Digital ulcers: definitions
A universally accepted definition of digital ulcers in systemic sclerosis (SSc) is lacking. The etiologic mechanism may be considered to distinguish between ischemic ulcers, those related to articular deformities, and those associated with calcinosis (Figs. 1 and 2). A study based on the assessment of clinical images by experts showed adequate intra-observer reproducibility (K coefficient 0.81), although inter-observer reproducibility was weaker (K coefficient 0.46).1 This fact presents a relevant methodological consideration due to the following reasons: (i) this compromise is included within the revised classification criteria for SSc2; (ii) digital ulcers are considered as an outcome, either primary or secondary, in several clinical trials. These concepts have been addressed by some authors who have aimed at standardizing clinical approaches.3,4 An international study proposed a specific definition through a literature review and an expert consensus: loss of epidermal covering with a break in the basement membrane (which separates dermis from epidermis). It appears clinically as visible blood vessels, fibrin, granulation tissue and/or underlying deeper structures (e.g., muscle, ligament, fat) or as it would appear on debridement. Thus, this definition excludes a scar, an abrasion, an incision, a fissure, or a laceration.5
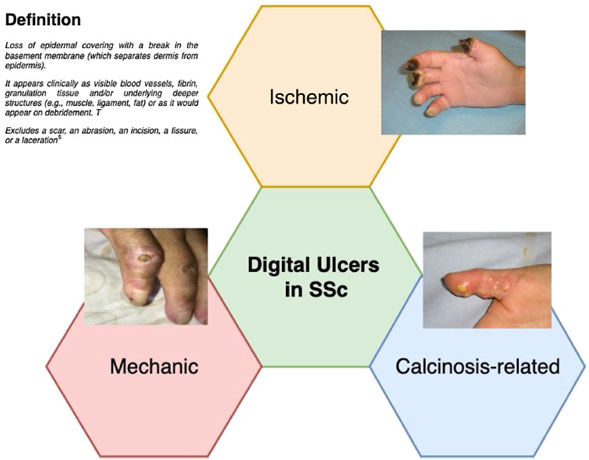
Fig. 1 Definition and etiology of digital ulcers in systemic sclerosis. Adapted from Suliman et al. [5].

Fig. 2 Examples of digital ulcers in systemic sclerosis, Panels A and B illustrate calcinosis-related ulcers. Panels C and D show ischemic ulcers. Courtesy of Pr. Yannick Allanore.
In clinical practice, it is essential to consider differential diagnoses, such as atherosclerotic macroangiopathy, phenomena of thrombophilia (e.g., antiphospholipid syndrome), embolic events (including septic embolisms, such as in endocarditis), vasculitides (particularly cryoglobulinemia), and even paraneoplastic syndromes.6
Pathophysiology
Vasculopathy is a cardinal feature of SSc. It is certainly illustrated by the wide prevalence of Raynaud's syndrome, which is present in over 95% of patients and is often its first clinical sign. Thus, the involvement of microvascular architecture and the activation of endothelial cells appear to be among the earliest events in the natural history of the disease. The pathophysiology of ulcers is complex and includes vascular ischemia and probably the involvement of mechanical factors (Fig. 3). At the early stages, vascular damage is mainly vasomotor and reversible. However, the onset of diffuse vascular structural anomalies ultimately leads to microcirculation obliteration, which generates progressive tissue hypoxia that turns into permanent over time. In addition, endothelial cells in the arterioles undergo apoptosis, which fosters the expression of adhesion molecules and their interaction with several cytokines and growth factors. These phenomena promote intimal proliferation that blocks the lumen and activates pericytes. The endothelial production of vasodilating substances, such as nitric oxide (NO) and prostacy clins, is reduced, whereas the production of vasoconstrictive substances, such as endothelin-1, is augmented. Further, the neurovascular control disequilibrium is mainly peripheral, although central alterations have been identified, such as the reduction of vasodilating substances (e.g., calcitonin gene-related peptide) and vasoconstriction due to activation of α-2 adrenergic receptors. In addition, several other alterations that contribute to vascular obstruction have been described, namely, insufficient fibrinolysis due to endothelial compromise, leukocyte activation, a reduced erythrocyte deformability, an increased blood viscosity, and a rise in free radicals (i.e., oxidative stress). Platelet activation induces overexpression of thromboxane, a vasoconstrictive molecule.7,8 Another important element is the increased synthesis of VEGF (vascular endothelial growth factor), which is stimulated by the augmented endothelial permeability and hypoxia. Its action may represent an attempt to repair vascular damage; however, it is either insufficient or ineffective, as illustrated by the increase in serum concentrations and its association with the presence of avascular areas in capillaroscopy. Further, VEGF appears to be a molecular link between vascular damage and fibrosis. In addition, an alteration in compensatory mechanisms of vascular damage appears to be present, namely angiogenesis (i.e., compensatory growth of new vessels from residual vessels) and vasculogenesis (i.e., de novo vessel formation).9,10 Some of these molecules may be potential biomarkers for ulceration risk.
