Introduction
THE SARS-COV-2 (COVID-19) pandemic of 2020 forced many people into physically isolating and socially distancing themselves from others (Killgore et al., 2020). Developing an understanding of the psychological effects of the COVID-19 pandemic can help psychologists to prevent mental health problems in similar situations both during and after the isolation period has ended (Huremovic, 2019).
Quarantine involves the temporary seclusion of a person who has been exposed to a contagious disease; this is a historical control strategy for maintaining public health (Dénes & Gumel, 2019). Social isolation, in contrast, is defined as 'the inadequate quality and quantity of social relations with other people at the different levels where human interaction takes place' (Zavaleta et al., 2017, p. 370). In the present article, we use the term isolation to refer to people undergoing the social distancing measures proposed by various governments as a way of slowing the spread of COVID-19.
The psychological impact of social isolation, social distancing, and quarantine has been the object of various studies in the past. Leigh-Hunt et al. (2017) reveal that isolation is associated with poor mental and physical health. Santini et al. (2020) found correlations between isolation in elderly people and symptoms of depression and anxiety. Other studies focusing on mental health show that isolated people experienced anxiety and fear of contagion during a Middle East Respiratory Syndrome (MERS) epidemic. Some of the factors relating to fear during social isolation were: the sense that the state was not protecting its citizens, worry about the national economy, and the lack of control in different situations (Jeong et al., 2016; Travaglino et al., 2020).
In a systematic review, Brooks et al. (2020) found that most studies reported negative and long-lasting psychological effects, including posttraumatic stress disorder (PTSD) symptoms, confusion, anger, frustration, boredom, financial loss, and stigma. Yoon et al. (2016) found that many people who were in quarantine during a MERS outbreak in Korea experienced psychological issues and required mental health support even after the quarantine had ended. Finally, Huremovic, (2019) suggests that quarantine situations can cause complications in various aspects of health in quarantined patients, ranging from delirium to PTSD and cognitive impairment to adjustment disorder.
The COVID-19 infections quickly escalated and achieved global proportions (World Health Organisation [WHO], 2022). However, due to previous experience during 'smaller' epidemics, psychologists planned treatments and pressed for measures to ensure psychological help for people with the COVID-19 disease, in particular, for patients with existing mental health problems. These measures include policy-making and public health programmes (Cénat et al., 2020; Duan & Zhu, 2020; Leigh-Hunt et al., 2017). Efforts to prevent mental health problems due to isolation become increasingly important when managing the aggravation of existing conditions in those previously diagnosed with mental health problems or in special population groups as elderly people (Huremovic, 2019).
In this study we aimed to map different psychological symptoms related to mental problems and feelings (both problematic and not) experienced during the isolation period due to COVID-19. The group of symptoms and feelings examined correspond to those found in the literature. These include stress, worry, boredom, restlessness, anguish, sadness, tiredness, sleeping disorders, confusion, feeling of carrying a burden, anger, loneliness, feeling mentally ill, not being able to form thoughts, foggy mind, hopelessness, feeling physically ill, bad memory, communication troubles, and feelings of guilt. If problematic symptoms and feelings occur, it is necessary to map their frequency so that mental health practitioners can be informed and create programmes for treating them. In addition, we inquired about positive affect as a means of controlling the bias towards negative affect and clinical symptoms. Positive affect results from having time for the family, having time for oneself, having more time in general, feeling calmed, entertained, or happy.
Material and Methods
Design
The research was exploratory and aimed to map the frequency of different psychological symptoms and the feelings of people undergoing isolation due to COVID-19. As part of the explorative design, we inquired at a deeper level (using standardised scales) about depression and stress as the literature indicates the prevalence of these mental problems. The exploratory design was developed in a way that initial results and observations could be investigated progressively. This allowed us a better understanding of the data and ensured we were not measuring biases due to peripheral factors.
We used a cross-sectional design to inquire about the mental condition of people at a particular point in time during the isolation measures imposed by various governments to prevent the spread of COVID-19.
