahoo.gr
2 RN, BSc, MSc. Head Nurse of Intensive Care Unit, "Laiko" General Hospital of Athens. Athens, Greece.
3 MD, PhD. Assistant Professor, Faculty of Nursing, University of Athens. Athens, Greece.
Fecha de recibido: 23/08/12 Fecha de aprobado: 15/12/2014
Abstract
Objective: This study investigated symptoms of anxiety and depression in relatives of patients admitted in the Intensive Care Unit and determined whether these symptoms were associated to the seriousness of the patients' condition.
Metodology: A total of 102 patients' relatives were surveyed during the study. They were given a self-report questionnaire in order to assess demographic data, anxiety and depression symptoms. The symptoms of anxiety and depression were evaluated with the Hospital Anxiety and Depression Scale (HADS). Patient's condition was evaluated with A.P.A.CH.E II Score.
Results: More than 60% of patients' relatives presented severe symptoms of anxiety and depression. No relation was found between symptoms of anxiety and depression of the relatives of patients and patients' condition of health. On the contrary, these feelings used to exist regardless of the seriousness of patient's condition.
Conclusions: The assessment of these patients is recommended in order serious problems of anxiety and depression to be prevented.
Descriptors: Anxiety; Depressive Disorder; Intensive Care Units; Visitors to Patients (source: DeCS BIREME).
Resumen
Objetivo: El presente estudio se propuso investigar los síntomas de ansiedad y depresión en familiares de pacientes que fueron admitidos en la Unidad de Cuidados Intensivos y se determinó si estos síntomas se asociaron con la gravedad de la condición del paciente.
Metodología: Durante este estudio se encuestó un total de 102 familiares de pacientes, a quienes se les solicitó diligenciar un cuestionario auto-administrado para estimar aspectos sociodemográficos y síntomas de ansiedad y depresión. Los síntomas de ansiedad y depresión fueron evaluados con la Hospital Anxiety and Depression Scale (HADS). La condición del paciente fue evaluada con el A.P.A.CH.E II Score.
Resultados: Más del 60% de los familiares encuestados presentaron síntomas severos de ansiedad y depresión. No se encontró relación entre los síntomas de ansiedad y depresión de los familiares de los pacientes y el estado de salud de éstos. Por el contrario, aquellas sensaciones solían darse con independencia de la gravedad de la condición del paciente.
Conclusiones: Se recomienda la evaluación de estos pacientes para evitar problemas serios de ansiedad y depresión.
Descriptores: Ansiedad; Trastorno Depresivo; Unidades de Cuidados Intensivos; Visitas a Pacientes (fuente: DeCS BIREME).
Resumo
Objetivo: O presente estudo pesquisou os sintomas de ansiedade e depressão em familiares de pacientes que foram admitidos na Unidade de Terapia Intensiva e se determinou se esses sintomas se associaram com a gravidade da condição do paciente.
Metodologia: Durante este estudo se inquiriu um total de 102 familiares de pacientes, a quem se solicitou diligenciar um questionário auto-administrado, para estimar aspectos sociodemográficos e sintomas de ansiedade e depressão. Os dados sobre sintomas de ansiedade e depressão foram processados usando a Hospital Anxiety and Depression Scale (HADS). A condição do paciente foi avaliada com o A.P.A.CH.E II Score.
Resultados: Mais de 60% dos familiares questionados apresentaram sintomas severos de ansiedade e depressão. Não se encontrou relação entre os sintomas de ansiedade e depressão dos familiares dos pacientes e o estado de saúde deles. Pelo contrário, essas sensações com frequência se apresentavam com independência da gravidade da condição do paciente.
Conclusões: Recomenda-se a avaliação destes pacientes para evitar problemas sérios de ansiedade e depressão.
Descritores: Ansiedade; Transtorno Depressivo; Unidades de Terapia Intensiva; Visitas a Pacientes (fonte: DeCS BIREME).
