Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Colombiana de Reumatología
Print version ISSN 0121-8123
Rev.Colomb.Reumatol. vol.25 no.1 Bogotá Jan./Mar. 2018
https://doi.org/10.1016/j.rcreu.2017.04.004
Case report
Hematological changes as the initial manifestation of primary Sjögren's syndrome✩
a Servicio de Medicina Interna, Hospital Universitario Mayor Mederi, Bogotá, Colombia
The case is presented of a 50-year-old woman with persistent abnormal uterine bleeding, secondary anemia, adynamia, and asthenia, in whom bicytopenia is documented with microcytic normochromic anemia and thrombocytopenia. After conducting a thorough study of the causes of bicytopenia, the diagnosis of Sjögren's syndrome was made, in the absence of dry symptoms.
Keywords: Sjögren syndrome; Anemia; Thrombocytopenia
Se presenta el caso de una mujer de 50 arios de edad con cuadro de hemorragia uterina anormal persistente, síndrome anémico secundario, astenia y adinamia, en quien se documenta bicitopenia con anemia normocítica normocrómica y trombocitopenia. Después de realizar un minucioso estudio de las causas de la bicitopenia, se diagnostica síndrome de Sjögren primario, en ausencia de síntomas secos.
Palabras clave: Síndrome de Sjögren; Anemia; Trombocitopenia
Introduction
Sjögren's syndrome is a chronic autoimmune disease, characterized by the presence of clinical manifestations due to the involvement of the exocrine glands and, occasionally, by extraglandular involvement, conditioning its prognosis. Usually, the first clinical manifestations of the patients are xerostomia (dry mucous membranes) and xerophthalmia (ocular dryness). Other etiologies associated with dry syndrome, such as the use of anticholinergic drugs, hypothyroidism, hepatitis B and C infection, menopause, among others, should be ruled out to make an accurate diagnosis.
In addition to the dry symptoms we can find extraglandular commitment such as polyarthritis, Raynaud's phenomenon or anemia. The diagnosis is based on the demonstration of exocrine glandular involvement and the presence of positive antibodies such as anti-Ro, anti-La and rheumatoid factor.1
Sjögren's syndrome occurs in patients of all ages, predominantly in women between 40 and 50 years of age. 1 It is classified as primary when it is not associated with any disease and as secondary when it is associated with other autoimmune diseases. Its etiopathogenesis is multifactorial, and the onset of the autoimmune process is due to a combination of intrinsic and extrinsic factors. Patients with primary Sjogren's syndrome may develop hematological alterations as an initial manifestation in 5-10% of cases. 2
Clinical case
A 50-year-old female patient with a history of uterine myomatosis, who was admitted due to a clinical picture of two months of evolution consisting of mucocutaneous pallor, asthenia, adynamia, reduction of functional class II/IV on the NYHA scale and persistent vaginal bleeding. The patient did not report weight loss or nocturnal diaphoresis, and did not have dry symptoms.
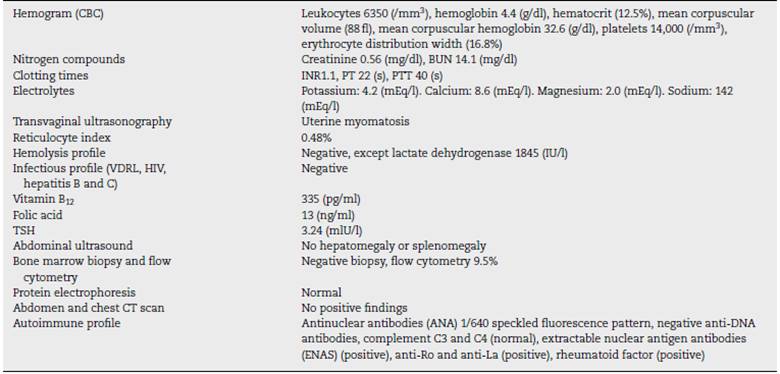
On admission, the patient was tachycardic, with mucocutaneous pallor and vaginal bleeding. The paraclinical tests on admission showed normocytic, normochromic anemia and thrombocytopenia. Studies of bicytopenia were initiated in order to rule out deficiency, infectious, autoimmune and neo-plastic etiologies (Table 1).