The data was pre-processed and then analysed using R and SPSS (see Appendix A for a reference to the data and code used in the analysis). We used descriptive statistics to depict the frequency of symptoms and feelings in the quarantined populations. Finally, based on the prevalence of findings, we used Chi-square analyses to investigate associations between variables and to assess possible sources of bias in the results.
For the Chi-square analysis, the null hypothesis was that the observed frequencies of PHQ-9 and the PSS-10 results in the categories of the independent variables (gender, age, education level, employment status, worries about losing jobs, financial worries, and worries about income), were not different from the expected frequencies (Ugoni & Walker, 1995). Cramer's V was calculated as an effect size measure and a significance level of a = .05 was assumed (See Appendix C and D).
Participants
Inclusion criteria: Anyone from the age of 18 years and above who could read and complete the survey could take part in the study. In addition, they had to comply with the informed consent request before taking the survey.
Exclusion criteria: People below 18 years old were not allowed to participate in the study as GDPR regulations and Colombian ethical regulations for research forbid data collection from underage people without parental consent. Participants not agreeing to give their informed consent were also excluded.
Sample
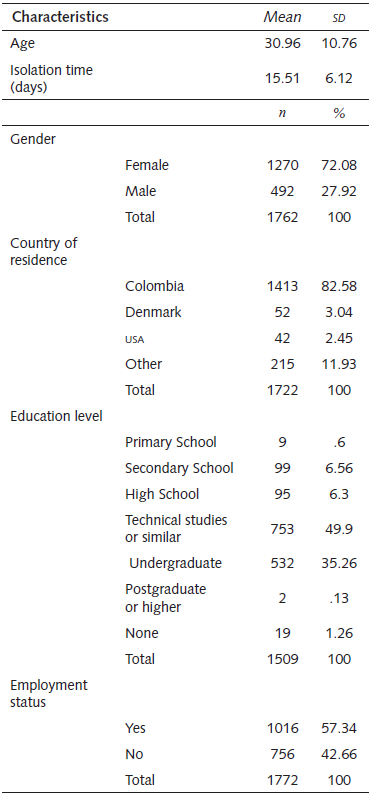
We gathered the data during a period of 15 days (30th of March to 13th of April 2020). A total of 1890 respondents completed the survey. From these participants, we discarded the data from 105 participants who did not correctly fill in all sections of the informed consent form or who stated they were younger than 18 years old. Our final sample consisted of N=1785 participants. A summary of the sociodemographic data is presented in Table 1.
Materials
We designed a survey inquiring about sociodemographic data (language -required before taking the survey-, gender, age, country of residence, education level, and employment) and seven topics that could affect people during the isolation period, including:
Measures taken by the government to prevent the spread of the virus.
Inquiries about the relationship between the work situation and mental health.
Compliance with the measures proposed by the government.
People who cohabit with the respondent.
Perception of COVID-19.
Whether COVID-19 has affected the health of the respondent or someone close to them.
Questions regarding current symptoms and feelings associated with mental health as indicated by the literature reviewed.
Although the greater part of the research focused on the symptoms and feelings that people had during isolation (topic 7), the other questions allowed us to test for possible biases affecting symptoms and feelings that were not directly related to the isolation.
In addition, we used standardised psychological scales to assess depression and stress. The Patient Health Questionnaire-9 (pHQ-9; Spitzer et al., 1999) is a self-report measure to assess the intensity of depressive symptoms during the last seven days. The sentence instruction was, 'since your isolation period started, how often have you been bothered by any of the following problems?' this was followed by items as 'Feeling down, depressed, or hopeless. The scale provides a total of nine items and a 4-point Likert type measurement (0 = Not at all-3 = Nearly every day). The severity levels of depressive symptoms that can be interpreted are no depression (0-4), mild depression (5-9), moderate depression (10-14), moderately severe depression (15-19), and severe depression. (20-27). It has a Cronbach's alpha of .89, and its test-retest reliability is high (.84) (Kroenke et al., 2001). The instructions for the PHQ-9 measurements can be found in Spitzer et al. (n.d.).