Background
It is generally accepted that hospitals are places where emotions of anxiety, depression and sometimes aggressiveness can be expressed both by health care professionals and patients or their relatives (1). It is also understood that patients who are admitted in specific wards of the hospital, such as Intensive Care Units and Operating Rooms, are more likely to develop these feelings. However, ICU is probably the only place where patients' relatives seem to suffer more, not only because of the critical ill's condition, but also because of the fact that relatives must represent the patient and, in some cases, may need to take a decision for him (2).
Researches have shown that in half of the cases, people who visit ICU patient and they are close to him/her have difficulties in understanding doctors' information about prognosis, diagnosis and results of the cure (3), so anxiety and depression symptoms may occur to those relatives quite often (4, 5). In both cases relatives make efforts to share with ICU staff the burden of decisions related to quality and sometimes length of life of their beloved persons (6).
Aim of this study was to examine the presence of anxiety and depression symptoms in relatives of ICU patients that admitted in the Intensive Care Unit of a General Public Hospital in Athens, Greece, and whether such feelings are connected to the critical ill's condition.
Methods
A total of 151 questionnaires were given to the family members of ICU patients from August 2008 to September 2010. Finally, 102 of them were enrolled in this study —62 females and 40 males—. The criteria for the participants were as follows: a) to have visited the ICU patient at least two times in a row (7); and b) that the patient to be intubated for 48 hours at least (8). HADS (Hospital Anxiety and Depression Scale) (9) was distributed to the family members of the patients, after visiting the patient and being informed about his condition from the doctor in charge.
Data collection occurred from August 2008 to September 2010, after being approved by the Review Board of the hospital where the study took place. Two measurements took place: The first one, 7-10 days from the admission of the patient in the ICU (10-12) and the second one, after 15-20 days from the admission —7-10 days after first measurement— (11). For each measurement, questionnaires were given to the same relative and always after doctors' information about patient's condition.
The supplementation of the questionnaires was anonymous and each one had a code number in order to be recoded and used for the purposes of the study. Relatives that completed the first questionnaire and their patient died between the two data collection point, were after excluded from the study. Patient's condition was evaluated with A.P.A.CH.E II (Acute Physiology And Chronic Health Evaluation II) score. The score was calculated for each patient before the delivery of the questionnaires to his relatives and relatives were unknown of this score. The higher the score was getting, the more the patient's condition was deteriorating.
We devised a questionnaire to obtain demographic information on age, gender, relationship between family member and patient —husband, wife, son, daughter, brother, sister, mother, father—, prior relationship with ICU as a family member, place of staying and frequency of communication with ICU patient. The questionnaire also included the Hospital Anxiety and Depression Scale (HADS), which presented high internal consistency; Cronbach's α cofficient was 0,91 —0,863 for anxiety and 0,855 for depression—. The validation of the scale in the Greek population is included in the study of Michopoulos et al. (13) and the Greek translation has been done by Mystakidou et al (14).
This scale consists of two subscales, being one for anxiety (HADS-Anxiety) and other one for depression (HADS-Depression). Each subscale has seven multiple choice questions. There are four answer choices for each question, each with a score that varies from 0 to 3. The total HADS score varies from 0 to 21 points —being 0 to 21 for anxiety and 0 to 21 for depression—. Interpretation of the HADS scores was performed according to the methodological reference adopted (9).
As such, a score between 0 and 7 was interpreted as no case of depression or anxiety, scores between 8 and 10, as a possible case and scores from 11 to 21, as a probable case. Possible means something that has a chance of being or happening and the word probable means something that can be proven or that appears to be true (15).
Statistical analysis of the data was performed with the use of the statistical program Statistical Package for Social Sciences (SPSS) Version 18.0. The sample characterization data were analyzed descriptively and independent t test and chi square test were used for the comparative analysis between variables. The adopted level of significance was < 0,05.
Results
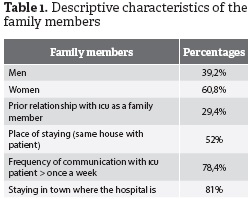
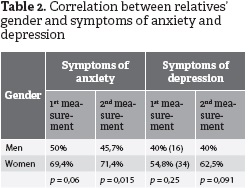
Demographic and clinical variables. Demographic characteristics of the participants are given in Table 1. From the statistical analysis with chi-square, tests occurred that, in both measurements, women seem to suffer more than men from anxiety symptoms (p < 0,05) but no correlation was found between gender and symptoms of depression (p > 0,05) (see Table 2).
