Introduction
Systemic sclerosis is a chronic multi-systemic auto-immune disease characterized by excessive collagen deposits, vascular hyperreactivity, and obstructive microvascular phenomena.1 This condition is classified based on the rate of progression, cutaneous and visceral compromise, into limited or diffuse disease. Three main processes characterize the pathophysiology of the disease: (1) fibroblast dysfunction that increases the deposits of extracellular matrix, (2) production of auto-antibodies, and (3) vasculopathy.2
Manifestations of vascular injury include Raynaud phenomenon, digital ischemia, pulmonary arterial hypertension, and renal crisis. The last one is developed mainly in patients with diffuse systemic sclerosis (proximal cutaneous compromise).1
Scleroderma renal crisis is the primary manifestation of renal compromise in patients with systemic sclerosis, and it is considered a medical emergency. It is developed in approximately 4.2% of patients with diffuse disease, and in 1.1% of patients with limited disease; most cases occur during early phases (first years) of the disease.3,4
There is not an accepted standard definition for scleroderma renal crisis.5 It is characterized by recent onset, rapidly progressive arterial hypertension (defined as: systolic arterial pressure above 140 mmHg and diastolic pressure above 90 mmHg, or increased systolic pressure by at least 30 mmHg, or an increased diastolic pressure by at least 20 mmHg, or development of hypertensive encephalopathy) and/or acute renal failure (defined as an increase of more than 50% from baseline serum creatinine or 120% above the upper limit of normal range, or proteinuria >2 + in urinalysis confirmed by protein-to-creatinine ratio above the normal value, or hematuria ≥2 + or 10 red blood cells per field) without another cause to explain it, and/or microangiopathic hemolysis (platelets <100,000/mm3, schistocytes, increased reticulocyte count).3,5,6
The pathophysiology of scleroderma renal crisis remains unclear. It is believed that it begins in a renal vascular intima that presents injured endothelial cells, causing a thickening of the intima and proliferation of arcuate and interlobular arteries, producing a reduction of the vascular lumen and renal blood flow. Local vasoconstriction could also be present, similar to Raynaud's phenomenon ("Renal Raynaud's phenomenon") that contributes to the reduction of renal perfusion. Low renal blood flow produces hyperplasia of juxtaglomerular apparatus, and increased production of renin, activating the renin-angiotensin-aldosterone pathway. Since these renal vascular changes and hyperreninemia are present in patients with systemic sclerosis, not all of them suffering a renal crisis, other factors should be involved in the development of a renal crisis. Endothelin-1 is a potent vasoconstrictor and fibrosis mediator that is involved in vascular manifestations of systemic sclerosis, and high levels have been documented in patients with scleroderma renal crisis and in those with pulmonary arterial hypertension. Increased expression of endothelin-1 receptors A and B present in the kidneys of patients with renal crisis has been documented. The use of cocaine, cyclosporine, and glucocorticoids (prednisone ≥15mg/day for more than three months) could precipitate the development of renal crisis.1,3,7
Approximately, 90% of patients have arterial hypertension (arterial pressure > 150/90 mmHg) with clinical manifestations given by malignant hypertension with hypertensive encephalopathy, which is characterized by an acute or sub-acute beginning, accompanied by lethargy, fatigue, confusion, headache, visual changes, and seizures (focal or generalized). 11-14% of patients with renal crisis do not develop hypertension. Patients with normal pressure renal crisis usually have received treatment with glucocorticoids, two-thirds present thrombotic microangiopathy, and the prognosis is worse, compared to patients with hypertensive renal crisis.1,3,7
Before the introduction of angiotensin-converting enzyme inhibitors (ACEI), the prognosis of patients with scleroderma renal crisis was ominous, and it was the first cause of death in patients with systemic sclerosis. The introduction of ACEI in 1979, improved the evolution of patients with scleroderma renal crisis, based on the reduction of mortality from 76% to 15%.8 However, despite the fact that treatment with ACEI improves the outcomes of patients with renal crisis, the prognosis of patients who present this complication is still reserved, pointing the need for new therapeutic agents besides the ACEI.
Nowadays, there is no substantial scientific evidence that demonstrates the use of other therapeutic agents; however, it has been documented the use of endothelin receptor antagonists and other molecules as potential alternatives.
This study aimed to develop a systematic literature review regarding the different pharmacological treatment options available for patients with scleroderma renal crisis.
Methods
Inclusion criteria
Language: English
Publication dates: From January 1990 to August 2019
Types of studies: Observational, descriptive, clinical trials, and systematic reviews.
Search: Pharmacological treatment of scleroderma renal crisis as monotherapy or combined therapy in any form of administration. The pharmacological agents included were: o Angiotensin-converting enzyme inhibitors (ACEI)
Search strategy
The study was designed based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines.9 The search was done in the following electronic scientific databases: MEDLINE PUBMED and EMBASE, using as search terms the following keywords: ("scleroderma renal crisis" OR "Acute renal failure") and MeSH terms that include "Scleroderma, Systemic", "Angiotensin-Converting Enzyme Inhibitors", "Angiotensin Receptor Antagonists", "Calcium Channel Blockers", "Endothelin Receptor Antagonists", and some specific agents as "Prostacyclin analogues" (Including "Epoprostenol", "Treprostinil", "Iloprost", "Beraprost"), "Labetalol", "Minoxidil", and "Aliskiren". Results were filtered based on the inclusion and exclusion criteria named before, including publication dates (January/1990 to August/2019), study design (descriptive studies such as case reports were excluded), and publication language (English). After the literature search was done, a manual search was conducted by checking the bibliographic references from review papers about scleroderma renal crisis.
Data collection process
Two researchers (AZ and JF) made the screening of studies in a separate way. Each one made the selection process applying the inclusion criteria. After concluding this process, results from each researcher were compared to identify similarities and differences. In the case of disparities regarding the inclusion of a study, a consensus was made between the researchers. If an agreement was not reached, a third researcher with extensive experience in Epidemiology and research methods (GQ), came to settle it.
The following information was collected from the selected studies: information about the characteristics of each study (publication year, authors, study design), the amount of patients with scleroderma renal crisis, the exposure and/or intervention, and the primary outcomes (number of patients who required temporal and permanent dialysis, and survival rate).