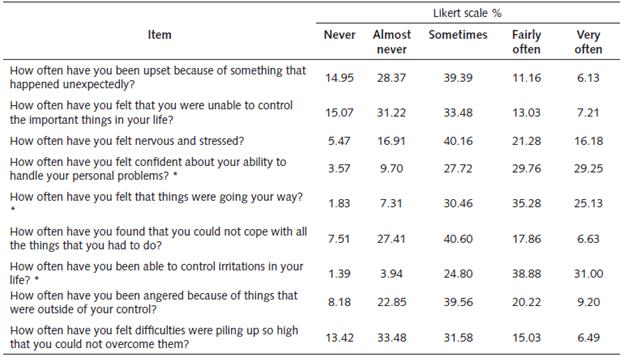
The Perceived Stress Scale (pss-10; Cohen et al., 1983) has 10 items to measure the degree to which one's life situations have been perceived as overloaded, unpredictable, and uncontrollable in the past month (e.g., 'How often have you been upset because of some-thing that happened unexpectedly?'). Participants answer each question on a 5-point Likert scale ranging from 0 (never) to 4 (very often). Internal reliability (Cronbach's alpha) ranges from .78 to .91 (Cohen, & Janicki-Deverts, 2012). We graded the results of the scale according to the age normative data provided by Cohen (1994) as follows: ages 18-29, M = 14.2, SD = 6.2; ages 30-44, M = 13.0, SD = 6.2; ages 45-54, M = 12.6, SD = 6.1; ages 55-64, M = 11.9, SD = 6.9; ages 65+, M = 12.0, SD = 6.3. We considered everything within the Mean plus/minus one SD (inclusive) to be normal. More than one SD above the Mean was coded as 'high stress' and less than one SD below the Mean was coded as 'low stress. The full survey can be found in Appendix B.
Procedure
The survey was distributed through the Sur-veyXact platform, which complies with the GENERAL DATA PROTECTION REGULATION (GDPR) requirements for the storage and protection of data. The survey was presented in English, Spanish, Danish, Italian, German, French, Hungarian, and Thai. After choosing a language, participants were presented with an informed consent request in their language. Participants could only proceed once they had accepted the terms and purposes of the research.
The survey was shared via social media, including Facebook, Twitter, and WhatsApp, via open calls and groups of interest.
Ethical considerations and data management
The research was considered as low risk according to the regulations proposed by the Directorate-General for Research Science, Economy, and Society (2010) and the Colombian regulations in the "Resolución Número 8430 de 1993" (Ministerio de Salud, 1993). This meant that answering some of the survey questions might create mild subjective discomfort in the participants. Participants were not paid.
Furthermore, the Bioethics Committee of the University of San Buenaventura evaluated and endorsed the execution of the research. The study was rated by the Committee as minimum risk. In addition, the study was conducted under the ethical principles of beneficence, nonmaleficence, fidelity, responsibility, integrity, justice, respect for people's rights, and dignity established for the American Psychological Association (APA, 2017) under the ethical avail of the Universidad San Buenaventura, Medellin (See appendix E). Observing the directions of the GDPR, we did not gather any sensitive data that would allow the recognition of participants on a personal basis. All data gathered were anonymous.
Results
Reliability of the survey
We conducted a unidimensional reliability analysis based on Cronbach's alpha and McDonald's omega to assess the internal consistency of the questions in the survey's Section G, as well as the reliability of the psychological scales used according to our sample. The results are summarised in Table 2.
Table 2 Summary of the reliability analysis of instruments
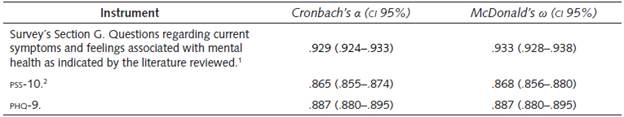
Seven items were coded reversed -see Appendix E
Four items were coded reversed -see Appendix E
Our analysis suggests that the internal consistency of our tool is good (0.8 ≤ α ≤ 0.9; 0.8 ≤ ω ≤ 0.9) for the standardised tests PSS-10 and PHQ-9, and excellent (α ≥ 0.9; ω ≥ 0.9) for the survey's section G. This allows us to ensure that the items are related and measure the same dimensions (Ravinder & Saraswathi, 2020).