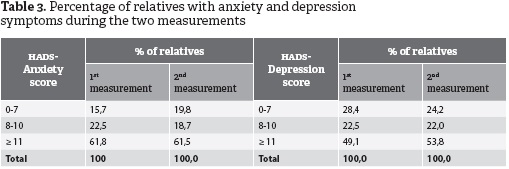
Generally, over 60% of the relatives in first measurement and almost half of them in the second measurement had strong anxiety and depression symptoms. Scores over 11 in subscales of Hospital Anxiety and Depression Scale (HADS) showed severe symptoms of these feelings (3), whose results are given in Table 3.
According to Table 3, during first measurement, it was observed that 22,5% relatives were possible cases and 61,8% were probable cases of anxiety. Moreover, according to the same table, 22,5% relatives were possible cases and 49,1% were probable cases of depression. From the same table, it can be also seen that during the second measurement, 18,7% possible cases of anxiety and 61,5% probable cases of anxiety were identified as well as 22% possible cases and 53,8% probable cases of depression.
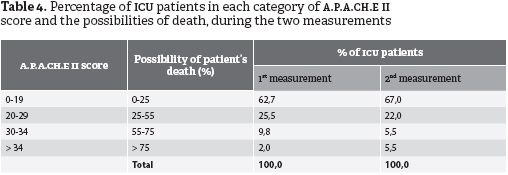
The A.P.A.CH.E II score for the majority of the ICU patients fluctuated between 0 and 19 and consequently the possibilities of death for those patients were smaller than 25% (16). The same results occurred from the second measurement too (see Table 4).
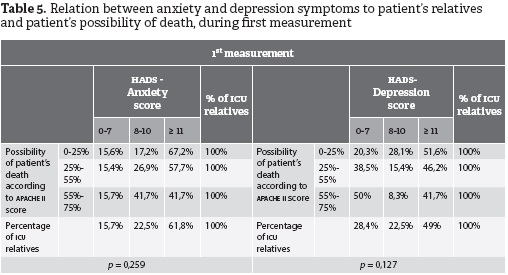
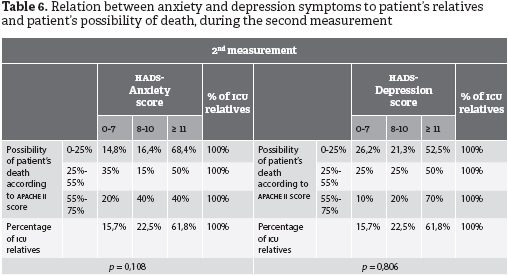
Mean scores of Hospital Anxiety and Depression Scale and possibilities of death, according to A.P.A.CH.E II score, were assessed by using independent-samples t test. No statistically a significant difference was observed to symptoms of anxiety and depression between relatives whose patient was more likely to live —lower A.P.A.CH.E II score— and to those whose patient was in a more critical condition (p > 0,05). In both measurements, the members of the patient's family seemed to feel very anxious and depressed either patient was doing better or not, according to chi square tests (see Table 5 and Table 6).
Discussion
In this study, we aimed to investigate the existence of anxiety and depression symptoms to family members of patients that were admitted in the Intensive Care Unit of a general hospital in Athens, Greece, and to find out whether such symptoms are associated to critical patient's condition. Consequently, mean anxiety and depression scores are very high to all relatives, regardless of patient's condition.
The HADS-Anxiety scores indicated that almost 62% of the participants faced severe symptoms of anxiety in both measurements. The same results also occurred in other studies (17-18), according to which 73% of the family members suffered from anxiety during the hospitalization of their beloved in ICU and after their discharge of it. In the same studies (17-18), depression symptoms occurred in a lower degree, about 35% of the relatives, comparative to those with anxiety symptoms. In our study, relatives with severe symptoms of depression were fewer comparative to relatives with symptoms of anxiety.