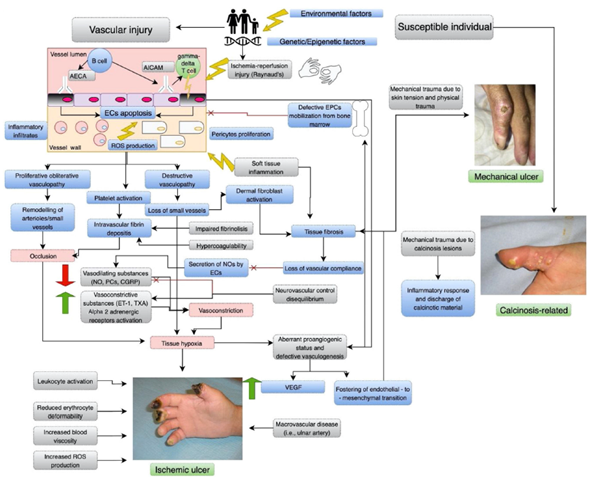
Fig. 3 Proposed pathophysiologic mechanisms of digital ulcers in systemic sclerosis. The pathophysiology of digital ulcers (DUs) in systemic sclerosis (SSc) is complex and involves several mechanisms, in which vasculopathy is a cardinal feature. Gray boxes display the main identified mechanisms. Red boxes show critical events. Due to a multifaceted interaction between genetic, epigenetic and environmental factors, a susceptible individual develops SSc in which DUs appear. The initial vascular injury is mainly vasomotor and reversible, particularly due to ischemia-reperfusion injury, such as Raynaud's phenomenon. In addition, an aberrant immune response contributes to the initial insult. In patients with SSc, үδ T cells express CD49d, an activation marker that mediates the adherence to endothelial cells (ECs) through the vascular adhesion molecule-1 (VCAM-1), and have been shown to induce ECs damage. B - cells produce antibodies against ECs; Anti-Endothelial Cell Antibody (AECA) induce EC apoptosis, while Anti-Intercellular Adhesion Molecule-1 (AICAM) antibody promotes reactive oxygen species (ROS) production and the expression of VCAM-1. These insults will induce ECs apoptosis, infiltration of inflammatory cells and pericytes proliferation, which will contribute to proliferative-obliterative and destructive vasculopathies. The former will promote small vessel remodeling, while the latter will yield the loss of these vessels, leading to vascular occlusion. In addition, vascular injury promotes platelet activation and the formation of intravascular fibrin deposits. As an impaired fibrinolysis and hypercoagulability have been described in patients with SSc, these phenomena will foster vessel occlusion. The loss of small vessels will result in tissue fibrosis due to dermal fibroblast activation, that among other effects, will reduce vascular compliance, which is an important stimulus for ECs secretion of nitric oxide synthase (NOs). Further, a reduction in other vasodilating substances, such as prostacyclins (PC) and an increase in vasoconstrictive substances, including endothelin-1 (ET-1) and thromboxane A (TXA), have been observed. This disequilibrium is worsened by an impaired neurovascular control, in which central alterations in vasodilation (e.g., calcitonin gene-related peptide, CGRP) and vasoconstriction due the activation of α-2 adrenergic receptors have been described. All these events will lead to tissue hypoxia with the formation of an ischemic ulcer. An aberrant proangiogenic status and a defective vasculogenesis have been reported in these patients. For instance, after vascular injury, Endothelial Progenitor Cells (EPC) are mobilized from the bone marrow and recruited to vascular lesions. However, a decreased number, dysfunction, and/or impaired recruitment have been described in SSc, leading to an ineffective vascular repair. An increased synthesis of vascular endothelial growth factor (VEGF) has been observed, which is stimulated by the augmented endothelial permeability and hypoxia. Its action may represent an attempt to repair vascular damage, nonetheless it is either insufficient or ineffective. Some other events (see gray boxes) contribute to ischemic ulcers development. In addition, these defects foster endothelial-to-mesenchymal transition, that will lead to tissue fibrosis. Regarding mechanical ulcers, their mechanisms are mainly due to skin tension and physical trauma. Calcinosis-related ulcers present mechanical trauma due to calcinosis lesions, but will present an inflammatory response and the discharge of calcinotic material. Adapted from: Allanore et al. [8], Matucci-Cerinic et al. [9], and Asano et al. [7].
