Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Colombiana de Reumatología
versão impressa ISSN 0121-8123
Rev.Colomb.Reumatol. vol.25 no.1 Bogotá jan./mar. 2018
https://doi.org/10.1016/j.rcreu.2017.04.003
Case report
Sulphasalazine-induced eosinophilia and systemic symptoms: A case report✩
a Facultad de Ciencias de Salud, Universidad del Quindío, Armenia, Colombia
b Departamento Medicina Laboral, Valsalud, Armenia, Colombia
Drugs reactions with eosinophilia and systemic symptoms can be caused by an extensive list of medications, including sulphasalazine. The compromise is very varied, from skin rash to visceral involvement, accompanied by an eosinophilia that can sometimes lead to death. The cornerstone of the treatment is the suspension of the aggressive medication and the use of oral and intravenous corticosteroids, depending on the severity of the condition.
Keywords: Drug hypersensitivity syndrome; Eosinophilia; Sulphasalazine
La reacción a drogas con eosinofilia y síntomas sistémicos es una condición debida a una lista extensa de medicaciones, entre las que se encuentra la sulfasalazina. El compromiso es muy variado, desde rash cutáneo hasta afectación visceral acompañado de eosinofilia, que en ocasiones puede llevar a la muerte. El pilar del tratamiento es la suspensión del medicamento agresor y el uso de corticosteroides orales e intravenosos dependiendo de la severidad del cuadro.
Palabras clave: Síndrome hipersensibilidad droga; Eosinofilia; Sulfasalazina
Introduction
The acronym DRESS refers to "Drug Reaction with Eosinophilia and Systemic Symptoms", it is a rare, potentially fatal condition with skin manifestations and visceral involvement. 1 The number of cases in the different reports is variable, ranging from 1 per 1000 to 10,000 exposures. 2,3 Adults are more affected than children. The importance of this syndrome lies in the timely recognition and treatment, since the estimated mortality is 10-20%.4
Clinical case
A 65-year-old woman who consulted for a clinical picture that began in 2014 with pain in the right knee with swelling, subjective fever and left red eye without pain or suppuration. The patient has a personal history of hypothyroidism under treatment with levothyroxine, 50 mcg once a day, orally. Her sister has a HLA B27 positive spondyloarthritis in treatment with tumor necrosis factor blocker. On physical examination it was found a severe left scleral congestion, as well as joint effusion in the right knee. Ophthalmology ruled out uveitis and considered the diagnosis of scleritis, for which it was initiated therapy with topical steroids, with improvement of her ocular condition. With the above information a peripheral spondyloarthritis was suspected and paraclinical exams were requested. After 20 days, it was found a C-reactive protein of 159 mg/l, erythrocyte sedimentation rate: 46 mm/h, HLA B27, rheumatoid factor negative with leukocytosis and neutrophilia and normal knee X-rays. Joint effusion and heat in both knees with entheses pain in both elbows was documented in this occasion. Treatment was started with sulphasalazine 1 g twice a day, prednisone 5 mg once a day, and calcium + vitamin D once a day; all medications taken by mouth. Three weeks later she consulted for non-quantified high fever and skin rash. On the articular examination was found pain at flexion-extension of the right knee with effusion, in addition, maculopapular lesions mainly in the trunk and extremities, without fever at the time of consultation. The laboratory tests showed eosinophilia of 1080/mm3, ESR: 93 mm/h, CRP: 48 mg/l, AST: 86, ALT: 118, there was no alteration in renal function, nor anemia or eosinophils in the urine. There was no pleural effusion on the chest radiograph, A DRESS was diagnosed, it was ordered to immediately suspend the sulphasalazine and prednisone and it was started the administration of deflazacort, 30 mg once a day (the patient had existences) for 7 days and then 15 mg once a day. In the control of the next month, there was no fever, rash, red eye or joint pain. The laboratory tests did not show eosinophilia and the liver function was normalized; the deflazacort was reduced to 6 mg once a day. 6 months later she attended consultation again due to pain in one finger of the right hand and in both knees. It was evidenced edema, erythema of the 1st right proximal interphalangeal joint with joint effusion in the ipsilateral knee. There was elevation of acute phase reactants: erythrocyte sedimentation rate 54 mm/h, C-reactive protein 96 mg/l. A chest X-ray and a tuberculin skin test were requested with the purpose of initiating anti-TNF therapy.
The tuberculin test was reported in 10 mm and there were no alterations in the chest X-ray, it was started treatment with isoniazid 300 mg, once a day for 9 months orally. One month later, the patient began treatment with golimumab, 50 mg monthly subcutaneously. After 7 months of follow-up the patient remains asymptomatic with laboratories within normal ranges.