In another study (19), anxiety symptoms occurred in more than 70% of family members, while those with depression symptoms were not more than 40%. Prevalence in women —compared with men— was 69,4% (p = 0,06) in first measurement, and 71,4% in second one (p = 0,015) for symptoms of anxiety, while no correlation was found between symptoms of depression and gender. These prevalence were similar to those found earlier, as far as the symptoms of anxiety were concerned (20, 19, 6). In the same studies, among family members, women were the most likely to face severe symptoms of depression.
Results found in this study are similar to those found with the utilization of HADS, where the researchers found that 69,1% of family members had anxiety and 35,4% had depression (6). Maruiti et al. (15) found that 43,6% of relatives suffer from anxiety and 35,9% suffer from depression, by using the same scale in the family members of ICU patients, in the Intensive Care Unit of Hospital Albert Einstein in Sao Paulo, Brazil.
Anxiety can be identified as a feeling of apprehension and constitutes an individual experience, usually as a consequence of a new situation or experience. This situation or experience can be either pleasant, such as the birth of a child, or unpleasant such as the admission of a beloved person in the ICU (15). The relation between the appearance of anxiety and depression symptoms with unpleasant and stressful events was found in other studies too (6, 21). Depressive symptoms are associated with difficulties in sleep, loss of weight, reduced energy and difficulties to think or concentrate.
Patients' condition assessed with the A.P.A.CH.E II scale and scores varied from 0 to 19, meaning that the possibilities of death for those patients were lower than 25% (16). However, the A.P.A.CH.E II scale failed to correlate with symptoms of anxiety and depression in family members, indicating that these symptoms exist during the whole patient's staying in the ICU, regardless to the seriousness of the patient's condition. In another study (6), researchers used the Simplified Acute Physiology Score II (SAPS II), in order to evaluate patient's condition, and no correlation was found between SAPS II and symptoms of anxiety and depression to the relatives.
Consequently, it could be said that relatives of patients that admitted in an ICU, face severe symptoms of anxiety and depression (22-24, 5) during the entire hospitalization of the patient and the majority of these relatives needs further help from specialists in Psychology and Psychiatry. The nurses who work in the ICU and have direct contact with patients and relatives too (6, 25, 26) need to recognize these symptoms and adopt ways of minimize them.
All these symptoms can be transmitted from relatives to patients interfere in their health conditions and change their clinical situation (27). Holden et al. (28) have shown that development of relationships between critical care nurses and close relatives demands time and energy, but it can also help to reduce stress for all concerned. Physicians should also be committed to caring not only for the patients but for their families too and more studies establishing the clinical impact of anxiety and depression symptoms are necessary to be done (29).
References
(1) Carlet J, Garrouste M, Dumay MF, Diaw F, Guidet B, Timsit JF et al. Managing intensive care units: make LOVE, not war! J Crit Care. 2010 Jun;25(2):359.e9-359.e12. [ Links ]
(2) Davidson JE. Family-centered care: meeting the needs of patients' families and helping families adapt to critical illness. Crit Care Nurse. 2009 Jun;29(3):28-34. [ Links ]
(3) Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007 Feb;35(2):605-622. [ Links ]
(4) Gries CJ, Engelberg RA, Kross EK, Zatzick D, Nielsen EL, Downey L et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010 Feb;137(2):280-287. [ Links ]
(5) Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008 Jun;36(6):1722-1728. [ Links ]
(6) Schmidt M, Azoulay E. Having a loved one in the ICU: the forgotten family. Curr Opin Crit Care. 2012 Oct;18(5):540-547. [ Links ]