Large vessels, such as digital or ulnar arteries, are occasionally affected, without the presence of atherosclerotic lesions.11 In recurrent lesions, magnetic resonance (MR) or computed tomography (CT) angiography may be indicated to determine the need of reperfusion strategies.
Epidemiology
The literature on the epidemiology of digital ulcers is consistent and suggests that one out of every two patients will present at least one digital ulcer throughout the course of their disease.12-14,3 The first ulceration may appear early and a higher risk of recurrence will be present. The strongest risk factor for the development of an ulcer is the fact of having a previous ulcer. Regarding clinical associations, recent literature has shown an increased risk in patients suffering from the diffuse cutaneous subtype and in the presence of anti-topoisomerase I autoantibodies.12-14,3 Male patients present an increased risk of ulcers and vascular complications.15 Some reports have suggested an association with other signs of vasculopathy, such as the presence of telangiectasia, a reduced carbon monoxide diffusion, and even with pulmonary hypertension. A prospective study by EUSTAR has suggested that the presence of ulcerations may be a marker of reduced survival.14 These facts have led to propose the concept of a unified vascular phenotype during the course of SSc.8
Clinical consequences
Digital ulcers are often recurrent, multiple and tend to affect both hands. Healing time depends on the severity of the lesions and on the time of medical intervention, although it is acknowledged that it is usually delayed. A study in which 100 patients were followed and 1614 lesions were observed, suggested a mean healing time of 76 days.16 The presence of underlying calcinosis prolonged healing time (94 days). Some other negative factors were reported, such as the presence of osteomyelitis, perilesional edema, abnormally dry or wet necrosis, the presence of a pressure sore, visible underlying structures (e.g., tendons, ligaments), or gangrene.16 Local infections are common and the isolation of Staphylococcus aureus is frequent. Nonetheless, some other microorganisms, such as enterobacteria, may be isolated, thus highlighting the paramount importance of hygiene and patient's education, particularly when chronic wounds are present. In the European DUO registry, 32% of patients required antibiotic therapy for a soft tissue infection.17 When osteoarticular infection is suspected, a magnetic resonance imaging should be performed.