Main findings
Based on H1, our main set of analyses focused on the section inquiring about the different symptoms and feelings people might experience when socially isolated. Our analysis of the data excluded the answers 'It doesn't apply' (accounted for .04% of the answers) as these could skew the data. We treated this data as NAS. Table 3 depicts the distribution of answers to the questions in groups, ordered by the extent to which people agreed with the various statements.
Table 3 Distribution of answers to the questions relating to feelings and symptoms during isolation
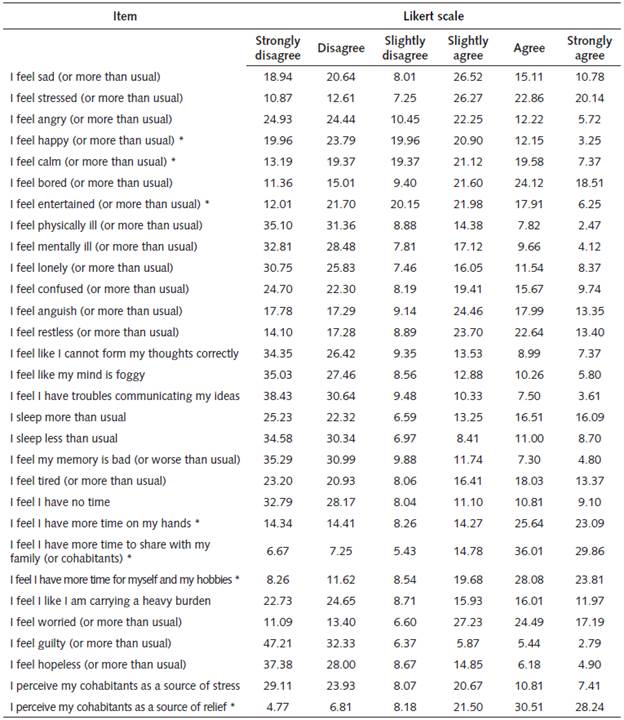
Note: *item was coded reversed.
On the one hand, people agreed that, since the quarantine started, they had more time to share with their family (81%), to spend on personal activities (71.6%), or in general (62.9%). Most of the participants reported that their cohabitants were a source of relief in the situation (80.2%). On the other hand, people also reported negative feelings or symptoms as worry (68.9%), stress (69.2%), and boredom (64.2%).
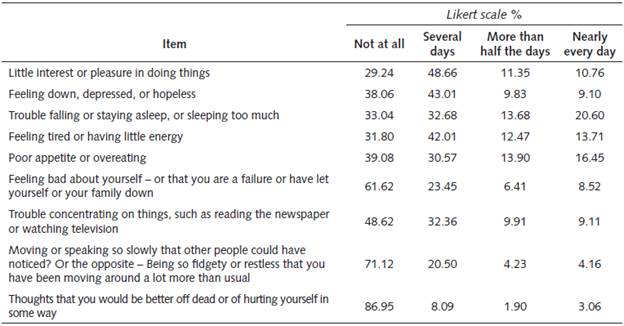
Analyses of psychological scales
Based on H2, we applied two standardised psychological scales, the PHQ-9 (Depression) and the PSS-10 (Stress).
As shown in Table 4, the two highest items of the scale were: item 3 (trouble falling or staying asleep or sleeping too much), and item 5 (poor appetite or overeating).
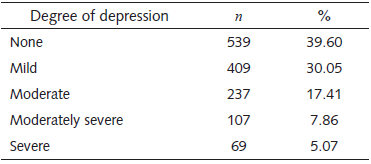
The largest group of participants did not present with depressive symptoms (39.6%), while only 5.07% of the isolated people presented with severe depression (see Table 5).