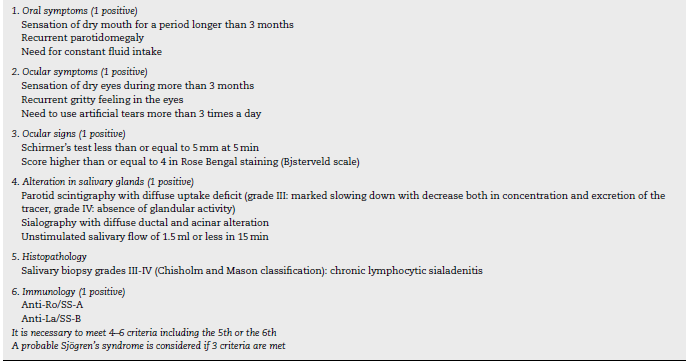
In the complementary studies, the presence of positive antinuclear antibodies (ANA), antibodies to extractable nuclear antigens (ENAs) and rheumatoid factor was evidenced in the immunological profile, and for this reason, a picture compatible with Sjögren's syndrome of atypical presentation was considered as a diagnostic possibility; it was carried out a salivary gland biopsy which reported chronic sialadenitis grade III/IV in the Chisholm Mason classification. In this way, it was confirmed the diagnosis of primary Sjögren's syndrome with the onset of hematological manifestations; and it was established management with methylprednisolone and azathioprine with progressive improvement of the bicytopenia, evidencing a gradual rise in hemoglobin, with a control at discharge of 9.3 g, and an increase in platelets to 53,000/mm3.
Discussion
Sjögren's syndrome is a chronic inflammatory autoimmune disease, which mainly affects the exocrine glands. It may occur alone (primary), or associated with another connective tissue disease (secondary); its diagnosis is based on the classification criteria proposed by the American-European Consensus Group published in 2012 (Table 2). 3
It is the second most common systemic rheumatic disease, with an estimated prevalence between 0.1% and 4.8%. It mainly affects middle-aged women with a women to men ratio of 9:1. 4
It is characterized by an alteration in the response of T and B lymphocytes, which generates exocrine gland damage through an inflammatory cascade that perpetuates the lesion. The infiltration of lymphoplasmacytic cells in the salivary and lacrimal glands, with subsequent fibrosis thereof, is responsible for the cardinal symptomatology. 5
There are different extraglandular manifestations, such as hematological alterations, which include anemia, hemocytopenias, monoclonal gammopathies and lymphoproliferative disorder, predominantly B-cell non-Hodgkin's lymphoma. 6 Hematological manifestations can occur as the first manifestation of hidden Sjögren's syndrome, therefore, this disease should be taken into account as a differential diagnosis in the presence of unexplained cytopenias. 7
Hematological alterations are a frequent finding in different autoimmune diseases, being found in up to 25-50% of patients. There are several pathophysiological mechanisms involved in the emergence of anemia, which include the peripheral destruction of mature red blood cells, alteration in the production of red blood cells and hematopoietic alterations secondary to autoimmune mechanism. Anemia is documented in up to 34.1% of patients with primary Sjögren's syndrome. The leading cause of anemia is chronic disease in 69%, and to a lesser extent autoimmune hemolytic anemia (10%), iron deficiency anemia (9%) and other causes (4%),8 being autoimmune hemolytic anemia the most severe. 9
The anemia secondary to chronic disease is explained by the release of hepcidin, a peptide of hepatic origin with antimicrobial activity and involved in iron homeostasis. Hepcidin inhibits the activity of ferroportin 1, decreasing the basolateral transport of iron in the duodenum, in addition to increasing the uptake and storage by the reticuloendothelial system, inhibiting its release from the macrophages and the liver. On the other hand, proinflammatory cytokines, tumor necrosis factor, interferon gamma and interleukin 1 decrease the production of erythropoietin (EPO) and block the action of the circulating EPO. This anemia can be treated with recombinant EPO and iron substitution. 10
Among the factors related to a higher prevalence of anemia is the presence of ANA, anti-Ro, anti-La and anticardiolipin antibodies. In a study conducted to classify the primary Sjögren s syndrome, it was found that patients with anti-Ro antibodies had a higher frequency of systemic characteristics, including hematological alterations such as anemia and thrombocytopenia. 11
Among the hematological alterations, leukopenia can also be evidenced in 14-42% of patients, associated with autoimmune neutropenia or lymphopenia, usually with a chronic presentation; however, in some occasions they may appear in acute form as an effect of medications or due to infections associated with immunosuppression, 12 in the same way as thrombocytopenic purpura.
