Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that affects approximately 20-50/100,000 inhabitants worldwide.1 Current therapeutic approaches have improved the prognosis and the quality of life of the patients with this disease, (2 however, their quality of life is lower than that of the general population. (3
According to the American College of Rheumatology (ACR), neuropsychiatric syndromes associated with this disease include 19 entities. There are 12 that affect the central ner vous system (CNS), of them, 5 are considered diffuse (cognitive alteration, psychosis, acute confusional state, mood disorders and anxiety). (4
Timely diagnosis and adequate treatment can influence adherence, prognosis and the quality of life of the patients5; however, some studies demonstrate that adherence in these cases is not appropriate. (2,6,7 This could be explained by sev eral factors, such as the difficulty to accept the disease and the belief of the patients that the treatment is not necessary, the fear of the adverse effects of the drugs, the practical difficulties in obtaining the medications and the scarce communication between the doctor and the patient due to time limitations. (7-10
Adherence to treatment refers to compliance with medical recommendations on drug regimens and changes in lifestyle, including the diet and exercise agreed with the patient. (11 Treatments are usually complex and prolonged, and can pre dispose the patients not to adhere adequately. (1
Neuropsychiatric disorders in patients with SLE can reduce therapeutic compliance and thus cause reactivation of the dis ease, increased number of visits to health care centers and the consequent impact on prognosis and quality of life. Therefore, the main objective of this study was to evaluate the degree of adherence to treatment in patients with diffuse neuropsychiatric disorders of the CNS associated with SLE.
Material and methods
Patients
All patients with a diagnosis of diffuse neuropsychiatric disor ders associated with SLE, belonging to the Internal Medicine service of a third-level hospital in Ecuador were included. In total, there were 60 patients. The inclusion criteria were: meeting a diagnosis of SLE according to the Systemic Lupus International Collaborating Clinics 2012 criteria, having a diagnosis of diffuse neuropsychiatric disorders established through the MINI neuropsychiatric interview and the Mon treal cognitive assessment, being over 15 years of age and agreeing to participate in the research through an informed consent/assent process. Patients under 15 years of age and a previous neuropsychiatric disease were considered as exclu sion criteria.
Instruments
The Systemic Lupus International Collaborating Clinics 2012 criteria were used for the diagnosis of SLE, and the MINI neuropsychiatric interview and the Montreal cognitive assess ment for the diagnosis of diffuse neuropsychiatric disorders, previously conducted by the services of Internal Medicine and Psychiatry. The lupus activity was evaluated according to the Systemic Lupus Erythematosus Disease Activity Index 2000. The 8-item Morisky Medication Adherence Scale (MMAS-8), a validated indirect method which was performed in Span ish was applied for this study. The score ranges from 0 to 8, considering a value of 8 as high adherence, 6-7 as medium adherence, and <6 as low adherence. (12
Procedure
A descriptive cross-sectional study that evaluated the degree of adherence to treatment was conducted. This study was carried out from October 2017 to May 2018. Patients with a previous diagnosis of diffuse neuropsychiatric disorders of the CNS associated with SLE were evaluated in the outpatient clinic of the Internal Medicine service. An informed consent/assent process was carried out and sociodemographic and clinical characteristics were collected. Next, the assess ment of the adherence to treatment was performed with the MMAS-8, which lasted approximately 10 min for each patient.
Results
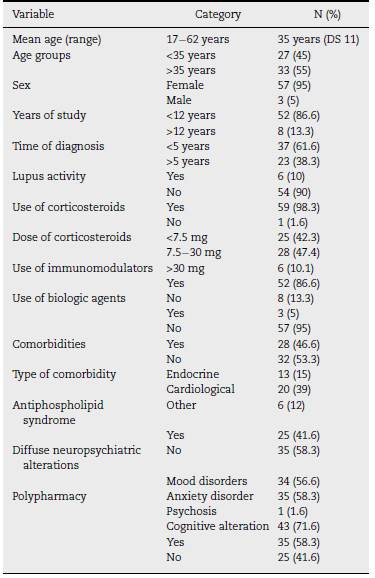
Sixty patients with diffuse neuropsychiatric disorders associ ated with SLE were included, the mean age was 35 years and the majority of them were women, with at least 12 years of study. At the time of the research, 37 patients had a time of diagnosis of the disease <5 years and 90% did not present lupus activity according to the Systemic Lupus Erythematosus Dis ease Activity Index 2000. As for the medication, 98.3% took corticosteroids, and almost half of them used intermediate doses (between 7.5-30 mg/day), while 52 patients (86.6%) used immunomodulators and 3 (5%) received biological agents. In addition, 46.6% had comorbidities, mainly cardiological, and 25 patients (41.6%) had an association with antiphospholipid syndrome. In total, 58.3% of the participants received polypharmacy. The 4 most prevalent diffuse neuropsychiatric syndromes were: cognitive impairment (71.6%), mood disor ders (56.6%), anxiety disorders (58.3%), and psychosis (1.6%). Table 1 describes the sociodemographic and clinical charac teristics of the study population.