Table 5 Distribution of the population according to the degree of depression, as categorised by the normative data for the PHQ-9
As shown in Table 6, the four items with the highest scores were: item 7 (How often have you been able to control irritations in your life?), item 5 (How often have you felt that things were going your way?), and item 4 (How often have you felt confident about your ability to handle your personal problems?).
Ultimately, we obtained the distribution of stress for our sample as indicated in Table 7. This indicates that 70.78% of people had severe or moderately severe stress and 28.77% had normal stress. For the general sample, the score Mean = 21.99 and the SD = 4.41 (where the minimum score was 0 and the maximum score was 40).
Table 7 Distribution of the population according to the degree of stress as categorised by the normative data for the PSS-10
| Degree of stress | n | % |
| High stress | 957 | 70.78 |
| Normal | 389 | 28.77 |
| Low stress | 6 | .44 |
Note. High stress corresponds to a score of one SD above the mean. Low stress corresponds a score of one SD below the mean. Scores were corrected by age group according to the normative data (Cohen, 1994).
Follow-up analyses
To ensure that our results were not biased and were coherent with previous findings, we conducted a series of follow-up analyses. First, we conducted an exploratory factor analysis to find latent variables in the data based on the correlation structure of the items in the survey (Mair, 2018). Second, we conducted a series of association tests using Pearson's Chi-Squared (x2) for testing whether the results from the psychological scales were influenced by gender, age, education, employment, job or financial worries, or previous diagnoses of physical or mental health.
Exploratory factor analysis
We conducted an exploratory factor analysis to detect latent uncorrelated factors formed by questions related to particular problems or syndromes that could develop during a time of isolation (see Table 8). The extraction of factors was developed using the Minimum Residual method, and the number of factors was determined by the parallel method and by analysis of the sedimentation graph. We chose an Oblimin rotation as we expected to have overlapping factors (Field et al., 2012). The minimum load values were fixed at .4.
Table 8 Exploratory factor analysis of mental health questionnaire
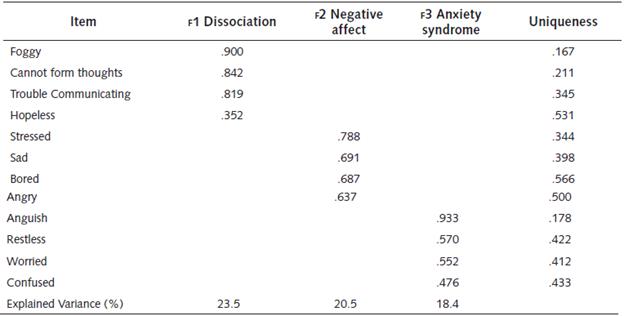
Note: 'Minimum residual' extraction method was used in combination with an 'Oblimin' rotation.
We found three factors associated with the psychological symptoms people reported suffering during isolation: we named them 'dissociation', 'negative affect, and 'anxiety syndrome. 'Dissociation' consisted of feelings of having a foggy mind, difficulty in forming thoughts correctly, trouble communicating ideas, and feelings ofhopelessness. 'Negative affect' included feelings ofstress, sadness, boredom, and anger. Anxiety syndrome' included feelings of anguish, restlessness, worry, and confusion. These three factors explained 62.4% of the variance. The internal consistency of each factor was analysed using Cronbach's alpha and McDonald's Omega: Dissociation (a = .88; co = .88), Negative affect (a=.82; co = .82), and Anxiety syndrome (a=.86; co =.86). Values greater than .7 were considered significant. As the values of alpha and omega were indistinguishable, we assumed compliance with the principle of tau equivalence.
In addition, we took the questions that did not have factor loadings above .4 into the three factors and found two more factor of questions, one relating to positive affect: people reporting feeling happy, entertained, and calmed; and a factor of questions about time management: people reporting feeling that they had more time, had time for themselves, and had time for their family. We analysed these questions separately as they are not symptoms related to mental health problems but have a different nature, this explains why they did not load into the three factors.