(7) Stricker KH, Kimberger O, Schmidlin K, Zwahlen M, Mohr U, Rothen HU. Family satisfaction in the intensive care unit: what makes the difference? Intens Care Med. 2009 Dec;35(12):2051-2059. [ Links ]
(8) Rothen HU, Stricker KH, Heyland DK. Family satisfaction with critical care: measurements and messages. Curr Opin Crit Care. 2010 Dec;16(6):623-631. [ Links ]
(9) Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361-370. [ Links ]
(10) Pillai L, Aigalikar S, Vishwasrao SM, Husainy SM. Can we predict intensive care relatives at risk for posttraumatic stress disorder? Indian J Crit Care Med. 2010;14(2):83-87. [ Links ]
(11) Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008 Nov;23(11):1871-1876. [ Links ]
(12) Pillai LV, Ambike D, Husainy S, Vaidya N, Kulkarni SD, Aigolikar S. The prevalence of post-traumatic stress disorder symptoms in relatives of severe trauma patients admitted to the intensive care unit. Indian J Crit Care Med. 2006;10(3):181-186. [ Links ]
(13) Michopoulos I, Douzenis A, Kalkavoura C, Christodoulou C, Michalopoulou P, Kalemi G et al. Hospital Anxiety and Depression Scale (HADS): validation in a Greek general hospital sample. Ann Gen Psychiatry. 2008 Mar;7:4. [ Links ]
(14) Mystakidou K, Tsilika E, Parpa E, Galanos A, Vlahos L. Psychometric properties of the Impact of Event Scale in Greek cancer patients. J Pain Symptom Manage. 2007 Apr;33(4):455-461. [ Links ]
(15) Maruiti MR, Galdenao LE, Dias OGF. Anxiety and depressions in relatives of patients admitted in intensive care units. Acta Paul Enferm. 2008;21(4):636-642. [ Links ]
(16) Bian Y, Zhang P, Xiong Y, Xu F, Zhu S, Tang Z, Xue Z. Application of the APACHE II score to assess the condition of patients with critical neurological diseases. Acta Neurol Belg. 2015 Jan;[Epub ahead of print]. [ Links ]
(17) Azoulay E, Pochard F, Chevret S, Adrie C, Annane D, Bleichner G et al. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med. 2004 Sep;32(9):1832-1838. [ Links ]
(18) Azoulay E, Chaize M, Kentish-Barnes N. Involvement of ICU families in decisions: fine-tuning the partnership. Ann Intensive Care. 2014 Nov;4:37. [ Links ]
(19) Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005 Mar;20(1):90-96. [ Links ]
(20) Paparrigopoulos T, Melissaki A, Efthymiou A, Tsekou H, Vadala C, Pavlou E et al. Short-term psychological impact on family members of intensive care unit patients. J Psychosom Res. 2006 Nov;61(5):719-722. [ Links ]
(21) Brand A, Leor S, Apter A, Fennig S. The impact of comorbid depressive and anxiety disorders on severity of anorexia nervosa in adolescent girls. J Nerv Ment Dis. 2014 Oct;202(10):759-762. [ Links ]
(22) Płaszewska L, Gazda D. Emotional reactions and needs of family members of ICU patients. Anaesthesiol Intensive Ther. 2012;44(3):145-149. [ Links ]
(23) Carlet J, Garrouste M. Welcome to our intensive care unit, make yourself at home! Crit Care Med. 2009 Jul;37(7):2313-2314. [ Links ]
(24) Carson SS, Vu M, Danis M, Camhi SL, Scheunemann LP, Cox CE et al. Development and validation of a printed information brochure for families of chronically ill patients. Crit Care Med. 2012 Jan;40(1):73-78. [ Links ]
(25) Goethals S, Dierckx de Casterlé B, Gastmans C. Nurses' decision-making in cases of physical restraint: a synthesis of qualitative evidence. J Adv Nurs. 2012 Jun;68(6):1198-1210. [ Links ]
(26) Peigne V, Chaize M, Falissard B, Kentish N, Rusinova K, Megarbane B et al. Important questions asked by family members of intensive care unit patients. Crit Care Med. 2011 Jun;39(6):1365-1371. [ Links ]
(27) Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007 Feb;356(5):469-478. [ Links ]
(28) Adams A, Mannix T, Harrington A. Nurses' communication with families in the intensive care unit: a literature review. Nurs Crit Care. 2015 Jan;[Epub ahead of print]. [ Links ]
(29) Kross EK, Engelberg RA, Gries CJ, Nielsen EL, Zatzick D, Curtis JR. ICU care associated with symptoms of depression and posttraumatic stress disorder among family members of patients who die in the ICU. Chest. 2011;139(4):795-801. [ Links ]