Quality and risk of bias
All studies included were assessed in order to identify the methodological quality and risk of bias. The quality of the studies was assessed according to the design of each reference. For clinical trials, it was assessed following the recommendations from the Cochrane Handbook for Systematic Reviews of Interventions.10 For cohort and case-control studies, the Scottish Intercollegiate Guidelines Network (SIGN) checklist was applied.11 Finally, for case-series studies, a critical appraisal tool developed by the Joanna Briggs Institute from the University of Adelaide was used.12
Meta-analysis
Based on the quantitative results available and the homogeneity of outcomes from the studies included in this systematic review, the possibility of developing a meta-analysis was assessed. However, due to the diversity of outcomes reported and the limited amount of evidence available, it was not possible to make this kind of statistical treatment to the data.
Results
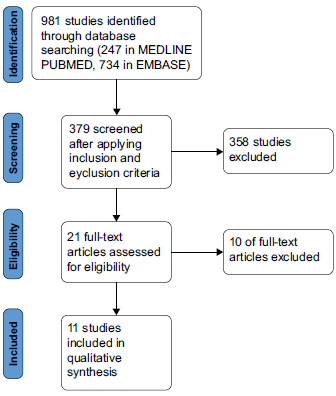
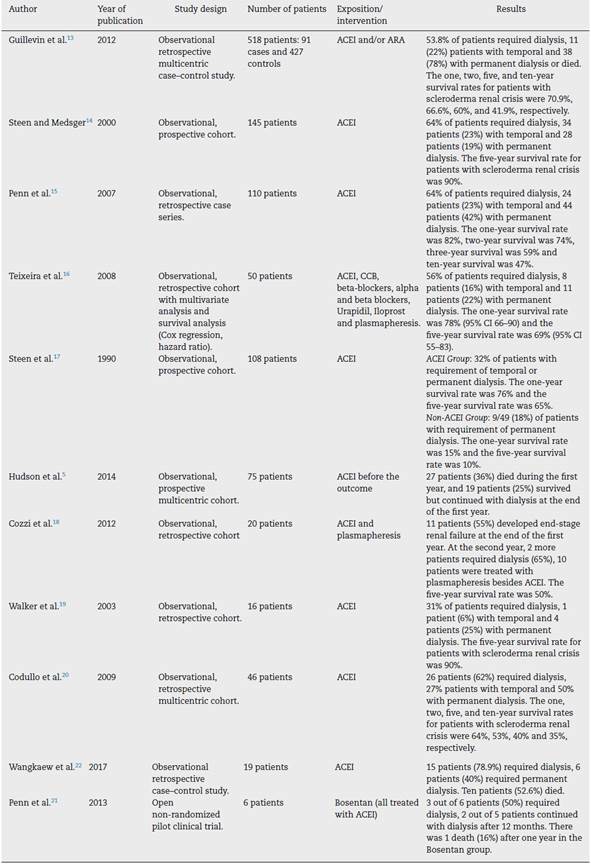
The search identified 247 studies in MEDLINE PUBMED and 734 in EMBASE. Filters were applied based on the inclusion and exclusion criteria described before, obtaining 379 studies. After assessing the references by title and abstract, 21 studies were selected for full-text assessment. Finally, 11 studies were included in the review (see Fig. 1). The characteristics of the studies included are described in Table 1.
The main reasons for excluding studies were: not mentioning the pharmacological agent used for the treatment of scleroderma renal crisis, or not reporting as outcomes the requirement of temporal or permanent dialysis, or not reporting the survival rate, or preliminary reports with the final study already published.
A total of 1113 patients were included, the study conducted by Guillevin et al. contributed with most of the patients (518 patients). The data shows that 824 patients were women (74.03%), which is consistent with the gender distribution reported for systemic sclerosis. The mean age at the diagnosis of scleroderma renal crisis was 52.4 years, with the study of Walker and colleagues reporting the most extreme ages. More than half of patients with scleroderma renal crisis had diffuse systemic sclerosis, approximately 56% (data was missing from the study of Steen and colleagues from 1990, regarding the proportion of patients with the diffuse form of the disease).
After developing the search and analyzing the information of 11 studies, it could be concluded that most studies available are observational, descriptive case-control, or cohort. Only one study had a different methodological design as one pilot study was conducted comparing the effectiveness of Bosentan in the management of patients with scleroderma renal crisis. All analyzed studies used ACEI as exposition, case definition and/or comparison in a clinical trial. Primary outcomes assessed in the studies were the requirement of beginning dialysis as temporal or permanent treatment, and one, two, five, or ten-year survival.
In a retrospective, multi-centric case-control study published by Guillevin and colleagues, the aim was to describe the characteristics, treatments, prognosis, and outcomes of patients with scleroderma renal crisis. They found that renal crisis was more frequent in women, usually during the first three years after the diagnosis of systemic sclerosis and was more frequent in patients with diffuse systemic sclerosis than in patients with limited diseases (78 patients (85.7%) vs. 145 patients (34%); p> 0.001). Regarding the treatment, 83 out of 91 cases (91.2%) were treated with ACEI, and 18 cases (19.8%) received ARA; 23 patients did receive an ACEI before the beginning of the renal crisis; 9 out of 23 patients (39.1%) that received an ACEI before the beginning of the renal crisis died vs. 28 out of 68 patients (41.2%) that received Bosentan; 14 out of 23 patients (60.1%) treated with ACEI required dialysis; 7 patients did not receive ACEI or ARA, and 3 of them died during the following month after the diagnosis of renal crisis; 51 patients (56%) received both ACEI and ARA. Regarding the control group, 82 patients (19.2%) received ACEI. The clinical outcome of this group of patients was poor, as 49 patients (53.8%) required dialysis, which was temporary for 11 patients, while 38 required permanent dialysis or died. 37 patients (40.7%) died, compared to 46 patients (10.8%) from the control group (p<0.001). Considering mortality cases, 24 patients were in renal replacement therapy or did require it at some point during the disease. Deaths were more frequent in patients who never recovered renal function. Thirteen patients that never required dialysis died. One, two, five, and ten-year survival rates of patients with scleroderma renal crisis were 70.9%, 66.6%, 60%, and 41.9%, respectively. The mean survival time after the diagnosis of renal crisis was 99 months. The dialysis-free survival rates after one, two, and five years were 55.3%, 44.4%, and 33.7% respectively. The outcomes were better in patients with arterial hypertension (73.8%) compared to normotensive patients (58%).13
Another prospective cohort study published by Steen and Medsger aims to assess the risk factors, natural history, and outcomes of patients with scleroderma renal crisis treated with ACEI. They assessed all patients with systemic sclerosis from the University of Pittsburgh between 1979 and 1996. From 807 patients with diffuse systemic sclerosis, 145 developed Scleroderma renal crisis and received ACEI (The specific ACEI, dose, and administration were not mentioned).14 Patients were divided into 4 groups based on their outcomes:
Those who did not require dialysis during the first year after the diagnosis of renal crisis, considered as a favorable outcome.
