Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Colombiana de Reumatología
Print version ISSN 0121-8123
Rev.Colomb.Reumatol. vol.18 no.2 Bogotá Apr./june 2011
PRESENTACIÓN DE CASO/CASE REPORT
2 Dermatopathologist, Universidad El Bosque.
Correspondencia: Yimy F. Medina. Correo electrónico: yimym@yahoo.com
Los autores declaran no presentar ningún conflicto de interés al momento de la redacción del manuscrito. No hubo ningún tipo de financiación.
Recibido: 22 de febrero de 2011. Aceptado: 24 de marzo de 2011
Summary
Lupus panniculitis or lupus profundus is a variant of lupus Erythematosus cutaneous that primarily affects subcutaneous tissue. Clinically, it is characterized by one or several firm subcutaneous nodules and/or plaques with or without overlying epidermal changes. It is reported to occur with a frequency of 2-3% in patients with Systemic Lupus Erythematosus (SLE). Between 10 and 50 percent of patients with lupus panniculitis will have or eventually develop Systemic Lupus Erythematosus. In nearly all cases there are deep, erythematosus plaques and nodules, and some of them ulcers, which usually involve the proximal extremities, trunk, breasts, buttocks, and face. These lesions may be tender and painful and frequently heal with atrophy and scaring, turning as a chronic condition and subsequently heal with disfigurement. We describe a patient who suffers from lupus panniculitis with no association to SLE symptoms and complicated by several progressive and disabling cutaneous lesions.
Key words: lupus panniculitis, dystrophic calcification, lupus erythematosus cutaneous.
Resumen
La paniculitis lúpica o también llamada lupus profundus es una variante del lupus eritematoso cutáneo que afecta el tejido celular subcutáneo. Se caracteriza clínicamente por uno o varios nódulos subcutáneos que son firmes y/o placa con o sin cambios epidérmicos. Se ha informado su frecuencia en 2% a 3% de casos de Lupus eritematoso sistémico. Entre el 10 al 50% de los casos de paniculitis lúpica va a desarrollar lupus eritematoso sistémico. En casi todos los casos hay placas eritematosas y/o nódulos que en algunos casos se ulceran y que usualmente están localizados en las áreas proximales de las extremidades, tronco, mamas, nalgas y la cara. Estas lesiones pueden ser clínicamente dolorosas y sensibles a la presión y frecuentemente cicatrizan con desfiguración del área circundante. Describimos un paciente que padece de paniculitis lúpica sin asociación de lupus eritematoso sistémico y que se complicó con varias lesiones cutáneas progresivas y discapacitantes.
Palabras clave: paniculitis lúpica, calcificación distrófica, lupus eritematoso cutáneo.
Introduction
Lupus panniculitis or lupus profundus is a variant of lupus Erythematosus cutaneous that primarily affects subcutaneous tissue. Clinically, it is characterized by one or several firm subcutaneous nodules and/or plaques with or without overlying epidermal changes. New nodules may appear while other may resolve slowly or may have long standing calcification. In nearly all cases there are deep, erythematosus plaques and nodules, and some of them ulcers, which usually involve the proximal extremities, trunk, breasts, buttocks, and face. Lesions may be tender and painful and frequently heal with atrophy and scars turning as a chronic condition and subsequently heal with disfigurement. Lupus panniculitis is reported to occur with a frequency of 2-3% in patients with Systemic Lupus Erythematosus (SLE)1-3. Conversely, between 10 and 50 percent of patients with lupus panniculitis will have or eventually develop systemic.
Lupus Erythematosus. This entity can manifest along with symptoms and laboratory of SLE or by itself. Approximately a quarter of patients with lupus panniculitis fulfilled the American College of Rheumatology criteria of SLE. Antinuclear antibodies (ANA) are positive in 65% of patients in low titters4.
Lupus panniculitis has been described associated to other entities and it is not limited to patients with SLE5. Prognosis is generally good, despite the association to systemic manifestations.
A panniculitis associated with a patchy lymphocytic infiltrate and deposition of mucin in the overlying dermis is suggestive of lupus panniculitis6.
We describe a patient who suffered from lupus panniculitis with no association to SLE symptoms and complicated by several progressive and disabling cutaneous lesions.