Review
The term DRESS was coined by Bocquet based on the description of 24 patients of Callot, who called it drug-induced pseudolymphoma and hypersensitivity syndrome. 5,6 The pathophysiology of DRESS is still not fully understood. Among the suggested hypotheses there is a disorder in the biotransformation of active metabolites of a drug that would eventually activate the immune response with the subsequent clinical characteristics of the disease. It has been reported an association between the herpesvirus 6 and the development of the disease, 7 based on the late onset of the signs and symptoms after exposure to the drug, clinical and laboratory findings suggestive of viral infection and episodes of exacerbation after the suspension of the offending agent. 8 Other viral agents such as herpesvirus 7, cytomegalovirus and Epstein Barr virus have been involved. 9,10 The detection of the reactivation by the herpesvirus 6 has been used in Japan and in some European countries as an aid in the diagnosis of the disease. 11 However, the clear role of this virus in the etiopathogenesis has been questioned. 12 There is no characteristic histopathological pattern that defines DRESS. It has been described a perivascular or diffuse lymphocytic infiltrate, eosinophils in the dermis with or without edema thereof or a band-like infiltrate of atypical lymphocytes imitating a fungal mycosis.
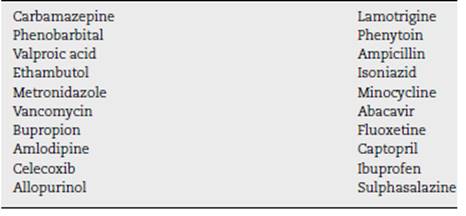
The drugs most frequently associated with DRESS are anti-convulsants, however, it has been described an extensive list (Table 1).
Sulphasalazine is a compound of sulphapyridine and 5-aminosalicylic acid (5-ASA) linked by an azo bond. Most of the drug reaches the colon where the azo bond is reduced by the action of the colonic bacteria releasing the 2 aforementioned components. It has been mainly used in the treatment of rheumatoid arthritis, as monotherapy or combined, and in peripheral spondyloarthritis. Sulphapyridine is the main therapeutic component for rheumatic diseases. 13 The adverse effects of sulphasalazine are usually mild and reversible after discontinuation, and occur in the first months of treatment with subsequent reduction over time. 14 The most frequent are nausea, exanthema, neutropenia, megaloblastic anemia, headache, and alteration in liver function. Serious adverse reactions are rare events. 15 Both sulphapyridine and 5-ASA have been involved in the DRESS. 16
The clinical manifestations occur between 3 weeks and 3 months after the intake of the drug, but this time is shortened with its reintroduction. 17 High fever is the most common symptom (90-100%) followed by rash (87%) especially with anticonvulsant drugs. 18-20 The cutaneous commitment is varied, it can be a morbilliform eruption, maculopapular reaction, erythema multiforme, purpuric or desquamative lesions, or cheilitis. 21 For some authors, facial edema, especially periorbital, is present in 25% of patients and may be key in the diagnosis of the DRESS. 22,23 Painful lymphadenopathy is found in 70% of cases, it can be localized or generalized and disappears with the suspension of the offending medication. The visceral involvement includes myocarditis, pericarditis, interstitial nephritis, encephalitis, meningitis, colitis, thyroiditis and hepatitis. 24 Hepatic affection is the most common internal manifestation (50-60%) and it behaves as an anicteric hepatitis (51%) that can progress to fulminant hepatic failure and death. Myocarditis usually occurs late, even several months after the withdrawal of the offending agent and is most commonly associated with the use of ampicillin and minocycline. 25 A decreased ventricular ejection fraction and pericardial effusion can be found in the echocardiogram, and in the electrocardiogram there are changes in the ST segment or in the T wave.
Laboratories usually show leukocytosis that can reach up to 50,000 leukocytes/mm3 with marked eosinophilia (up to 20,000), which can occur in up to 30% of patients. Eosinophilia may occur between one and two weeks after the onset of the disease and is associated with visceral involvement. Atypical lymphocytes similar to those of infectious mononucleosis can also be seen in 30% of cases. Thrombocytopenia, hemoglobin drop and hemophagocytic syndrome have also been reported. 26 The elevation of transaminases, especially ALT, has been found in 70% of patients with DRESS and they may persist elevated for several days after the withdrawal of the drug involved27; a severe elevation of ALT (>10-fold) with liver failure has been reported mainly in women between the 2nd and 4th decades of life under treatment with sulphasalazine. 28
The renal involvement may manifest itself as an elevation in creatinine and urea nitrogen, in addition to proteinuria and hematuria. Eosinophiluria can also be found, but no abnormalities are observed on renal ultrasound. Myocarditis can be suspected when CPK and troponin are elevated.