Those who required temporal dialysis (required dialysis and it was suspended at least for a year).
Those who required permanent dialysis.
Those who died early (defined as those patients who died during the first six months after the diagnosis of renal crisis).
75% of patients had systemic sclerosis symptoms for at least four years, the mean age of diagnosis was 50 years, 75% of patients were women, 92% were Caucasian, and 88% had diffuse systemic sclerosis.14
Considering renal function, of the group of patients that did not require dialysis (55 patients (38%)), two patients presented progressive worsening of renal function, requiring dialysis after 4 and 6 years, respectively. All 55 patients continued receiving ACEI, and one patient developed malignant hypertension and renal failure despite using Captopril. Thirty-four patients (23%) received temporal dialysis that was suspended between 2 and 18 months after the beginning of the renal crisis. All 34 patients continued treatment with ACEI. Thirty-two patients (3 from the non-dialysis group and one from temporal dialysis) received permanent dialysis (9 with peritoneal dialysis and 23 with hemodialysis). Twenty-eight patients died from early disease (19%) after a mean period of 3 months from the diagnosis. Most patients from this group were men (33%), older (54 years vs. 46 years) and had higher initial levels of serum creatinine. Of them, 64% required dialysis. Regarding survival, it was similar in patients from the non-dialysis group and from the temporal dialysis group. The cumulative survival rate after five years was 90% and 80-85% after eight years.14
A study developed by Penn and colleagues described the clinical and pathological characteristics of patients with scleroderma renal crisis, and correlated them with renal outcomes and mortality. A total of 110 patients were included, 24 patients (22%) with limited form and 86 patients (78%) with the diffuse form of systemic sclerosis. The calculated frequency of renal crisis in this center was 2% for patients with limited systemic sclerosis and 12% for patients with diffuse systemic sclerosis. The mean age at diagnosis was 50.7 years (range 24-80 years); 79% were women; the mean duration of systemic sclerosis at the diagnosis of renal crisis was 7.5 months (range 0-200 months); 69 patients (66%) developed renal crisis during the first year of diagnosis of systemic sclerosis. Patients with normotensive renal crisis were not included in this study. Most patients received ACEI, except for two patients (one was pregnant and treated with Methyldopa and a beta-blocker, and the other patient was treated with a beta-blocker and a CCB). In at least 46 patients, intravenous prostacyclin analogs were given (there was no information about the specific agent, dose or duration of treatment). Information regarding the need for renal replacement therapy was available in 106 out of 110 patients. Of them, 38 patients (36%) did not require dialysis. From this group, only 3 required dialysis later (one due to nephrectomy for treatment of renal carcinoma after 10 years of presenting scleroderma renal crisis; other with progressive worsening of renal function that required dialysis 7 years after presenting scleroderma renal crisis; the last one with requirement of dialysis after 8 years of presenting renal crisis). 24 patients (23%) required dialysis at the moment of the diagnosis, with posterior recovery of renal function, allowing the suspension of dialysis (2 of them required dialysis later on: 1 was in dialysis for 13 months with no dialysis for 6 months and reinitiated it, and the other was in dialysis for 18 months and after 7 years from diagnosis of renal crisis required dialysis for 10 days). Forty-four patients (42%) required dialysis at the moment of diagnosis and never recovered renal function (43 patients) or refused the renal replacement therapy and died (3 patients). Nineteen patients died during dialysis, and three received renal transplant. The mean time for recovery of renal function (discontinuation of dialysis) was 11 months (range 1-34 months). After 24 months, it was less frequent the recovery. 63% of patients required dialysis at the beginning of renal crisis, and 33% of survivors still received dialysis after five years. From patients that required dialysis at the beginning of renal crisis, 35% were able to discontinue the therapy. 7% of patients that required dialysis and were able to recover renal function needed to reinitiate dialysis later on.15
Regarding mortality, 44 patients died after the renal crisis. The one, two, three, and ten-year survival rates were 82%, 74%, 59%, and 47%, respectively. Deaths were more frequent in the group of patients who received dialysis and never recovered renal function.15
The study published by Teixeira and colleagues described the presentation and outcomes of patients with scleroderma renal crisis. They included patients with renal crisis defined as a rapidly-progressive oliguric renal failure without other explanation, and/or rapidly progressive arterial hypertension that occurs during systemic sclerosis. Normotensive renal crisis was defined as an increase of more than 50% of baseline serum creatinine or more than 20% above the top limit of normal creatinine, and one of the following five characteristics:
Proteinuria with 2 or more +.
Hematuria with 2 or more +, or 10 or more red blood cells per field.
Thrombocytopenia below 100,000/nm platelets.
Hemolysis (anemia, schistocytes, increased reticulocyte count).
Renal biopsy with findings suggestive of renal crisis.
Patients were divided into 4 groups based on their outcomes: no dialysis, temporal dialysis, permanent dialysis, or death. From 50 patients, the mean age was 53.3 years, the women:men ratio was 2.5. Forty-three patients had diffuse systemic sclerosis. Ten patients were receiving low dose ACEI at the moment of diagnosis of renal crisis. Forty-seven patients (94%) received an ACEI. Of them, ten were already receiving ACEI (doses were increased). From 37 patients, 2 had nor-motensive renal crisis, and 14 died. Only four patients received ACEI alone, 23 received ACEI + CCB, 5 received ACEI + Beta-blocker, 2 with ACEI + alpha and beta-blocker. In 5 patients receiving ACEI + CCB, Urapidil was included. Plasmapheresis was required in 5 patients. Only one patient needed Iloprost. After 47 months of follow-up, 28 patients (56%) required dialysis. Temporal dialysis was required in 8 patients (the mean duration of therapy was nine months), and permanent dialysis was required in 11 patients. A total of 9 patients (18%) died during dialysis. No patient received a renal transplant. One-year survival rate was 78% (95% CI = 66%-90%), and five-year survival was 69% (95% CI= 55%-83%). The multivariate analysis found that an age >53 years at the moment of diagnosis of renal crisis, and normotensive renal crisis were independent predictors of lower chronic dialysis-free survival. A limitation of this study was the origin of the information, as cases were obtained from previous reports of renal crisis cases.16
Another study published in 1990 assessed the outcomes of patients with scleroderma renal crisis before and after the introduction of ACEI as treatment, and identified risk factors associated with poor outcomes. The renal crisis was defined as an incidental increase in diastolic pressure above 110 mmHg, accompanied by at least two of the following criteria:
Keith-Wagener grade III or IV changes in the ocular fundus.