On the other hand, the risk of vascular compromise complications should be considered, such as critical ischemia that may evolve into gangrene; sometimes these events are associated with infections. In a study of 2080 patients, the vast majority had developed ulcers during the course of their disease (58%).18 A third of them (32%, n = 666) presented persistent or recurrent ulcers, and among those, 30% (n = 197) were considered severe (due to the presence of gangrene, amputation or the need of sympathectomy). In the randomized trial that assessed the effects of bosentan on the recurrence of ulcers, among 188 patients, 11% required amputation.19 In the DUO registry, among 4944 recruited patients, 4642 presented analyzable data regarding the development of gangrene: 82% (n = 3787) were classified as "never", 18% (n = 855) as "previous gangrene", and 6% (n = 258) as "current gangrene". The 3 groups were rather homogenous, although smoking habits were more frequent in the previous and current gangrene groups. The severity and complexity of the vascular compromise was confirmed by the increased frequency of hospitalization and surgical intervention in the groups with a history of gangrene. Based on the data of patients with an adequate follow-up (n = 3809), multivariable analyses showed that, at inclusion, previous smoking habits, a history of 3 or more digital ulcers, and a previous gangrene episode or sym-pathectomy, predicted the development of a new episode of gangrene (n = 243).20
The cardinal symptom of ulcerations is pain, which is usually continuous and present during night, yielding a negative and significant functional impact. A recent analysis of the DUO registry, based on 2327 patients, showed that a higher number of ulcers at inclusion (0,1-2 and >3) was associated with a higher risk of inability to work during the previous month (8, 42 and 48%, respectively), a higher disability to perform simple daily tasks (35, 54 and 63%, respectively), and to a higher expenditure due to the need of paid help (mean number of hours: 17, 36 and 64, respectively).21 Digital ulcers are one of the fundamental phenomena driving permanent disability in SSc.22 Reducing the number and the severity of ulcers would allow to diminish the disability burden associated to the disease, particularly when the functionality of the hand is recovered.23 Fig. 4 summarizes the main consequences of digital ulcers in SSc.
Management
When digital ulcers appear, the management must be expeditious and should be based on patient's awareness of clinical changes and the availability of medical interventions by the treating physician. Early warning signs to be aware of are: an increasing frequency of Raynaud's phenomenon flares, a prolongation of the cyanotic phase, and any other tissue change that suggests digital necrosis.
Non-pharmacologic treatments
The patient should avoid cold stimuli that trigger Raynaud's crisis. Smoking habits are equally harmful and interventions aimed at stopping tobacco should be implemented.24,25 Medications that trigger Raynaud's phenomenon should be avoided or suspended whenever possible. Regarding mechanical ulcers associated with articular deformations, a low awareness threshold is encouraged, particularly when local lesions due to trauma are present.
Local treatment is fundamental and patients should be taught about adequate care habits. The 3 objectives of local treatment are: to prevent infectious complications, to protect wounds from trauma that may generate a local aggravation or pain, and to foster healing. Wound cleansing with saline solution or soap and water is recommended. Using antiseptic solutions may generate contact eczema, irritant dermatitis, promote antibiotic resistance and may delay healing. Thus, local antibiotics should be avoided. Mechanical cleansing and debridement should be performed under appropriate analgesia. The election of adhesive dressings is based on the healing stage and the appearance of the ulcer. Hydrocolloid dressings (i.e., substances that form a gel when mixed with water) are based on a humid milieu.26 Some other dressing options such as hydrocellular polyurethane films may be used in this type of wounds as well. Neutral tulles (i.e., a lightweight, very fine cloth that resembles a net or a gauze), Vaseline® or paraffin are adequate alternatives. In case of local superinfection, topical antibacterial products such as flammazine (i.e., silver sulfadiazine) are sometimes applied as a thick layer and covered by a dry compress, or a Vaseline® or silicone-soaked compress, and hold temporarily by a gauze bandage.
In severe or refractory cases, hyperbaric oxygen, which is a developing alternative in diabetic ulcerations, has been offered to patients with SSc.27,28
Vasodilators
Vasodilators play an essential role in the management of digital ulcers in SSc.