Association Between the Prevalence of Depression, Stress, and Other Participant Characteristics
Following the previous literature on isolation, we conducted Pearson's Chi-squared analysis to test for relationships between the results of the PHQ-9 and PSS-10 and the variables gender, age, education level, employment status, worries about losing jobs, financial worries, and worries about income. See Appendix C and D for a detailed description of the Chi-squared analyses.
Prevalence of depression was associated with gender (p < .001), age (p < .001), education level (p < .001), employment status (p < .001), job losing worries (p < .001), financial worries (p < .001), income worries (p < .001), and previous diagnoses ofphysical ( p = .025) and mental ( p < .001) health. Cramer's v analysis (v = .354) suggests that the relationship between previous mental health conditions and depression is strong, unlike the other variables.
Chi-squared results of associations between stress prevalence and gender and previous mental health conditions were significant (p < .05), although these associations were small (gender v = .089; mental health condition v = .120). Associations between prevalence of stress and age, education level, employment status, job losing worries, financial worries, income worries, and previous diagnoses of physical condition were not significant.
Discussion and Conclusions
From the findings of the study, we observed two implications for the mental health of people undergoing isolation measures due to the co-VID-19 pandemic. The first relates to the negative effects on mental health, expressed as high levels of depression, anxiety, stress, and dissociation. The second relates to the high degree of perceived social and family support, that is indicated by the high responses to items related to spending time with the family and the perception of being able to control difficult circumstances. High perceived social and family support suggest that people are embracing active coping mechanisms.
Negative Consequences of Isolation for Mental Health
The first important finding of the study was the high prevalence of depression among the participants (12.93%), characterised by disturbed sleep patterns and eating problems. These values are almost three times higher than the latest reference values provided by the 'Encuesta de Salud Mental Colombiana 2015' (Colombia 2015 National Mental Health Survey), that shows a prevalence of depression of 4.7% for the general population (Ministerio de Salud y Protección Social, 2015), while the WHO regards 4.4% as the average (WHO, 2017).
The finding of a high prevalence of depression is congruent with the results of other works on the impact of COVID-19 (Huang and Zhao, 2020; Ahmed et al, 2020). The findings of the current study also identified hopelessness among the symptoms in the exploratory factor analysis model, that are consistent with findings from previous epidemics as the Severe Acute Respiratory Syndrome (SARS) epidemic (Cheung et al., 2008).
Brooks et al. (2020) identified stressors during isolation that included the duration of the isolation period, fear of infection, frustration, boredom, and inadequate supplies and information. Stressors after the isolation period were also identified, amongst them financial concerns and stigma. Therefore, many concurrent vital stressors are added to the isolation period, aggravating the impact of isolation on the mental health of people (for an example see Kawohl & Nordt, 2020).
We found that stress was almost twice that of the reference values when the prevalence of stress in the current study (70.78%) was contrasted with the values provided by the 'Encuesta de Salud Mental Colombiana 2015' (Colombia 2015 National Mental Health Survey), suggesting an increase in the prevalence of stress of 40.2% (Ministerio de Salud y Protección Social, 2015). The high prevalence of stress in our survey is congruent with other research into the impact of COVID-19 and other epidemics (Wang et al., 2020; Lee et al., 2018) as well as PTSD symptoms (Huremovic, 2019).
The exploratory factor analysis enabled us to explain a variance in the results of 62.4% with three factors: dissociation, negative affect, and anxiety syndrome. Regarding dissociation (defined as the central mechanism for dissociative disorders and characterising a schizophrenic affect; American Psychiatric Association, 2013), previous studies suggest these dissociative symptoms tend to be closely related to stressful life events (Rocca et al., 2006), which were a central point during our research. The presence of dissociative symptoms is an indicator of severity, because 70% of people with these symptoms attempt to commit suicide, while self-harm behaviour is frequent (American Psychiatric Association, 2013).