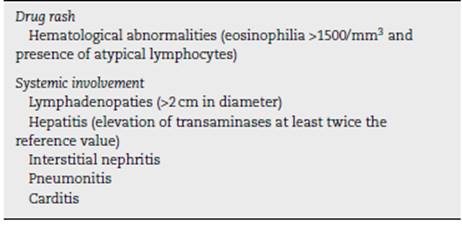
The diagnosis of DRESS is not always easy because the clinical and laboratory manifestations are varied and are not always present, besides the fact that the list of causative agents is also extensive. The criteria of Bocquet et al. have been used to define the DRESS, for which at least 3 findings are required (Table 2).
A Japanese group created other classification criteria similar to those mentioned above, but also included fever, persistence of findings after the withdrawal of the drug, as well as measurement of HHV 6, which makes it unviable in many hospitals and centers that do not have the possibility to perform this test.
Regarding the treatment, the most important issue is the rapid detection of the DRESS and the immediate suspension of the offending agent. Currently, the general treatment measures are of support and symptomatic control of the different clinical manifestations. In case that the main manifestations are cutaneous, antihistamine agents can be useful.
Glucocorticoids are the medication preferred by physicians despite the scarce existing evidence. 29 Prednisone at 1 mg/kg/day, orally, improves the symptoms and laboratory patterns, especially when there is hepatitis, nephritis, carditis or pneumonitis. In case of severe visceral involvement such as encephalitis, hemophagocytic syndrome, respiratory failure, renal failure or severe hepatitis, the patient can receive pulses of methylprednisolone at 30 mg/kg/day, for 3 days30 or immunoglobulin at a dose of 2 g/kg during 5 days intravenously. 31 The use of antivirals such as ganciclovir is reserved for cases of herpes infection.
In our case, the patient consulted for a clinical picture of peripheral spondyloarthritis according to ASAS criteria for which she received sulphasalazine, and 3 weeks later she had Bocquet criteria expressed with drug-induced rash, systemic compromise given by hepatitis and although she had eosinophilia, it was not higher than 1500/mm3, perhaps due to the previous intake of corticosteroids and the early detection of the condition. The rapid withdrawal of sulphasalazine and the treatment with intermediate doses of steroids led to the resolution of the clinical picture with normalization of the laboratory parameters.
This report illustrates the need for early recognition of this disease and the timely treatment to avoid complications derived from the use of a medication of the daily life of the rheumatologist.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on human beings or animals for this research.
Confidentiality of data. The authors state that patient data do not appear in this article.
Right to privacy and informed consent. The authors state that patient data do not appear in this article.
REFERENCES
1. Newell B, Moinfar M, Mancini A, Nopper A. Retrospective analysis of 32 pediatric patients with anticonvulsant hypersensitivity syndrome (ACHSS). Pediatr Dermatol. 2009;26:536-46. [ Links ]
2. Shear N, Spielberg S. Anticonvulsant hypersensitivity syndrome In vitro assessment of risk. J Clin Invest. 1988;82:1826-32. [ Links ]
3. Fiszenson-Albala F, Auzerie V, Mahe E, Farinotti R, Durand-Stocco C, Crickx B, et al. A 6-month prospective survey of cutaneous drug reactions in a hospital setting. Br J Dermatol. 2003;149:1018-22. [ Links ]
4. Piüana E, Lei S, Merino R, Melgosa M, de La Vega R, Gonzáles-Obeso E, et al. DRESS-syndrome on sulfasalazine and naproxen treatment for juvenile idiopathic arthritis and reactivation of human herpevirus 6 in an 11-year-old Caucasian boy. J Clin Pharm Ther. 2010;35:365-70. [ Links ]
5. Bocquet H, Bagot M, Roujeau J. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250-7. [ Links ]
6. Callot V, Roujeau J, Bagot M, Wechsler J, Chosidow O, Souteyrand P, et al. Drug-induced pseudolymphoma and hypersensitivity syndrome. Two different clinical entities. Arch Dermatol. 1996;132:1315-21. [ Links ]
7. Suzuki Y, Inagi R, Aono T, Yamanishi K, Shiohara T. Human herpesvirus 6 infection as a risk factor for the development of severe drug-induced hypersensitivity syndrome. Arch Dermatol. 1998;134:1108-12. [ Links ]
8. Criado P, Avancini J, Santi C, Medrado A, Rodríguez C, de Carvalho J. Drug reaction with eosinophilia and systemic symptoms (DRESS): a complex interaction of drugs, viruses and the immune system. Isr Med Assoc J. 2012;14:577-82. [ Links ]