Calcium channel inhibitors
Calcium channel inhibitors (CCI) are an effective strategy for the management of digital ulcers, as they reduce the number and the severity of Raynaud's crises. One meta-analysis suggests a reduction in the number and the severity of flares within a period of 2 weeks of -8.3 [CI -15.7; -0.91] and of -0.7 [-1.2; -0.17], respectively, for the CCI group as a whole, and of -10.2 [-20.1; -0.3] and -0.99 [-1.74; -0.24], respectively, for nifedipine.29 None of the included studies presented data regarding the prevention or the evolution of digital ulcers. One cross-over controlled trial that assessed 10 patients reported a reduction in the number of digital ulcers, although without statistical significance. Another trial compared iloprost and nifedipine (10-20 mg, 3 times per day) during a 16 weeks follow-up, and showed a reduction of 4.3 compared to 1.4 digital ulcers (p< 0.001) in favor of nifedipine; however, the evolution was close to that of iloprost and the lack of a placebo control undermined an adequate interpretation.30
Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists
Although the rationale to propose these drug classes as a treatment strategy appears solid, data on Raynaud's syndrome do not support neither their utility nor their efficacy for digital ulcers. A large study over a 3 years follow-up period did not report effectiveness of quinapril for the prevention of global vascular progression of the disease.31,32
Prostacyclins
Prostacyclins analogs are potent vasodilators with anti-aggregation properties and anti-remodeling effects on smooth muscle cells. Adverse effects are mainly complications of venous accesses, hypotension, vertigo, flushing, abdominal pain and diarrhea, skin allergies and sometimes jaw pain. Two therapeutic studies revealed that prostacyclin infusions improved the healing of ulcers and prevented the appearance of new lesions.33,34 The infusion protocol was a continuous infusion of 0.5-20 ng/kg/min over at least 6 h for 5 consecutive days. Some other authors have adapted this protocol in severe patients using repeated infusions for 3-5 days during the winter.35 A sub-cutaneous preparation (treprostinil) was studied in a randomized trial; however, it did not show a beneficial effect on ulcers.36 Moreover, an oral preparation (selexipag), which was recently developed for pulmonary hypertension, was not effective in a trial of SSc-associated Raynaud's phenomenon.37
Endothelin receptor antagonists
Endothelin-1 is the most potent vasoconstrictor substance. It presents vascular remodeling effects due to its action on smooth-muscle cells. Its effect occurs through 2 receptors, namely, ETA and ETB, which are expressed by smooth muscle cells and play a role in vasoconstriction and vascular hyper-plasia; ETB receptors are expressed by endothelial cells as well and promote vasodilation. Bosentan is a non-selective endothelin antagonist that blocks both ETA and ETB. At first, it was approved for pulmonary hypertension, and thereupon, two phase 3 trials on ulcers revealed a significant effect on recurrence prevention, but not on healing nor on Raynaud's syndrome.19,38 These findings were reinforced in a trial including 188 patients that presented at least 1 active digital ulcer who were randomized and followed for 24 weeks. The total number of ulcers was 1.9±0.2 for bosentan versus 2.7±0.3 for placebo (p = 0.035; magnitude of improvement of 30%).19 A trend toward a higher effect in patients with a larger number of ulcers at inclusion was observed. A three-fold increase in aminotransferases was detected in up to 10.5% of patients on bosentan; monitoring at least once a month is recommended. This medication is usually offered to patients with multiple or recurrent ulcers. Nevertheless, treatment duration is not well defined and some groups employ this treatment as a prevention strategy in high-risk patients during cold seasons only, whereas others prefer a long-term usage.
Macitentan is another non-selective endothelin inhibitor that exhibits a higher bioavailability than bosentan. It is approved for pulmonary arterial hypertension. Nonetheless, in two large randomized studies, it did not prevent the appearance of new ulcers in SSc.39
Ambrisentan is a selective antagonist of ETA It is approved for the treatment of pulmonary arterial hypertension. However, it has not been evaluated in rigorous trials for the management of digital ulcers. Only one study with interim results has been reported, which is rather inconclusive.40 Thus, it is not used in the context of digital ulcers.
Phosphodiesterase-5 inhibitors
Phosphodiesterase-5 inhibitors prevent the destruction of cyclic GMP, thus increasing its bioavailability and fostering a high concentration of NO. The latter acts as a vasodilator due to the relaxation of smooth muscle cells, and as an anti-platelet aggregation agent.