Seizures.
Proteinuria.
Hematuria.
Microangiopathic hemolytic anemia.
Azotemia or hyperreninemia.
Patients without diastolic hypertension were included if they presented rapidly progressive renal failure without other explanation and at least two of the clinical criteria mentioned before. Fifty-three patients with scleroderma renal crisis did not receive ACEI, and 55 patients received ACEI: 47 patients received Captopril, 1 received Enalapril. Seven patients developed toxicity to Captopril (Rash), requiring a change to Enalapril. For the analysis, patients were divided into two groups: those who received ACEI as treatment, and those who did not receive it. They were also divided based on the outcomes: favorable (those with a survival of at least six months after the beginning of the renal crisis, and not requiring dialysis, or successful recovery of renal function) or unfavorable (survival lower than six months or requirement of permanent dialysis), obtaining the following results:
Received ACEI + favorable outcome: thirty-one patients. Twenty survived six months or more, and 11 survived and required temporal dialysis (3-15 months).
Did not receive ACEI + favorable outcome: four patients. All of them survived more than six months without dialysis.
Received ACEI + unfavorable outcome: twenty-four patients. Fifteen survived less than six months, and nine required permanent dialysis.
Did not receive ACEI + unfavorable outcome: forty-nine patients. Forty survived less than six months and nine required permanent dialysis.
Eighteen percent of patients that were not exposed to ACEI required permanent dialysis. The other 82% of patients survived less than six months and did not have a registry of requiring renal replacement therapy. Of 53 patients that did not receive ACEI, one-year survival was 15%, and five-year survival was 10%. Instead, patients that received ACEI had a one-year survival of 76% and a five-year survival of 65%.17
Hudson and colleagues published a study in 2014 in which they determined the outcomes of patients with scleroderma renal crisis and compared the outcomes of patients that received ACEI vs. those that did not receive ACEI before the onset of renal crisis. One year after the case was identified, a follow-up was made to establish if the patient required dialysis, or if the patient died. The final sample included 75 new cases with scleroderma renal crisis, 70 of them were hypertensive, and five were normotensive. The mean age at diagnosis was 53 years, 67% were women, 77% were Caucasian, and 75% had diffuse systemic sclerosis. Sixteen patients (21%) received ACEI before the onset of renal crisis, and they had higher probabilities of presenting normotensive renal crisis. Those exposed to ACEI before the onset of the renal crisis were older (57 years vs. 51 years), it was less common in women (50% vs. 71%) and they were exposed to lower doses of glucocorticoids compared to patients not exposed to ACEI (9.2mg/day vs. 18.2mg/day of prednisone). Twenty-seven patients (36%) died during the first year, and 19 patients (25%) survived and continued with dialysis at the end of the first year. The cumulative incidence rate of death during the first year after the onset of the renal crisis in patients exposed to ACEI was 1.56 (95% CI = 0.68-3.57) compared to those not exposed to ACEI. There were no differences regarding the rate of dialysis during the first year (cumulative incidence rate = 0.94, 95% CI = 0.43-2.05). After adjusting based on the initial prednisone dose, the risk of death in patients exposed to ACEI before the onset of renal crisis was more than twice, compared to those not exposed, and the difference was statistically significant (HR: 2.42, 95% CI: 1.02-5.75, p< 0.05). The outcomes after the diagnosis of the renal crisis were poor, with 60% of death, 25% continued to require dialysis after the end of the first year, and 15% recovered renal function. A possible explanation of the higher risk of mortality in patients exposed to ACEI could be that the medication may camouflage the development of the renal crisis. Also, the presence of systemic hypertension and cardiac comorbidities could contribute to this behavior. It is possible that patients treated with ACEI for hypertension during the onset of systemic sclerosis, may present an undiagnosed renal crisis, and that treatment could have solved it. Renal biopsy was made in 10 patients. The samples were not examined in the same institution; however, all of them were diagnosed with renal crisis by the pathologist.5
In a study developed by Franco Cozzi and colleagues, they assessed the prognosis of patients with scleroderma renal crisis. It was a cohort of patients with systemic sclerosis between 1980 and 2005. Of 606 patients with diagnosis of systemic sclerosis, 20 patients (3.3%) developed renal crisis, defined as an abrupt onset of rapidly progressive renal failure (two-fold increase of serum creatinine levels above the baseline level, without other explanation) and/or malignant hypertension (systolic pressure above 160 mmHg or diastolic pressure above 110 mmHg measured in two opportunities). 7 patients with renal crisis had microangiopathic hemolytic anemia. After the diagnosis of renal crisis, all patients continued their established treatment and increasing doses of ACEI (Captopril, Enalapril, and Ramipril). Three patients did not tolerate high doses of ACEI and developed hypotension without improvement of renal function. These three patients and other 7 (suffering from microangiopathic hemolytic anemia) required treatment with plasmapheresis, aside from ACEI. Outcomes assessed in this study include the development of end-stage renal failure (requirement of permanent dialysis), survival, mortality, and mortality due to renal crisis. Of 20 patients who developed renal crisis, 14 were women, and 6 were men. The mean age at diagnosis of systemic sclerosis was 45.5 ± 14.9 years, and for the diagnosis of the renal crisis was 49.0 ±12.1 years. The mean duration of systemic sclerosis at the onset of renal crisis was 3.7 ±4.8 years. Sixteen patients had diffuse systemic sclerosis with a mean Rodnan score of 20.5 (range 15-32), and four patients had limited disease (mean Rodnan score: 5.5; range: 5-7). Twelve patients had interstitial lung disease, six patients with cardiac compromise, and 13 patients with gastrointestinal compromise. At the moment of diagnosis of renal crisis, five patients were using D-penicillamine, 4 cyclosporine, 1 cyclophosphamide, 1 azathioprine, and 1 methotrexate. Ten patients were using low-dose glucocorticoids (7 with doses below 15 mg/day, and 3 with a dose of 25 mg/day). Also, 15 patients used oral