9. Oskay T, Karademir A, Ertürk O. Association of anticonvulsant hypersensitivity syndrome with Herpesvirus 6, 7. Epilepsy Res. 2006;70:27-40. [ Links ]
10. Seishima M, Yamanaka S, Fujisawa T, Tohyama M, Hashimoto K. Reactivation of human herpesvirus (HHV) family members other than HHV-6 in drug-induced hypersensitivity syndrome. Br J Dermatol. 2006;155:344-9. [ Links ]
11. Shiohara T, Kano Y. A complex interaction between drug allergy and viral infection. Clin Rev Allergy Immunol. 2007;33:24-133. [ Links ]
12. Augusto J, Sayegh J, Simon A, Croue A, Chennebault J, Cousin M, et al. A case of sulphasalazine-induced DRESS syndrome with delayed acute interstitial nephritis. Nephrol Dial Transplant. 2009;24:2940-2. [ Links ]
13. Pullar T, Hunter J, Capell H. Which component of sulphasalazine is active in rheumatoid arthritis? Br Med J (Clin Res Ed). 1985;290:1535-8. [ Links ]
14. Amos R, Pullar T, Bax D, Situnayake D, Capell H, McConkey B. Sulphasalazine for rheumatoid arthritis: toxicity in 774 patients monitored for one to 11 years. Br Med J (Clin Res Ed). 1986;293:420-3. [ Links ]
15. Plosker GL, Croom K. Sulfasalazine: a review of its use in the management of rheumatoid arthritis. Drugs. 2005;65:1825-49. [ Links ]
16. Ransford R, Langman M. Sulphasalazine and mesalazine: serious adverse reactions re-evaluated on the basis of suspected adverse reaction reports to the Committee on Safety of Medicines. Gut. 2002;51:536-9. [ Links ]
17. Shiohara T, Inaoka M, Kano Y. Drug-induced hypersensitivity syndrome (DIHS): a reaction induced by a complex interplay among herpesviruses and antiviral and antidrug immune responses. Allergol Int. 2006;55:1-8. [ Links ]
18. Gentile I, Talamo M, Borgia G. Is the drug-induced hypersensitivity syndrome (DIHS) due to human herpesvirus 6 infection or to allergy-mediated viral reactivation? Report of a case and literature review. BMC Infect Dis. 2010;10:49. [ Links ]
19. Criado P, Lucena S, Crivellaro A, Criado R, Tebcherani A, Nogueira A, et al. Drug hypersensibility síndrome to anticonvulsivants: report of two cases. Rev Bras Clin Terap. 2002;28:59-63. [ Links ]
20. Chang D, Shear N. Cutaneous reactions to anticonvulsants. Semin Neurol. 1992;12:329-37. [ Links ]
21. Choudhary S, McLeod M, Torchia D, Romanelli P. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Syndrome. J Clin Aesthet Dermatol. 2013;6:31-7. [ Links ]
22. Ganeva M, Gancheva T, Lazarova R, Troeva J, Baldaranov I, Vassilev I, et al. Carbamazepine-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: report of four cases and brief review. Int J Dermatol. 2008;47:853-60. [ Links ]
23. Criado P, Criado R, Vasconcellos C, Pegas J, Cera P. Drug-induced hypersensitivity syndrome due to anticonvulsants in a two-year-old boy. J Dermatol. 2004;31:1009-113. [ Links ]
24. Kano Y, Ishida T, Hirahara K, Shiohara T. Visceral involvements and long-term sequelae in drug-induced hypersensitivity syndrome. Med Clin North Am. 2010;94:743-59. [ Links ]
25. Bourgeois G, Cafardi J, Groysman V, Pamboukian S, Kirklin J, Andea A, et al. Fulminant myocarditis as a late sequela of DRESS: two cases. J Am Acad Dermatol. 2011;65:889-90. [ Links ]
26. Mockenhaupt M. Severe drug-induced skin reactions: clinical features, diagnosis, etiology, and therapy. J Dtsch Dermatol Ges. 2009;7:142-60. [ Links ]
27. Kano Y, Shiohara T. The variable clinical picture of drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms in relation to the eliciting drug. Immunol Allergy Clin North Am. 2009;29:481-501. [ Links ]
28. Fernando S, Henderson C, O’Connor K. Drug-induced hypersensitivity syndrome with superficial granulomatous dermatitis. A novel finding. Am J Dermatopathol. 2009;31:611-3. [ Links ]
29. Roujeau J, Stern R. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994;331:1272-85. [ Links ]
30. Kito Y, Ito T, Tokura Y, Hashizume H. High-dose intravenous immunoglobulin monotherapy for drug-induced hypersensitivity syndrome. Acta Derm Venereol. 2012;92:100-1. [ Links ]
31. Descamps V, Ben Said B, Sassolas B, Truchetet F, Avenel-Audran M, Girardin P, et al. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137:703-8. [ Links ]
Received: February 23, 2017; Accepted: April 26, 2017; other: August 16, 2017











 texto em
texto em