Concerning the negative affect and anxiety syndromes: negative affect includes intense experiences leading to a wide range of negative emotions (e.g. depression, anxiety, worry, and anger) as defined by the alternative dimensional model of the DSM-V, based on the Five-factor model (American Psychiatric Association, 2013). Negative affect is homologous to neuroticism and describes how people can be overwhelmed by negative emotions as worry or insecurity (McCrae & Costa, 1997). In our study, participants reported feeling stressed (69%), worried (69%), bored (63%), restless (60%), anguished (56%), and sad (52%). Previous research with people undergoing isolation due to MERS found symptoms of anxiety in people undergoing quarantine. In addition, these symptoms persisted from four to six months after the isolation period ended (Jeong et al., 2016; Kroencke et al., 2020). Our findings highlight the relevance of neuroticism and negative affect as some of the mood risk factors during a pandemic.
Positive Aspects of Isolation in Relation to Mental Health
Concerning the stress measures in our study, 70% ofthe participants felt that they had control over their life issues, 60% said they felt that things were going their way, 59% said they could manage their problems. These results suggest that, regardless ofthe disruptive experience of isolation, many people feel that they could face stressful situations. These findings could be regarded as contradictory because, according to the scores of the PSS-10.70% of participants were experiencing a high degree ofstress. This implies that despite the connection between the stressors and the participants' mental health, a large proportion of them felt in control of their lives, irrespective of the possible psychological problems. It is important to perceive the control locus in establishing active coping mechanisms. Oros (2005, p. 95) explains this: "El locus de control funciona como un importante recurso de afrontamiento que tiene gran relevancia como factor predictivo de otras variables actitudinales, afectivas y comportamentales" (The control locus is an important coping resource of great relevance as a predictive factor for other attitudinal, affective, and behavioural variables).
In previous research, 'family time' has been found to act as a general coping support for parents, children, and adolescents alike (Hutchinson et al., 2006), a phenomenon that has been identified across several cultures (Tubbs et al., 2005). Positive family time has, for instance, been related to shared routines, including TV-time and recreation habits (Coyne et al., 2014), and the presence of parents who usually spend less time at home (Offer, 2013), and that it may continue unimpeded during isolation while other social activities are halted. As such, isolation with one's family may even provide a positive psychosocial disruption for some. Large scale research into the COVID-19 situation reveals that people were less worried about missing social opportunities than about the wellbeing of friends and family living far away, and that digital communication with loved ones was one of the more prominent de-stressing activities (Liebertoh et al., 2020; Travaglino et al., 2020). For instance, the role of the family in coping and resilience may also be digitally supported. These factors may cast some light on the role of family in our findings, as well as the nuances in them.
Unlike quarantine, social isolation allows people to be with their relatives and carry out personal activities. The main results of this research suggest that despite the disruptive nature of social isolation, family bonds and other activities as hobbies can be associated with balancing out the distress social isolation might generate.
To summarise, it is important to prevent the negative impacts of isolation and other concurrent stressors on mental health and to intervene during and after the pandemic as this can prevent serious psychological syndromes. It is relevant to promote the individual's resources for active coping regarding the multiple stressors associated with the pandemic and its public health consequences.
To achieve this, we suggest the use of tele-therapy, the clinical efficacy of which has been proven to treat depression (Deady et al., 2017; Kim et al., 2019; Massoudi et al., 2019; McCall et al., 2019) and stress (Glassman et al., 2019; McLean et al., 2020; Morland et al., 2020). Interventions directed towards coping should be adapted to account for the uncontrollability of stressors and the cultural preferences of people for different coping strategies.
Associations Between Mental Health and Other Factors
We found some association between the results of the psychological scales and the other variables. Although we did not test for direction of relationships, we found that many factors can be associated with depression (gender, age, education level, employment status, worries about losing the job, worries about financial status, worries about income, being diagnosed with a physical disease that puts you in a risk group for COVID-19, and being previously diagnosed with a mental condition).