vasodilators, and 5 used intravenous Prostanoids. During the first year of diagnosis of renal crisis, 11 patients (55%) developed end-stage renal failure, and six patients (30%) died due to complications of renal crisis. The five-year survival rate was 50%, and renal crisis-related mortality was 35%. Ten patients were treated with plasmapheresis and ACEI, due to intolerance to high doses of ACEI or for development of microangiopathic hemolytic anemia. The duration of plasmapheresis varied between 1 and 10 months, with a mean number of 28 ± 12 sessions. After the first year of diagnosis of renal crisis, 7 out of 10 patients preserved or recovered enough renal function to prevent the need of dialysis, two patients developed end-stage renal disease, required permanent dialysis and received a renal transplant. One patient died as a consequence of complications from the renal crisis. In this group of patients, the five-year survival since the onset of renal crisis was 70%, and renal crisis-related mortality was 10%. Two more patients that initially improved died of cancer after 15 and 18 months, respectively. These results confirm the poor prognosis of scleroderma renal crisis, as 55% of patients developed end-stage renal failure, and 30% died during the first year after the diagnosis. Short-term prognosis has improved, but long term prognosis remains low.18
Another study published by J.G. Walker and colleagues in 2002, determined the frequency and outcomes of patients with scleroderma renal crisis. They also determined the mean duration of the disease since the onset of this complication, the clinical and serological predictors of the development of renal crisis, and the pharmacological therapy used. They found 16 patients; 11 were women; the mean time to the onset of renal crisis since the appearance of the first symptom of systemic sclerosis was 15 months. At the moment of the onset of renal crisis, most patients (94%) presented arterial hypertension, 56% cardiac failure, and 81% microangiopathic hemolytic anemia. All of them presented rapidly progressive renal failure with hematuria, proteinuria, and the presence of cellular cylinders. The mean age of onset of systemic sclerosis in patients with renal crisis was 54.5 years (range: 47.6-61.3). Renal biopsy was done in 7 patients, and an autopsy was done in 3 patients. The outcomes were poor in these patients despite receiving aggressive anti-hypertensive treatment. In 13 patients, ACEI was given (in 2 patients, it was suspended due to hypotension). Another patient received Captopril, and developed a severe cutaneous reaction, requiring the suspension of the medication. Five patients died within days or weeks after the development of renal crisis as a direct consequence of it. The other five patients required permanent dialysis (2 required renal transplant) and serum creatinine returned to normal levels in 2 patients. One patient was able to suspend dialysis after six months.19
Codullo and colleagues developed a multi-centric retrospective study to describe the characteristics of Italian patients with scleroderma renal crisis, with a special interest in the serological profile. A total of 46 patients, with 38 being women and eight men were included. Forty patients presented a diffuse disease. The mean age at the beginning of systemic sclerosis was 52.8 years, and the mean age at the diagnosis of renal crisis was 55.4 years. Renal biopsy was made in 5 patients with typical findings of renal crisis in the pathology. Patients were divided into:
Those with a diagnosis of renal crisis during the first 18 months since the beginning of the disease.
Those with diagnosis between 18 and 48 months since the beginning of the disease.
Those with diagnosis after 48 months since the beginning of the disease.
62% of cases with renal crisis ccurred during the first 18 months, 18% between 18 and 48 months, and 20% after 48 months. Patients with renal crisis before 18 months since the diagnosis of systemic sclerosis were older compared to the patients who developed the renal crisis after 48 months. The treatment strategy used was available for 42 patients. Thirty-three patients (78%) received an ACEI as soon as the diagnosis of renal crisis was made, 26 patients (62%) required dialysis. Dialysis was suspended in 7 out of 26 patients (27%). Three patients received renal transplant after a mean period of 140 ± 54 months since the onset of renal crisis. One patient developed pulmonary arterial hypertension and required the use of a non-selective endothelin-1 receptor antagonist. The one, two, five, and ten-year cumulative survival rates were 64%, 53%, 40%, and 35% respectively. 80% of patients developed renal crisis during the first four years after the diagnosis of systemic sclerosis.20
Wangkaew and colleagues published a case-control study in 2017, determining the prevalence, risk factors, and outcomes in Thai patients with scleroderma renal crisis. They included patients with systemic sclerosis that fulfilled the ACR classification criteria from 1980, by reviewing clinical records between January 1990 and December 2015. Cases of scleroderma renal crisis were identified based on the International Scleroderma Renal Crisis Study Criteria. Controls were selected from consecutive patients with systemic sclerosis without renal crisis from the database. Controls were matched based on a disease duration of ±1 year. The ratio of scleroderma renal crisis and control patients was 1:4. Clinical data obtained from the clinical records were: age, gender, scleroderma subtype, disease duration, organ involvement, laboratory results, medications used, and outcome. Laboratory results and current medications were recorded from the first date since the diagnosis of scleroderma renal crisis. In the control group, these variables were recorded and time-matched for the disease duration of the cases. The definition of scleroderma renal crisis was based on that of the International Scleroderma Renal Crisis Study Group, and patients were classified into two groups:
Hypertensive scleroderma renal crisis: presence of any of the following situations as systolic blood pressure >140 mmHg, or diastolic blood pressure >90 mmHg, or rise in systolic blood pressure >30 mmHg compared to baseline, or rise in diastolic blood pressure >20 mmHg compared to baseline, plus one of the following features: increase in serum creatinine >50% over baseline or serum creatinine >120% of the upper limit of normal value, hematuria >2+ by dipstick or >10 red blood cells per field, thrombocytopenia <100,000 platelets/mm3, presence of schistocytes or increase in the number of reticulocytes or hypertensive encephalopathy.