Sjögren s syndrome can be associated with the appearance of type II mixed cryoglobulinemia (polyclonal IgG and monoclonal IgM with rheumatoid factor activity) that entails peripheral neuropathy, Raynaud s phenomenon, purpura, kidney injury and arthralgias. 13
Progression to non-Hodgkin lymphoma is found in 4-6% of patients with Sjögren s syndrome; it has been associated with an increase in beta 2 microglobulin, presence of cryoglobulinemia, negativization of the rheumatoid factor, increase in the size of the parotid glands, adenomegalies and splenomegaly. 14
The treatment of Sjögren s syndrome is focused on the management of the dry symptoms; however, extraglandular manifestations will require additional immunomodulatory management. In the case of hematological alterations, iron supplementation, folic acid, cyanocobalamin, EPO, immunomodulatory treatment with corticosteroids, azathioprine, cyclophosphamide or methotrexate should be added, according to their etiology; some cases refractory to treatment will require the administration of immunoglobulin, as well as the performance of splenectomy in the most serious cases associated with severe thrombocytopenia. 15
Hematological alterations are a frequent finding in the different autoimmune diseases; however, in Sjögren s syndrome they are not a pathognomonic manifestation, and for this reason, in patients with few or no dry symptoms, as in the case presented, a delay in the correct diagnosis and timely management can occur. That is why the hematological alterations described should be taken into account as an initial manifestation of Sjögren s syndrome, progression of the disease, associated infection or adverse effects of the medications.
Conclusion
Sjögren s syndrome is an autoimmune disease that is characterized by the presence of dry symptoms, xerostomia (dry mucous membranes) and xerophthalmia (ocular dryness), however, it can be associated with extraglandular manifestations which include hematological alterations. Although these alterations occur with a high degree of frequency, it is atypical that this would be their sole manifestation, as in the case of the patient presented.
That is why in the different hematological alterations, such as cytopenias, the autoimmune diseases, and among them, Sjögren s syndrome, must be taken into account among the differential diagnoses.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
REFERENCES
1. Morcillo Valle M. Síndrome de Sjögren, Hospital el Escorial San Lorenzo. Madrid, España; 2009. [ Links ]
2. Rosas Gómez de Salazar J, Senabre Gallego JM, Santos Ramírez C. Manejo de las manifestaciones extraglandulares del síndrome de Sjögren primario, sección de reumatología Hospital María Baxia, Alicante, España, 30 Junio 30 de 2010. [ Links ]
3. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjögren's syndrome: A revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002;61:554-8. [ Links ]
4. Tincani A, Andreoli L, Cavazzana I, Doria A, Favero M, Fenini M, et al. Novel Aspects of Sjögren’s syndrome in 2012. BMC Med. 2013;11:93. [ Links ]
5. Khattri S, Barland P. Primary Sjögren's syndrome and autoimmune cytopenias. Bull NYU Hosp Jt Dis. 2012;70:130-2. [ Links ]
6. Manganelli P, Fietta P, Quaini F. Hematologic manifestations of primary Sjögren’s syndrome. Clin Exp Rheumatol. 2006;24:438-48. [ Links ]
7. Zhou JG, Fen Y, Jiang L, Yang QB, Luo WF. Clinical analysis of primary Sjögren’s syndrome complicating anemia. Clin Rheumatol. 2010;29:525-9. [ Links ]
8. Shinoda K, Taki H, Hounoki H, Ogawa R, Sugiyama E, Tobe K. Severe autoinmune hemolytic anemia associated with igM warm auto-antibodies in primary Sjögren síndrome. Int J Rheum Dis. 2010;13:94-6. [ Links ]
9. Kamath V, Prabhakar B, Veena, Lachikarathman D. Sjögren’s thrombocytopenia. J Assoc Physicians India. 2011;59:114-5. [ Links ]
10. Autrel-Moignet A, Lamy T. Autoimmune neutropenia. Presse Med. 2014;43:e105-18. [ Links ]
11. Rudolph SE, Kouba M, Hrdlicka P. Severe corticoid-refractory autoimmune thrombocytopenia associated with mixed connective tissue disease (Sharp’s syndrome). Treatment with rituximab. Dtsch Med Wochenschr. 2009;134:1734-8. [ Links ]
12. Radman I. Hematological Abnormalities in rheumatic disease. Reumatiziam. 2006;53:11-7. [ Links ]
13. Coppo P, Sibilia J. Agranulocitosis asociada con el síndrome de Sjögren primario. ¿Es un trastorno benigno? Ann Rheum Dis. 2003;62:476-8. [ Links ]
14. Navarro B, Yebra M, Romero J, Suárez D. Linfoma de Hodgkin asociado a síndrome de Sjögren primario. Med Clin. 2001;16:636. [ Links ]
15. Schattner A, Friedman J, Klepfish A, Berrebi A. Immune cytopenias as the presenting finding in primary Sjögren’s syndrome. QJM. 2000;93:825-9. [ Links ]
Received: November 25, 2016; Accepted: April 20, 2017; other: June 07, 2017











 text in
text in