Associations with depression have been well documented in the literature. Studies indicate that there is an increase of the prevalence of depression related to age, with depression being more prevalent during adolescence and in the elderly years (Akhtar-Danesh & Landeen, 2007; Stordal et al., 2003). Studies considering depression and gender suggest that there is an association between gender and depressive symptoms and depression diagnoses, with these being more prevalent in women than in men, and also varying according to age, where teenagers and elderly adults with a small social network are more vulnerable (Salk et al., 2017; Sonnenberg et al., 2012). Studies investigating education and depression demonstrate that education (understood as cultural capital and status) is linked to social and economic factors as job security, income, and social networks (ten Kate et al., 2017), factors that are often at risk due to isolation measures. Similarly, studies on socioeconomic stress and depression suggest that socioeconomic stress has a big influence on the prevalence of depression, stress, and anxiety; this prevalence increases when the stress is continuous over a period or when there is a lack of social support (Richardson et al., 2017; Viseu et al., 2018). Therefore, different socioeconomic aspects are linked with depression, but they are also interlinked with each other in a complex way that when even one is affected, it tends to affect the others.
Conversely, we found that a relatively small number of factors were associated with stress (gender, worries about losing the job, and being previously diagnosed with a mental condition). Studies of gender and stress suggest that male and female mammals react biopsychologically differently to stress, with a prevalence of females feeling more stressed relative to males (Handa & Chung, 2019; Verma et al., 2011). Additionally, an association between socioeconomic status and chronic stress has been identified (Baum et al., 1999).
Studies as those of Huremovic (2019) indicate how quarantine and isolation measures affect the mental health of people who have been previously diagnosed with psychological problems. These include an increase in symptoms due to the lack of social support or the disruption of routines, or problems emerging from a lack of medication or because of the interaction between medications.
We found that the association between depression and stress and other socioeconomic variables, including the diagnosis of a physical or mental disease, did not increase the number of people with symptoms of depression or stress in our sample. Although we cannot imply a causal relationship between mental health and isolation, our results (as well as previous research, e.g., Huremovic, 2019) suggest a relationship between isolation conditions and aggravated pre-existing vulnerabilities. This could imply higher frequency of depression and stress symptoms, leading to clinical manifestations. For instance, being isolated without a stable source of income could be a factor influencing stress, hopelessness, and depression.
Limitations of the Study
A possible selection bias was identified due to the use of snowball sampling, this implies that only people with access to ICT and the internet could complete the survey, leading to a possible lack of representation of the general population. The digital nature of the questionnaire and the sampling method could generate low participation by the elderly population.
Although the sample size presents good statistical power for data analysis, the generalisation of results should be limited to the age group 18 to 50 years. Similarly, although people from 40 different countries participated in the study, more than 80% were Colombian, so the generalisation of the findings to other countries should be done with caution. Most of the scales used were validated in Spanish, English, and Thai, but for other languages we made translations that would require validation for future research projects.
We suggest that future research should deepen the evaluation of predictors pre-quarantine for psychological impact, as previous psychiatric disorders, personality traits, perception of risk towards infectious diseases, and symptomatology of adaptive disorders, as well as stressful life events that could be added to the isolation situation.
Due to the cross-sectional characteristic of the data and the limitations noted above, no causal inferences should be made from these results. The pre-existence of psychopathologies and chronic conditions were not reported in the survey, and other confounders limit the scope of the findings.
Finally, isolation contributes to the development of problems associated with psychological and psychopathological conditions according to the prevalence of the symptomatology. The results of the study suggest that there is an impact on the mental health of participants undergoing isolation due to COVID-19. This impact is reflected in the high scores for depression, stress, anxiety, and dissociation, suggesting the necessity for prevention and intervention plans in the short-term to reduce dysphoric mood and its negative consequences. Prevention and intervention should be oriented towards the strengthening of social and family support, as well as building up active coping skills. Interventions should be adapted according to the cultural characteristics of the different countries and should account for the multiple simultaneous stressors associated with the isolation measures. This situation is critical for countries, health care institutions, and mental health professionals as they endeavour to prevent both physical and mental problems related to COVID-19.