Normotensive scleroderma renal crisis: presence of increased serum creatinine >50% over baseline or serum creatinine >120% of the upper limit of normal value, hematuria >2+ by dipstick or >10 red blood cells per field, thrombocytopenia <100,000 platelets/mm3, presence of schistocytes or increase in the number of reticulocytes or hypertensive encephalopathy.22
A total of 637 patients with systemic sclerosis were assessed. Nineteen patients (3.13%) developed renal crisis: 12 hypertensive and 7 normotensive. As controls, 76 patients were included. Considering the renal crisis, nine patients (47.4%) were men, the mean age at diagnosis of systemic sclerosis was 56.2 ±13.8 years, the mean disease duration was five months (range: 3-22 months), and 17 patients (89.5%) had diffuse systemic sclerosis. Regarding the control group, 25 patients (32.9%) were men, the mean age at diagnosis of systemic sclerosis was 50.4 ±11.2 years, and 61 patients (80.3%) had diffuse systemic sclerosis. Compared to controls, patients with renal crisis had a higher proportion of systemic sclerosis-associated organ involvement, and required higher doses of glucocorticoids. The results of multivariate conditional logistic regression analysis identified as independent risk factors for developing renal crisis the following: presence of digital gangrene, current glucocorticoid dose >15 mg/day, serum albumin <3 mg/dl, and cardiac involvement. Regarding the outcomes of patients with renal crisis, during a median follow-up period of one month after the diagnosis, 12 patients (63.2%) received ACEI, and 15 patients (78.9%) required dialysis. In 3 patients, ACEI was not used due to concurrent hypotension. From patients that required dialysis, 6 (40%) required the therapy for more than three months and then required long-term dialysis. Three patients (20%) that required dialysis were lost to follow-up within three months after dialysis. Ten patients (52.6%) with renal crisis died. The median time from renal crisis diagnosis to death was 17.5 days (range: 3.5-40.2). Limitations of this study include that the number of patients with renal crisis was small, affecting the statistical significance. Also, the median duration of patients follow-up was short, affecting the assessment of long-term outcomes.22
The study published by Penn and colleagues in 2013 is the only pilot study found. The aim was to measure the expression of endothelin-1 and endothelin receptors A and B in patients with scleroderma renal crisis and assess the possibility and safety of adding the treatment with Bosentan during six months to an ACEI treatment during the first six weeks since the diagnosis of renal crisis. The rationale to use Bosentan as part of the treatment for renal crisis is that this agent has demonstrated to be effective in the management of other vascular complications of systemic sclerosis including digital ulcers and pulmonary arterial hypertension. These complications and renal crisis have important microscopic similarities because of the clinical success of blocking the activity of endothelin-1 in two of these vascular manifestations (pulmonary hypertension and digital ulcers). Scleroderma renal crisis was defined as recent onset arterial hypertension above 150/85 mmHg measured in at least two opportunities in 24 h or the development of renal function impairment defined as a reduction of at least 30% of glomerular filtration rate. The following characteristics were considered as evidence that supports the diagnosis of renal crisis if they were present: microangiopathic hemolytic anemia, hypertensive crisis retinopathy, recent onset hematuria, acute pulmonary edema, oliguria or anuria, renal biopsy with defining changes. The cases included in this study were confirmed between 2000 and 2004, in which 27 patients had blood exams and renal biopsy available, and six more patients were included in the "Bosentan in Renal Disease-1" (BIRD-1) trial. In order to be able to include the results from the cases included in the BIRD-1 trial in the context of other cases of renal crisis treated in the same center, a comparative analysis of cases of renal crisis was made, and 49 cases were taken as a comparator. The outcomes assessed were mortality and renal function at 6 and 12 months (including the need of dialysis). All patients were treated with Bosentan 62.4mg twice a day, and then the dose was increased to 125 mg twice a day during another 5 months along with an ACEI.21
Regarding the six patients included in the study, 100% were Caucasian. One patient was receiving immunomodulatory therapy before the onset of renal crisis (mycophenolate mofetil). Two patients were treated with glucocorticoids (one with high doses due to suspicion of glomerulonephritis and the other with low doses of prednisone). None of the patients received ACEI and ARA before the onset of renal crisis. One patient receiving Bosentan withdraw from the study, due to the need for dialysis after ten days of treatment. Another patient discontinued the Bosentan after five weeks since the beginning of the treatment.21
Regarding the results, 3 out of 6 patients required dialysis, and two patients continued on dialysis after 12 months since the diagnosis. 34 out of 49 patients from the cohort used as a comparison, needed dialysis at some point during the follow-up, and 25 patients remained on dialysis after 12 months since the diagnosis. Regarding the one-year mortality, 1 out of 6 patients (16%) of the group that received Bosentan died, and 6 out of 49 patients (12%) of the cohort of comparison died. Based on this, the authors concluded that there were no significant differences in mortality rates or need for dialysis between the group that received Bosentan and the control group. Plasmatic levels of endothelin-1 were found increased in those patients with renal crisis, compared to healthy controls (the mean level in healthy controls was 0.5 pg/ml vs. 1.48 pg/ml in patients with renal crisis). The mean levels of endothelin-1 in the BIRD-1 cohort were not significantly different from the control group. Patients treated with Bosentan had increased levels of endothelin-1. No significant adverse events were registered. In conclusion, this study confirms the potential role of endothelin-1 and its receptor in the pathophysiology of sclero-derma renal crisis and gives information regarding the safety of the use of non-selective endothelin receptor antagonists combined with standard therapy in the context of patients with renal crisis.21
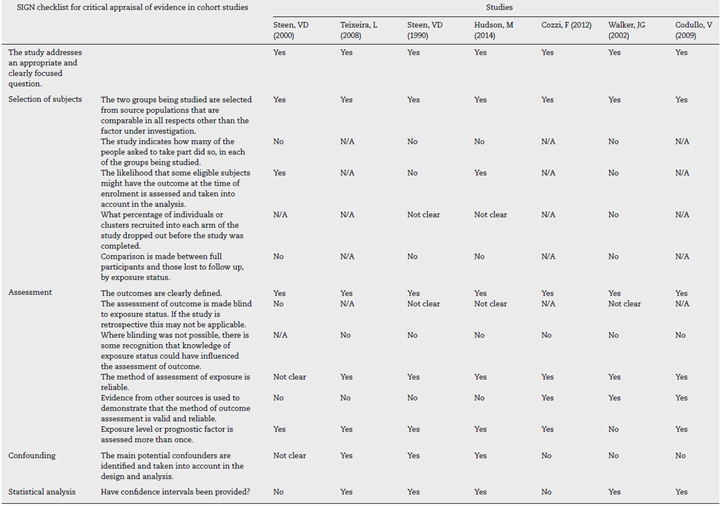
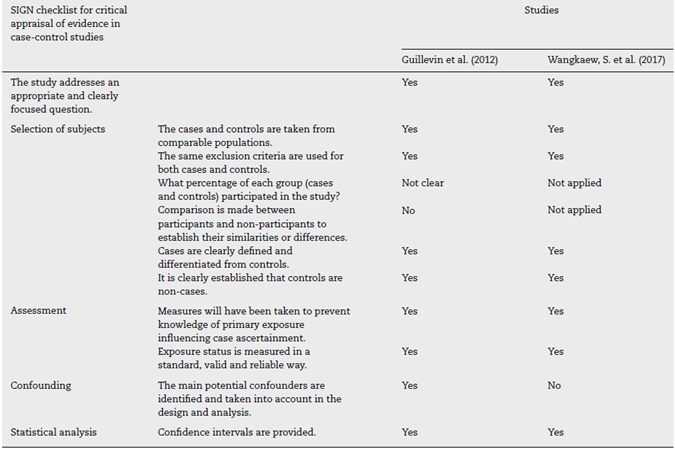
The quality of evidence assessment for every study found the following aspects:
Regarding clinical trials, the only one available is an open non-blinded trial, which gives a higher risk of selection, allocation and performance bias due to the design of the study. There is an unclear risk of attrition bias, as no information is given about the strategy used in case of loss to follow-up or withdrawal of participants from the study.
