Introduction
Granulomatosis with polyangiitis (GPA) is a systemic small-vessel vasculitis which affects almost any organ. Ocular manifestations occur in 30-50% of patients, and in 8% of cases can lead to permanent blindness.1 The orbital commitment occupies the second place after the scleral involvement, occurring in 5-30% of patients with GPA. 1 The orbital inflammation can occur primarily as a granulomatous lesion (orbital pseudotumor) or secondarily, either by diffuse infiltration of a nasal disease or by extraocular myositis. 1 Although the orbital pseudotumor is the most frequent cause of ocular proptosis in GPA representing 40-60% of orbital tumors2 in this disease; we should not forget that there are some other secondary ocular manifestations with orbital involvement in GPA.
The clinical and prognostic relevance is that the orbital disease in this vasculitis has been associated with functional loss of the eye and serious systemic disease. 3
Below we present the case of a woman with GPA who started with extraocular myositis, the rarest form of orbital involvement in this vasculitis.
Case presentation
A 56-year-old woman who started with pain and right ocular proptosis in 2013 was treated with systemic steroids, with which the episode remitted. In 2015 she presented again pain and right ocular proptosis and was treated by the ophthalmologist who documented by computerized axial tomography (CAT) of the orbits, extraocular myositis; in order to obtain a diagnosis, the patient underwent a biopsy of the upper rectus muscle and the lacrimal gland. The histopathological result was nonspecific inflammation; (Fig. 1A and B) and she received prednisone at a dose of 1 mg/kg/day for 2 months with which there was a remission. In March 2016 she presented weight loss, fever, neuropathic pain in the lower extremities, painful right ocular proptosis; and extraocular myositis was documented by CAT scan (Fig. 2A and B). The diagnosis of GPA was integrated due to the ocular involvement, constitutional symptoms, sensory neuropathy in lower extremities and positive antineutrophil cytoplasmic antibodies (ANCA) (c-ANCA: 1:40 [reference value: <1:40] and PR3: 5.4 [reference value: <4.3]). The patient received 3 boluses of methylprednisolone 1 g and cyclophosphamide 1 g monthly for 6 months; subsequently, a CAT scan of the orbits was performed in November 2016 (Fig. 3A and B) in which a remission of the ocular manifestation was found.
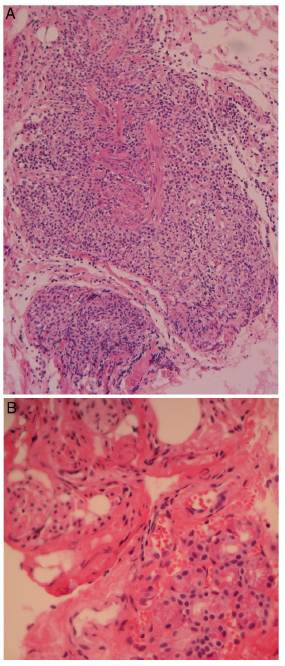
Fig. 1 (A) Photomicrography of the upper rectus muscle at medium magnification showing a dense inflammatory infiltrate mixed with bundles of smooth muscle (H&E, original amplification 20 x). (B) High magnification photomicrography of the main lacrimal gland showing few acini and some bundles of smooth muscle "Müller's muscle" (H&E, original amplification 40 x).
Fig. 2 (A) CAT scan of the orbits with right sagittal reconstruction where there is a slight increase in the thickness of the upper rectus muscle, inferior rectus muscle with preserved features. (B) CAT scan of the orbits with coronal reconstruction where thickening of the upper rectus and lateral muscles of the right orbit is observed with discrete caudal displacement of the eyeball.
Case discussion
GPA is a systemic vasculitis in which any structure of the eye can be compromised, however, the most frequent are the episclera in 20-25% and the sclera in 15-20%.4 Orbital involvement occurs in 15% of patients with this vasculitis and occupies the second place in ocular compromise. 5
Due to the nature of the vasculitis itself, there are few series that report ophthalmologic findings in this disease. The series in which the orbital involvement is classified and which describes in more detail is that of Ismailovaet al., 1 in which 74 patients with orbital manifestations are described in a series of 226 patients with GPA followed-up for 4 years. Of the 74 patients with orbital involvement, 45 (60.8%) had a granulomatous lesion (orbital pseudotumor), 26 (35.2%) developed rhinosinusitis with orbital involvement and 3 (4%) developed extraocular myositis. The 3 patients who developed extraocular myositis had localized GPA with negativity for ANCA, 2 of them had recurrence of the manifestation and none of them developed systemic disease.
The case presented shows a woman with painful unilateral proptosis with a final diagnosis of GPA, but who started with extraocular myositis, which was recurrent; it was not until the second recurrence when she developed systemic manifestations and the diagnosis of systemic GPA could be integrated. The induction of remission with high doses of steroids and cyclophosphamide showed significant clinical and radiological improvement. Although the biopsy of the extraocular muscle did not show data compatible with vasculitis; the response to treatment, as well as the extraocular clinical manifestations and the positivity of ANCAs allowed us to obtain the diagnosis. The role of biopsy in this orbital manifestation has not been studied.
According to our search, it is the first case of systemic GPA that began with unilateral and recurrent extraocular myositis.
When the ophthalmologist faces a patient with painful unilateral proptosis, he must consider GPA within the etiological possibilities; and the rheumatologist who faces a patient with an established diagnosis of GPA, and who develops painful unilateral proptosis must consider, in addition to the orbital pseudotumor, extraocular myositis as another diagnostic possibility.
Conclusions
The ocular manifestations in GPA can represent, from the functional point of view, a catastrophe for the patient, even leading him/her to blindness, it is important that both rheumatologists and ophthalmologists are familiar with the ocular clinical spectrum of this systemic vasculitis, since the timely diagnosis definitely changes the prognosis.











 text in
text in