Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Colombiana de Reumatología
Print version ISSN 0121-8123
Rev.Colomb.Reumatol. vol.24 no.1 Bogotá Jan./Mar. 2017
https://doi.org/10.1016/j.rcreu.2016.08.003
Case report
Use of rituximab for granulomatosis with polyangiitis-associated peripheral ulcerative keratitis☆
a Servicio de Oftalmología, Hospital Pablo Tobón Uribe, Medellín, Colombia
b Oftalmología, Universidad Pontificia Bolivariana, Medellín, Colombia
A 31-year-old female, presented with polyarthralgia, asymmetrical polyarthritis, fever, vasculitis skin lesions, together with decreased visual acuity in the right eye with severe peripheral corneal melting, peripheral ulcerative keratitis, fibrin hypopyon and posterior synechiae. Given the clinical and paraclinical findings with positive C-ANCA (anti-neutrophil cytoplasmic antibodies), the patient was diagnosed with granulomatosis with polyangiitis with ocular (corneal melting, peripheral ulcerative keratitis and uveitis), and systemic involvement. Treatment was started with methylprednisolone and cyclophosphamide, but due to poor control, Rituximab was subsequently administered, with medical improvement.
Keywords: Granulomatosis with polyangiitis Wegener granulomatosis Cornea Peripheral ulcerative keratitis Rituximab Uveitis
Mujer de 31 años con cuadro de poliartralgias, poliartritis asimétrica, fiebre, lesiones vasculíticas en piel, asociado a disminución de agudeza visual en ojo derecho, el cual presentaba compromiso corneal con adelgazamiento periférico severo, queratitis ulcerativa periférica, hipopión de fibrina y sinequias posteriores. Ante el cuadro clínico y paraclínicos con C-ANCA positivos, se realiza el diagnóstico de granulomatosis con poliangeítis con compromiso ocular (adelgazamiento corneal, queratitis ulcerativa periférica, uveítis) y sistémico. Se inicia tratamiento con metilprednisolona y ciclofosfamida con poco control, por lo que se inicia rituximab sistémico, evolucionando hacia la mejoría.
Palabras clave: Granulomatosis con poliangeítis Granulomatosis de Wegener Córnea Queratitis ulcerativa periférica Rituximab Uveítis
Purpose
The purpose is to describe the use of rituximab in peripheral ulcerative keratitis, corneal peripheral melting and uveitis in a patient with granulomatosis with polyangiitis.
Methods
Case report. Patient evaluated in the Services of Ophthalmology and Rheumatology of a high complexity hospital in Medellin, Colombia.
Results
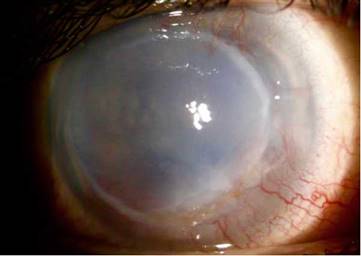
A 31-year-old female patient, with a personal history of pulmonary tuberculosis 8 years ago with complete treatment, idiopathic diffuse bronchiectasis, giant cell tumor in the left proximal femur 9 years ago, cholecystectomy, without significant ocular personal antecedents. She consults for a clinical picture of 10 days of evolution, sudden onset, consisting of polyarthralgia, asymmetric summatory polyarthritis in wrists, left elbow, ankles an right knee, fever, vasculitic lesions of petechial type and plaques with erythematous borders, irregular, necrotic infiltrated at the malleolar level of the right lower limb, 4 days later she presented pain in the right eye, photophobia, and decreased visual acuity. The ophthalmological physical examination showed a best corrected visual acuity in right eye (RE) light perception, left eye (LE) 20/20, at bio-microscopy, RE: conjunctiva with ciliary and mixed injection, sclera without nodules or thinning, limbal superficial vascularization in 360°, cornea with peripheral melting of 80% in 360°, epithelial ulcer of 80%, severe generalized edema, inferotemporal blister, fibrin hypopyon of 50%, posterior synechiae, without further details due to anterior opacity (Fig. 1), LE, within normal limits.

Fig. 1 Initial manifestations: 360° limbal superficial vascularization, cornea with 360° peripheral melting, epithelial ulcer, severe generalized edema, fibrin hypopyon.
Paraclinical tests were requested to clarify the causes of her symptomatology: ocular ultrasound with mild vitritis, negative C-reactive protein, hemogram with leukocytosis, without neutrophilia, thrombocytosis, elevated erythrocyte sedimentation rate, 24 h proteinuria of 110 mg, negative HIV, negative VDRL, negative blood cultures, negative Gram stain and culture of ocular secretion, negative bacilloscopies, sputum culture: Pseudomonas aeruginosa grow as a colonization of bronchiectasis. Autoimmune profile: rheumatoid factor, ANA and ENA negative, C-ANCA 1:20, C4 and C3 hypocomplementemia. CT scan of the paranasal sinuses: pansinusitis, chest HRCT: centriacinar micronodules with bilateral scattered distribution, cylindrical saccular bronchiectasis of basal predominance with mucus plug inside. Normal abdominal CT scan, normal echocardiogram. Given the clinical features and the high specificity of the positive.