Case report
A 50 year-old woman, housekeeping and Hispanic race, had a diagnosis of lupus panniculitis at the age of 40, when she presented with symptoms of arthralgias, headache, and malaise, weight and hair loss. She did not state relevant past medical and family history except of fibromata of uterus and migraine.
In the past 8 years she developed multiple subcutaneous nodules which were seen first at elbows and then they spread to most regions of the body: Thorax, abdomen, upper, and lower extremities (figures 1, 2, 3, 4, 5 and 6).
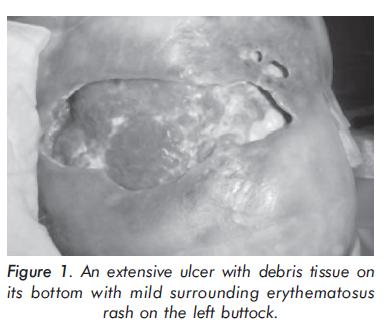
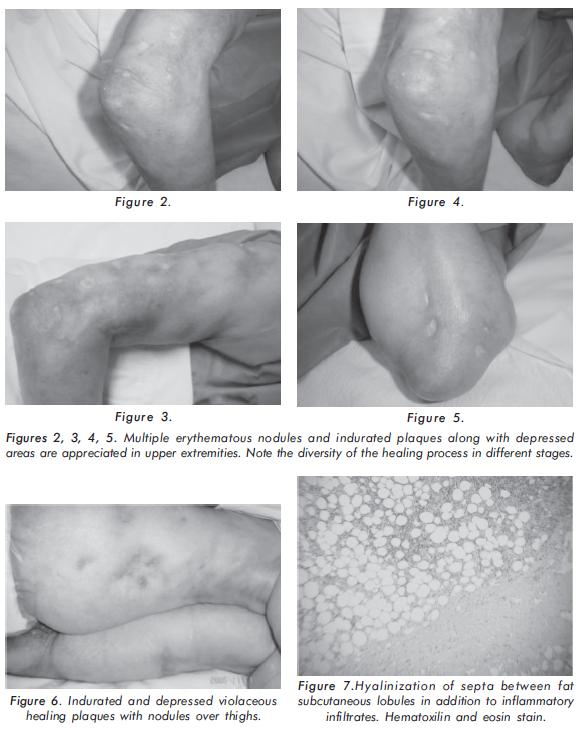
These lesions are characterized by being mobile, painful, hard or firm consistency, and cause fissures and ulcerations to the overlying skin with atrophy and depressions.
In the last years, the patient has undergone multiple hospitalizations due to several episodes of secondary infections and ulcerations on the nodules. It was obtained pseudomonas and staphylococcus species on cultures from one of the lesions and staphylococcus epidermidis on blood cultures requiring intravenous antibiotics. Physical examination was unremarkable except for an ulcer that reveals a debris tissue with mild surrounding erythematosus rash on the left buttock (figure 1) and several firm nodules of approximately 2 to 3 centimeters localized in thorax, abdomen, upper ((figures 2, 3, 4 and 5) and lower extremities (figure 6). These nodules were covered by a skin with depressions and lesions on different healing stages. Laboratory studies showed negative antinuclear antibodies (ANA), negative extractable nuclear antibodies that included anti La/SS-B, Ro/SS-A, Sm and RNP. Double stranded DNA was negative. Hemoglobin of 10.4 mg/dl, hematocrit 32%, and leucocytes 5000 x mm3 with lymphopenia, platelets 563000 x mm3, reactive C-protein 36ug/dl, erytrhosedimentation globular 22mm/h, calcium 10.8 mEq/ L. Proteins 5.9 g/L, albumin 2.4 g/L, globulins 3.5 g/L, alkaline phosphatase and transaminases were unremarkable. Levels of serum phosphorus were normal. Creatinine was n ormal and urinalysis showed: protein negative, bacteria +, 3 erythrocytes, 8-10 leucocytes. A urine culture was negative. Chest x-rays showed multiples soft tissue calcifications around axillary 's vessels. Radiographs of lower limbs and pelvis demonstrated calcifications in muscles and blood vessels. No bone lesions were found in these projections or in the skull x-rays. Thyroid gland and cortisol tests in blood were normal. Skin biopsy of ulcer on left buttock area revealed fat tissue with multiple chronic inflammatory fragments predominately lymphoid populations. Muscular tissue was appreciated with chronic inflammation and coexistence of multiple foci of dystrophic calcification and hyalinization of septa between fat subcutaneous lobules i n addition to inflammatory infiltrates (Figure 7). The Histopathologic diagnosis was lupus panniculitis and dystrophic calcifications.