The quality assessment of cohorts using the SIGN checklist is presented in Table 2. The overall quality of the studies shows that they developed an adequate research question, and the target populations for the selection of the participants were adequate. However, they did not give information regarding the amount of patients they asked to participate, and the comparison between participants and no-participants. In general, the studies clearly defined the outcomes, the methods of measurement, and in some cases, references to support the reliability of the methods used. However, no study gives information about the blindness of exposure status. Another weakness identified is that only few studies take into account the presence of potential confounders during the design and analysis.
The quality assessment of case-control studies using the SIGN checklist is presented in Table 3. In general, the case-control studies included in the systematic review had a good quality. The only weakness was that they did not give information about the percentage of people who participated from the overall population that was asked to participate in the study. Also, no comparison was made between the participants and non-participants. Also, the study of Wangkaev and colleagues did not mention that they considered potential confounders during the design and analysis.
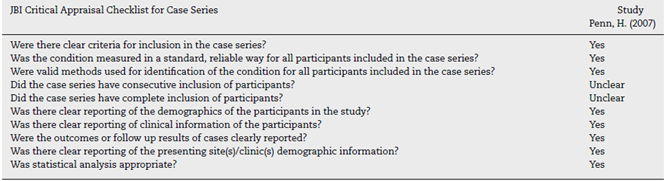
The quality assessment of case series made using the critical appraisal tool developed by the Joanna Briggs Institute from the University of Adelaide is presented in Table 4. The only study from this category, in general, meets the criteria to be considered to have an adequate quality. However, there was no enough information regarding the consecutive or complete inclusion of participants.
Discussion
Scleroderma renal crisis is a severe and uncommon complication from systemic sclerosis, that still presents a low survival rate at one, two, five and ten years, with a high percentage of patients requiring temporal or permanent renal replacement therapy.
It was found that approximately 54.9% of analyzed patients required temporal or permanent dialysis. Approximately, 6-27% of patients required temporal dialysis, and 19-78% of patients required permanent dialysis. The ranges are wide, which reflects the insufficient data samples available from the studies, a situation that does not allow the development of more accurate statistical analyses. However, the results show a clear correlation between the development of the renal crisis and the requirement of permanent dialysis.
Regarding survival, the analysis shows relevant data that could be synthesized as follows: one-year survival was 64-84%, two-year survival was 53-74%, five-year survival was 40-90%, and ten-year survival was 35-17%. It was evident that ten-year survival was significantly reduced compared to the rest. During the analysis, no specific justification was found in order to explain this behavior. However, this may be explained by the type of chronic disease (its progression, organ involvement), and the natural aging process.
The analysis shows that 91% of the analyzed patients received pharmacological therapy at the moment of the diagnosis. Consistent with the guideline recommendations, the most frequently prescribed agents were ACEI (88.75% = 81.4% as monotherapy, 7.35% combined with other agents). The most frequent combination observed was ACEI + ARA (4.6%). All the references described before, point toward the benefit of applying ACEI due to the improved survival rates compared to those patients that did not receive the therapy. This evidence supports the statement that the introduction of this medication in the management of renal crisis changed the natural history of the disease based on short-term survival. However, the use of this therapy was not enough in all cases to restore or maintain renal function without the requirement of dialysis. The effectiveness of ACEI therapy is associated with the interruption of the renin-angiotensin-aldosterone system, reducing the angiotensin-II vasoconstriction, and reducing the degradation of bradykinin, which increases renal vasodilation.23
An important observation was that the previous use of ACEI before the onset of renal crisis appears to be a risk factor for mortality. It could be explained by an early camouflage of the development of renal crisis, which could be initially misdiagnosed as primary systemic arterial hypertension. This situation supports the recommendations presented in recent reviews, in which the prophylactic prescription of ACEI is not supported, due to increased risk of harm. However, more evidence is required to develop a stronger recommendation.23
Unfortunately, not all studies named the specific ACEI used; however, the most frequently used was Captopril, followed by Enalapril. Captopril has been used as ACEI of choice because it has a rapid onset of action, short half-life, and allows rapid dose escalation if it is needed.23
Another medication that shows great potential to increase the survival rate of patients and reduce the requirement of renal replacement therapy was Bosentan. However, the evidence available is limited, and the number of cases analyzed in this review was small (0.5% of patients) to be able to give definite conclusions. More studies are required in this field.24,25
The rest of the pharmacological agents used such as ARA, CCB, and adrenergic blockers seem to work in the treatment, but in combination with ACEI. In the case of ARA, the benefits of its use as first-line therapy remain unclear as some authors reported a limited benefit, while others state that the use of ARA alone is not able to control the disease and is associated with a higher risk of renal failure. Initial reports indicate a benefit of combining ACEI and ARA; however, recent evidence discourages this combination due to the risk of adverse events such as hyperkalemia and worsening of glomerular filtration rate.25
Studies about the use of prostacyclin analogs for the treatment of scleroderma renal crisis were not found. The studies available aim to establish the effect of the chronic use of these medications in patients with systemic sclerosis. The evidence available suggests that the use of prostacyclin analogs had reduced the incidence of renal crisis in patients with systemic sclerosis.25 This statement is supported by the study published by Caramaschi and colleagues in 2012, which aims to evaluate the incidence of severe vascular complications as scleroderma renal crisis in patients receiving cyclical intravenous Iloprost during at least three years. In 115 patients with systemic sclerosis, none of them developed renal crisis.29 However, more studies are required to support the use of prostacyclin analogs as prophylaxis against this severe complication, and also the potential use as treatment in order to develop a stronger recommendation.