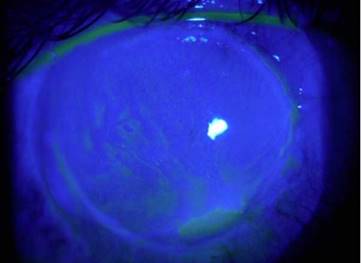
C-ANCA, jointly with Rheumatology it was established the diagnosis of granulomatosis with polyangiitis with ocular (corneal melting, peripheral ulcerative keratitis, uveitis), cutaneous (vasculitis), paranasal sinuses (recurrent pansinusitis), involvement, summatory polyarthritis of large joints; the pulmonary involvement was not characteristic, because it consisted of bronchiectasis. Treatment with pulses of methyl-prednisolone and cyclophosphamide, topical treatment with 20% autologous serum, sodium hyaluronate, loteprednol and atropine was started without any improvement of the inflammatory process, so it was decided subsequently to initiate rituximab 500 mg weekly, for 4 doses, without adverse effects. The ocular condition slowly evolved toward improvement (Fig. 2), with recovering from the corneal meltingby 40% (Fig. 3) and closure of the corneal epithelial ulcer (Fig. 4) in the last evaluation, 4 months later, with best corrected visual acuity of hand movement, explained by a dense leukoma as a sequel. She continues currently under follow-up and visual rehabilitation.
Discussion
Granulomatosis with polyangiitis is a systemic disease of unknown cause, characterized by granulomatous inflammation of the upper and lower respiratory tract, vasculitis and necrotizing nephritis; it is part of the group of ANCA-associated vasculitis, it presents 2 clinical forms (localized and systemic),1 it has a prevalence of 3 cases per 100,000 people in the United States, most frequent in the fifth to sixth decades of life.2 Its diagnosis is supported by the C-ANCA, with a specificity of up to 98%.1,3,4 Ocular involvement is reported in 28-60% of cases in whichever clinical form. The most common manifestations are the orbital inflammatory disease, necrotizing scleritis and peripheral ulcerative keratitis.3 It has been postulated that the etiology of the latter would be due to an occlusive vasculitis with commitment of the perilimbar vasculature and accumulation of antibody complexes in the epithelium, causing local inflammatory activity that leads to peripheral thinning, which is usually associated with necrotizing scleritis,5,6 different from the case described. The classical management consists of the use of systemic steroids in conjunction with cytotoxic agents such as cyclophosphamide and methotrexate.1,7,8 The anti-CD20 monoclonal antibody, rituximab, has been recently used for refractory cases.9-11 Few case reports have been published internationally with the use of rituximab for peripheral ulcerative keratitis refractory to treatment, with good outcomes.12,13 The case described corroborates the usefulness of rituximab in peripheral ulcerative keratitis, peripheral melting and uveitis secondary to granulomatosis with polyangiitis, with positive outcomes in terms of visual acuity and control of progression.
Conclusions
Granulomatosis with polyangiitis may exhibit ocular involvement, which includes peripheral ulcerative keratitis and uveitis. Treatment includes immunosuppression with steroids, methotrexate and cyclophosphamide. In refractory cases are used biological agents such as rituximab, which in this case was effective in the management of peripheral ulcerative keratitis and uveitis.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Acknowledgements
Hospital Pablo Tobón Uribe, Universidad Pontificia Bolivariana, Medellin, Colombia.
REFERENCES
1. Tarabishy AB, Schulte M, Papaliodis GN, Hoffman GS. Wegener's granulomatosis: Clinical manifestations, differential diagnosis, and management of ocular and systemic disease. Surv Ophthalmol. 2010;55:429-44. [ Links ]
2. Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, et al. Wegener granulomatosis: An analysis of 158 patients. Ann Intern Med. 1992;116:488-98. [ Links ]
3. Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med.1997;337:1512-23. [ Links ]
3. Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med. 1997;337:1512-23. [ Links ]
4. Finkielman JD, Merkel PA, Schroeder D, Hoffman GS, Spiera R, St Clair EW, et al. Antiproteinase 3 antineutrophil cytoplasmic antibodies and disease activity in Wegener granulomatosis. Ann Intern Med. 2007;147:611-9. [ Links ]
5. Reynolds I, Tullo AB, John SL, Holt PJ, Hillarby MC. Corneal epithelial-specific cytokeratin 3 is an autoantigen in Wegener’s granulomatosis-associated peripheral ulcerative keratitis. Invest Ophthalmol Vis Sci. 1999;40:2147-51. [ Links ]
6. Reddy SC, Tajunisah I, Rohana T. Bilateral scleromalacia perforans and peripheral corneal thinning in Wegener’s granulomatosis. Int J Ophthalmol. 2011;4:439-42. [ Links ]
7. De Groot K, Rasmussen N, Bacon PA, Tervaert JWC, Feighery C, Gregorini G, et al. Randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52:2461-9. [ Links ]
8. Jones RB, Tervaert JWC, Hauser T, Luqmani R, Morgan MD, Peh CA, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363:211-20. [ Links ]
9. Keogh KA, Wylam ME, Stone JH, Specks U. Induction of remission by B lymphocyte depletion in eleven patients with refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52:262-8. [ Links ]
10. Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, Schroeder DR, Specks U. Rituximab for refractory Wegener’s granulomatosis: Report of a prospective, open-label pilot trial. Am J Respir Crit Care Med. 2006;173:180-7. [ Links ]
11. Onal S, Kazokoglu H, Koc A, Yavuz S. Rituximab for remission induction in a patient with relapsing necrotizing scleritis associated with limited Wegener’s granulomatosis. Ocul Immunol Inflamm. 2008;16:230-2. [ Links ]
12. Huerva V, Sánchez MC, Traveset A, Jurjo C, Ruiz A. Rituximab for peripheral ulcerative keratitis with Wegener granulomatosis. Cornea. 2010;29:708-10. [ Links ]
13. Freidlin J, Wong IG, Acharya N. Rituximab treatment for peripheral ulcerative keratitis associated with Wegener's granulomatosis. Br J Ophthalmol. 2007;91:1414. [ Links ]
Received: June 24, 2016; Accepted: August 26, 2016











 text in
text in