Discussion
At the beginning of the 20th century (1912), almost simultaneously, two authors, Otto Kren7 and Oppenheim8 named a new entity called lupus profundus9. Lupus panniculitis or profundus diagnosis is made by primarily both clinical and histological findings. Usually, clinical picture is well established and one or several firm, asymptomatic, large subcutaneous nodules in patients with or without SLE is the most frequent clinical presentation10. It can lead to cutaneous and subcutaneous atrophy with occasional ulceration11 as seen in our patient. According to Winkelmann, lupus profundus histopathology lesions consist in an immflamatory process with perivascular and perianexial lymphoid infiltrate predominance on lymphoid conglomerates that suggests germinal centers in addition to collagen hyalinization, fibrinoid necrosis, mucinosis, perivasculitis and microcalcifications that are seen depending on the grade of calcification. It may be microcalcifications in fat or may be large cumulates of calcifications which compromise lobules or septa, and when are large enough it enable us to register them on plain radiographs12,13. It is uncommon to observe calcifications in lupus panniculitis lesions and when they are documenting is seen in old lesions as reported by Winkelmann in 1970 and Peter in 198914. In these cases, patients suffered from pain as happened in our patient who complained of pain on buttocks and thighs when sitting.
Calcification on deep soft tissues is rare and reports of cases are known in a renal transplantation and caciphylaxis which differ from our case. Other changes described as common findings are foci of lymphocytes with or without germinal centers, hyalinization of septa, fat lobules, and lymphocytes within the vessel walls or on the perivascular tissue15. Lesions will show variable degrees of calcification (mainly in old established lesions) or sometimes with intense calcium deposits on previously damage fat lobules with hyaline necrosis frequently limited by a collagenic pseudocapsule7.
Lesions have a chronic clinical course with remissions, recurrences and resolutions. They are commonly accompanied by large areas of depression and lypoatrophy16 as was seen in our patient.
Pathogenesis of calcium deposits is not clear but it is well documented that parathyroid hormone and vitamin D are not key factors. It was suggested that tissue alkaline phosphatase may activate extracellular pyrophosphatase (that normally inhibits calcium deposits) generating phosphates along with denaturized proteins of necrotic cells produced by inflammation of panniculitis17,18. This latter induces the production of phosphate calcium and calcareous deposits on lesions and is documented in dystrophic calcinosis19. These calcareous deposits damage the cytosolic sites producing cellular deposits and death. On elastic, collagenous and subcutaneous tissues, calcareous deposits may contribute to further calcareous deposition and worsening the cellular necrosis, an acid environment and interfering on the action of the calcification inhibitors and pyrophosfatases11,14,20.
This case not fulfils the American College of Rheumatology criteria for SLE. Therefore, Lupus panniculitis was diagnosed without any other disease manifestation. These lesions were progressive and caused a great burden in the patient's activities of daily living due to its sequels.
The treatment was challenging in this patient who had a poor outcome. She was on antimalarial agents and colchicine.
Management of patients with lupus panniculitis includes antimalarials that were used the first time by Thurson and Curtis9, 21, azathioprine22, cyclophosphamide14 and dapsone. Thalidomide was recommended in lupus panniculitis by Burrows, especially when it is associated to partial C4 deficiency23. It has been reported the management of older lesion calcifications with colchicine as was used in our patient24.