In recent years, no observational or analytical studies have been published about the use of new therapeutic agents for the treatment of this entity, in order to be included in the review. However, a recent review published by Zanetta and colleagues in 2018, gives information about the role of the complement system in the pathophysiology of scleroderma renal failure, as immunofluorescence studies made on kidney biopsies of patients with this disease show deposits of C1q, C3b, C4d, and C5b-9 in the endothelium of renal arterioles and glomeruli.25 Okrój and colleagues published a study in 2016 regarding the expression of complement biomarkers in systemic sclerosis, observing that patients with scleroderma renal crisis express a different pattern of complement activation markers compared to patients with systemic sclerosis and absence of renal involvement. They present higher amounts of C4d and lower levels of C3bBbP and sTCC. Both C3bBbP and sTCC are markers of hemolytic activity, indicating that complement activation is present during a scleroderma renal crisis.26
Two case reports have been published regarding the potential use of Eculizumab (a humanized monoclonal antibody against C5). One report was published by C.P. Thomas and colleagues, where they describe a case of a 46-year-old woman with non-specific interstitial lung disease, who was presenting worsening dyspnea over the last year, and one month with swelling of extremities and proximal muscle weakness. Physical examination showed arterial hypertension, reduced breath sounds, and proximal weakness. During admission, several laboratory tests were performed, showing platelet consumption, peripheral smear with schistocytes, decreased haptoglobin, and high levels of LDH consistent with hemolysis. Also, increased serum creatinine levels, urinalysis with the presence of blood and proteins, positive ANA (>1:2560) with speckled pattern, positive PM-ScL-100 and RNA polymerase III antibodies, and hypocomplementemia. The initial diagnosis was thrombotic thrombocytopenic purpura, which was treated with glucocorticoids and plasmapheresis. However, renal function worsened, and hemolysis was also present. Finally, given the presence of interstitial lung disease, positive capillaroscopy for scleroderma pattern, muscle weakness, and the autoantibodies profile, the suspected diagnosis was scleroderma polymyositis overlap syndrome, with ongoing scleroderma renal crisis. As glucocorticoids could worsen the renal crisis, they were tapered, and Enalapril with Aliskiren was given, without improvement. Due to consistent complement consumption, 900 mg of Eculizumab were given. After 24 h, signs of hemolysis were solving, and after a week, renal function and blood pressure were improving.27 Devresse and colleagues reported another case in 2016, where they describe a case of a 28-year-old pregnant woman (28 weeks) that was admitted in the emergency department due to severe arterial hypertension, signs of thrombotic microangiopathy and acute renal failure. She had a previous diagnosis of systemic sclerosis. Laboratories showed severe thrombocytopenia, microangiopathic hemolytic anemia, normal liver enzymes levels, increased serum creatinine, hypocomplementemia, and urinalysis with evidence of gross proteinuria. Cesarean delivery was performed, followed by lisinopril, nicardipine, and plasmapheresis. Renal function was decreased until anuria was present, requiring dialysis. This behavior ruled out preeclampsia. Ultrasound showed renal hypoperfusion. Renal biopsy was made, showing severe vascular changes, necrosis, glomerular ischemia, and complement deposits on vascular endothelium. A diagnosis of scleroderma renal crisis was made. After 18 days, they decided to initiate Eculizumab, achieving good control of arterial pressure and recovery of renal function. However, the patient suffered new-onset cardiac failure followed by acute pulmonary edema and cardiac arrest. She died despite resuscitation efforts.28 Both experiences show a potential benefit of using this agent as therapy for scleroderma renal failure, but more research is needed.
Based on the results and the discussion presented above, the following diagram was built regarding the pharmacological management of scleroderma renal crisis (see Fig. 2).
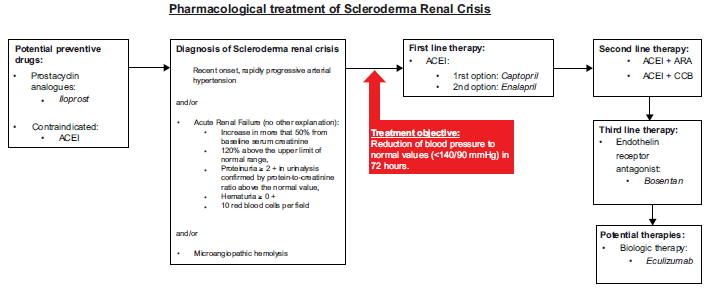
Fig. 2 Pharmacological treatment of scleroderma renal crisis based on the evidence included during the systematic review. ACEI: angiotensin-converting enzyme inhibitors; ARA: angiotensin-receptor antagonist; CCB: calcium-channel blocker.
All studies that were included had limitations related to the number of patients included. Most studies found were observational, descriptive, and retrospective, so these studies are focused on the description of epidemiological characteristics, and they do not assess the effectiveness and safety of pharmacological treatments. Only one clinical trial was included in the review. In the studies included in this review, most did not name the specific pharmacological agent used (especially the ACEI or ARA used), the dose, or the administration route. This situation increases the necessity of more analytical studies in order to have solid evidence of the effectiveness and safety of pharmacological treatments. These limitations represent a significant challenge in the accomplishment of the objective of the review, as no significant conclusions could be stated with the evidence available.
Conclusions
This review allows the statement of the following conclusions:
Scleroderma renal crisis is a severe and uncommon complication of systemic sclerosis.
Scleroderma renal crisis is the primary renal complication in this population.
ACEI agents remain the first line of therapy in scleroderma renal crisis, especially Captopril. However, prophylactic use or the use before the onset of renal crisis is associated with higher mortality rates.
The short-term prognosis of patients with scleroderma renal crisis has improved due to the introduction of ACEI therapy, but long-term prognosis continues to be a challenge.
Renal replacement therapy is a common requirement in the treatment of these patients. This procedure is considered a high-cost intervention, which may limit the access of patients to this therapy.
Considering the actual knowledge of the pathophysiology of renal crisis, new pharmacological agents with different mechanisms of action should be used in order to increase the effectiveness of pharmacological therapy.
More studies about this disease should be promoted in order to improve the times for the beginning of the treatment.
More analytical studies and clinical trials are required in order to have solid evidence regarding the effectiveness and safety of the different pharmacological options available for the treatment of scleroderma renal crisis.











 texto em
texto em