In a meta-analysis comprising 6 randomized trials, phosphodiesterase inhibitors were effective in reducing the activity of SSc-associated Raynaud's syndrome, although with a moderate effect.41 Further, a study assessing as-needed sildenafil 40 mg or 80 mg, showed a moderate benefit on the activity of Raynaud's syndrome in SSc.42
Regarding digital ulcers, a randomized trial that included 83 patients compared sildenafil 20 mg three times per day or placebo for 12 weeks.43 The primary outcome was the healing time of each ulcer (192 ulcers were included). The median healing time was 63 (59-86) days in the placebo arm compared to 56 (55-60) days in the sildenafil arm (p = 0.18). However, since week 8, the healing rate was superior in the sildenafil group (65% vs. 51%) and this benefit persisted through week 12 (78% vs. 66%).43 In addition, excellent tolerance was reported. These results did not lead to a registration request for this medication. This product, for which generic formulations are available, is often used in clinical practice as an off-label first-line medication in order to avoid the use of prostacyclins. It is used by some teams prior to the application of bosentan, or either in association with this drug as a bridging therapy before the use of prostacyclin. Tadalafil was studied in a randomized trial that supported the beneficial effects of this drug class on ulcers, although with a low statistical power.44
Treatment combinations
Long-term and systematic use of CCI is recommended in SSc for the prevention of disease progression. Whenever an ulcer appears, CCI should be continued and potent vasodilators should be associated, particularly prostacyclins to foster healing, and bosentan to prevent recurrence in case of multiple ulcers. Sildenafil is used as an off-label medication in both situations, although it is used as a bridging therapy for prosta-cyclins as well or in association with bosentan in severe or refractory disease.45,46 Nonetheless, randomized trials assessing these combinations are lacking, while a great interest for the treatment of SSc-associated pulmonary arterial hypertension has been elicited.
Other treatment strategies
Interim results of a randomized trial have suggested the beneficial effects of atorvastatin 40 mg per day due to a reduced frequency of new ulcers, with an adequate tolerance profile and without musculoskeletal adverse events. Several studies have shown further potential benefits in this context, thus supporting larger trials.47 Anticoagulants and anti-aggregation therapies are occasionally offered to patients who develop ulcers. However, studies that support a benefit are lacking. In fact, an open-label study reported the absence of effect of a low molecular weight heparin.48 Further, the association of salicylic acid and dipyridamole was not useful in a study with a low statistical power.49 In clinical practice, low dose salicylic acid is often given to patients with a vascular compromise phenotype. One should always assess a risk-benefit balance for this intervention, as a high risk for gastrointestinal bleeding is present in patients with SSc, particularly when risk factors for gastric ulcers are present; angiodysplasia-associated bleeding may be present as well.
Several anti-oxidative strategies have been assessed without compelling results (e.g., vitamin E, N-acetylcysteine, dimethyl sulfoxide). Vasodilators such as ketanserine, prazosin, and prostaglandins have been assessed in preliminary studies.49 Immunosuppressants have not been studied in this particular context, though neither an increased risk has been reported with rituximab, tocilizumab, or any other usual synthetic immunosuppressant.
Surgical interventions
Surgical interventions are seldom indicated for the management of digital ulcers in SSc. Surgical debridement is indicated exceptionally in otherwise uncontrolled pain, or the need to remove necrotic tissue as a potential risk factor for infection. In case of mummification, whenever possible, it is equally recommended to avoid to precipitate scarring tissue removal. Sympathectomy was previously offered, although it has been gradually abandoned.49 An equivalent therapy through the injection of botulinum toxin may play a role nowadays, although its evidence is based only on interim results particularly focused on Raynaud's syndrome.50 The rationale for a local treatment is still strong. Several topical vasodilators or anti-oxidative agents have been studied without compelling results.49 A recent development proposes the injection of fatty tissue, which may contain progenitor cells that may foster angiogenesis in an injured tissue and may promote healing. This tissue fraction appears to be rich in mesenchymal stem cells that may be equally beneficial. A pilot study in patients with digital ulcers has been recently published and may offer alternatives for refractory cases.51
Conclusion
Digital ulcers are frequent over the course of SSc and are a significant source of morbidity. They occur due to vasculopathy and, besides general measures, their treatment is based on the use of vasodilator agents. A better classification system of these lesions may guide care strategies and the formulation of standardized and personalized management protocols.











 text in
text in 