Some cases may respond to a combination of antimalarials such as hydroxychloroquine 200 mg and quinacrine 100 mg daily when a single drug is ineffective25. Other treatments include probenecid26, low doses of warfarin27,28 and diltiazem m18,29,30. Systemic glucocorticoids should be reserved for widespread and resistant lesions. Intralesional glucocorticoids are usually ineffective and may exacerbate the atrophic healing process31. Calcifying Lupus panniculitis in a patient without manifestations of systemic lupus Erythematosus]. Adjuvant treatments include topical care and prevention from injury. Surgical debridement or resection of individual lesions may be attempted when all other modalities have failed and there is appreciable debilitation. Surgical treatment includes the presence of recurrent infection, painful masses, ulcerations, and local functional impairment32.
In conclusion, we here report a case of lupus panniculitis with extensive dystrophic calcifications and any manifestation of SLE or other connective tissue disease. This is a case of lupus profundus associated to late dystrophic calcinosis due to calcium salt deposits derived from inflammatory process generated by a panniculitis process. These calcifying lesions which are found in perivascular and deep subcutaneous tissues, ulcerate, extrude and migrate through the surface of the skin revealing an aspect of whitish and chalk-like tissue. We highlight this case for the severity of lupus panniculitis and was originated after several years of a secondary and severe dystrophic calcinosis.
It has been described lupus panniculitis associated to discoid lupus, subacute cutaneous lupus, and systemic lupus erythematosus. It has been described cases of acute calcifying panniculitis or secondary panniculitis to renal failure and/or calciphylaxis and also described in severe dystrophic calcinosis as we described in the present case33,34. Although there are different reports of lupus calcinosis, up to we know there are not reports on lupus calcinosis associated to panniculitis as is this case5.
References
1. Yell JA, Mbuagbaw J, Burge SM. Cutaneous manifestations of systemic lupus erythematosus. Br J Dermatol 1996;135:355-362. [ Links ]
2. Diaz-Jouanen E, DeHoratius RJ, Alarcon-Segovia D, Messner RP. Systemic lupus erythematosus presenting as panniculitis (lupus profundus). Ann Intern Med 1975;82:376-382. [ Links ]
3. Tuffanelli DL. Lupus erythematosus (panniculitis) profundus: a classic revisited commentary and report of 22 cases. Hawaii Med J 1982;41:394-397. [ Links ]
4. Martens PB, Moder KG, Ahmed I. Lupus panniculitis: clinical perspectives from a case series. J Rheumatol 1999;26:68-72. [ Links ]
5. Fuchtenbusch M, Vogel A, Achenbach P, Gummer M, Ziegler AG, Albert E, et al. Lupus-like panniculitis in a patient with autoimmune polyendocrinopathycandidiasisectodermal dystrophy (APECED). Exp Clin Endocrinol Diabetes 2003;111:288-293. [ Links ]
6. Diaz Cascajo C. Panniculitis Definition of Terms and Diagnostic Strategy. Am J Dermatopathol 2000;22(6):530-549. [ Links ]
7. Kren O, op. cit., O. Kren, "lupus erythematosus" in Arch Dermatol u syph 1912;112:391-394. [ Links ]
8. Oppenheim M, 1915, op cit., M. Oppenheim, Lupus erythematosus Profundus", in Arch Dermatol u syph, 1912-1913;115:847. [ Links ]
9. Iglesias A. Las manifestaciones dermatológicas del lupus eritematoso. In: Historia del Lupus. Bogotá: Panamericana Press 2003;137-166. [ Links ]
10. Lipskeir E, Weizenbluth M. Calcinosis circumscripta: indications for surgery. Bull Hosp Jt Dis Orthop 1989;49:75-84. [ Links ]
11. Callen, J. Cutaneous lupus erythematosus: A personal approach to management. Australasian Journal of Dermatology 2006;47:13-27. [ Links ]
12. Sanchez NP, Peters MS, Winkelmann RK. The histopathology of lupus erythematosus panniculitis. J Am Acad Dermatol 1981;5:673-680. [ Links ]
13. Winkelmann RK, Peters MS. "Lupus Panniculitis", In dermatology update, reviews for physicians New York: Elsevier S. Moschella 1982;135-152. [ Links ]
14. Peters MS, Su WP. Lupus erythematosus panniculitis. Med Clin North Am 1989;73:1113-1126. [ Links ]
15. Diaz-Ramon JL, Izu R, Vicente JM, Mitxelena J, Aguirre A, Eizaguirre X, Diaz-Perez, JL. The Histopathological Spectrum of Lupus Panniculitis. Am J Dermatopathol 1998;20(6):614. [ Links ]
16. Wright D. Lupus panniculitis. Ann Rheum Dis 1997;56:7778. [ Links ]
17. Nossent HC. Swatak TJG. Berden JHM. Systemic lupus erythematosus: analysis of disease activity in 55 patients with endstage renal failure treated with hemodialysis or continuous ambulatory peritoncal dialysis. Am J Med 1990;89:169-174. [ Links ]
18. Thoong SC, Stenzel KH. End stage renal disease in systemic lupus erythematosus profundus. Clin Exp Dermatol 1989;14:333. [ Links ]
19. Quismoro FP, Dubois EL, Chandor SB. Soft-tissue calcification in systemic lupus erythematosus. Arch Dermatol 1975;111:352-356. [ Links ]
20. Kelli W. M. Callen J. Calcifying Lupus Panniculitis in a Patient with Subacute Cutaneous Lupus Erythe matosus: Response to Diltiazem and Chloroquine. The Journal of Rheumatology 2001;28:9. [ Links ]
21. Thurson C, Curtis A. Lupus Erythematosus Profundus (Kaposi-Irgang): Clinical Response to Hydroxychloroquine Sulphate. Arch Dermatol 1966;93:557. [ Links ]
22. Tuffanelli DL. Management of cutaneous lupus erythematosus. Clin Dermatol 1985;3:123-130. [ Links ]
23. Burrows NP, Walport MJ, Hammond Ah, Davey N, Jones RR. Lupus erythematosus profundus with partial C4 deficiency responding to thalidomide. Br J Dermatol 1991;125:62-67. [ Links ]
24. Fuchs D, Fruchter L, Fishel B, Holtzman M, Yaron M. Colchicine suppression of local inflammation due to calcinosis in dermatomyositis and progressive systemic sclerosis. Clin Rheumatol 1986;5:527-530. [ Links ]
25. Chung H-S, Hann S-K. Lupus panniculitis treated by a combination therapy of hydroxychloroquine and quinacrine. J Dermatol 1997;24(5):69. [ Links ]
26. Skuterud E, Sydnes OA, Haavik TK. Calcinosis in dermatomyositis treated with probenecid. Scand J Rheumatol 1981;10:92-94. [ Links ]
27. Berget RG, Featherstone GL, Raasch RH, McCarthey WH, Hadler NM. Treatment of calcinosis universalis with low-dose warfarin. Am J Med 1987;83:72-76. [ Links ]
28. Yoshida S, Torikai K. The effects of warfarin on calcinosis in a patients with systemic sclerosis. J Rheumatol 1993;20:1233-1235. [ Links ]
29. Farah MJ, Palmieri Gm, Sebes JI, Cremer MA, Massie JD, Pinals RS. The effects of diltiazem on calcinosis in a patient with the CREST syndrome. Arthritis Rheum 1990;33:1287-1293. [ Links ]
30. Vayssairat M, Hidouche D, Abdoucheli-Baudot N, Gaitz JP. Clinical significance of subcutaneous calcinosis in patients with systemic sclerosis. Does ditiazem induce its regression? Ann Rheum Dis 1998;57:252-254. [ Links ]
31. Lee SS, Felsenstein J, Tanzer FR. Calcinosis cutis circumscrpta: treatment with intralesional corticosteroid. Arch Dermatol 1978;114:1080-1081. [ Links ]
32. Lipskeir E, Weizenbluth M. Calcinosis circumscripta: indications for surgery. Bull Hosp Jt Dis Orthop 1989;49:75-84. [ Links ]
33. Nogueira P, Giuliani C, Rey N, Said M, Cochat P. Calcifying panniculitis in a child after renal transplantation, Nephrology Dial Transplant 1997;12:216-218. [ Links ]
34. Ming-Tien C, Kuo-Su C, MingJing C, Ning L, ChiJen T, RurSheng Y, WenJin C. Lupus profundus (panniculitis) in a chronic haemodialysis patient. Nephrol Dial Transplant 1999;14:966-968. [ Links ]