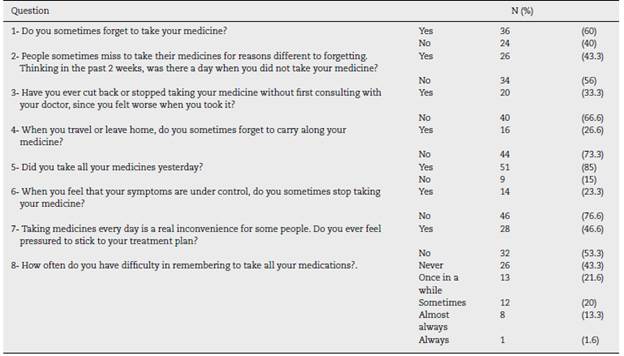
The MMAS-8 was used to assess adherence to treatment. Of the total population, 63.3% had low adherence (the global assessment is presented in Fig. 1). The breakdown of the answers obtained from the 8 questions that make up the MMAS-8 is found in Table 2.
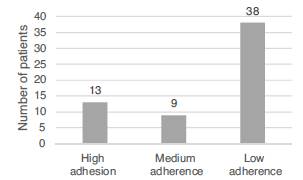
Fig. 1 Adherence to treatment in patients with diffuse neuropsychiatric disorders associated with SLE.
Discussion
In our work, according to the Morisky test applied, only 21.6% of the patients had high adherence to their pharmacolog ical treatment. Only patients with diffuse neuropsychiatric manifestations were analyzed; however, the result is consis tent with published data on adherence in patients with SLE. For example, the first work on adherence measured with a direct method, in which the hour when the drug bottles were opened was monitored with an electronic system, reported that throughout the 2 years of study only 24% of the participants adhered to their treatment in more than 80% of the doses that were initially prescribed. (13 In another more recent work, with 72 patients with SLE in an outpatient service of Internal Medicine in Spain, 63.9% did not have adequate adherence to treatment. (14 On a regional scale, a work con ducted in Peru determined an adherence of 25% in 48 patients with SLE. (15
There are studies that describe adherence problems in patients with psychiatric disorders.
A study conducted in China found that the presence of anxiety in patients with SLE, had a negative influence on the adherence; in contrast, Alsowaida et al. associated it with depression. (2,16
We described some variables of interest such as the years of study, time to diagnosis, lupus activity and polypharmacy; the latter was present in more than a half of the patients. In a study they found that the patients with high adherence had better punctuations in the sphere of mental health measured with questionnaires on quality of life, compared with those patients with lack of adherence to treatment. Furthermore, depression and polypharmacy were independent risk factors for poor adherence. (13
In 2003 the World Health Organization (WHO) made a report on the problems of adherence to treatment in chronic diseases. Already on that date, the WHO considered it a global problem of alarming magnitude, which would have as a con sequence an increase in direct and indirect healthcare costs and, logically, a negative impact on the health status of the individuals. (17
We consider that evaluating adherence to treatment should be one of the priorities in the consultation of a patient with SLE, especially in patients with neuropsychiatric manifestations. According to the WHO, it is emphasized that "increasing the effectiveness of interventions on therapeutic adherence can have a much greater impact on the health of the popula tion than any improvement in specific medical treatments-"17 Finally, the limitations of the study should be considered. This work was carried out with a relatively small sample; in addition, adherence to treatment and the presentation of neuropsychiatric disorders were measured with indirect methods subject to a margin of error, since they depended only on the veracity of the patient's report. On the other hand, the study was conducted in a public hospital, so there maybe differences regarding the characteristics of the population in private cen ters or with greater and better access to health services. It was also not possible to differentiate the primary neuropsychiatric disorders caused directly by the SLE, from those secondary to factors such as treatment, comorbidities, other metabolic alterations or psychosocial factors.
Conclusions
In our study population there is a significant number of patients (63.3%) with low adherence to treatment. The results highlight the importance of the diagnosis and treatment of neuropsychiatric disorders and their influence on adherence to treatment. The poor adherence to treatment in patients with SLE is a problem that must be taken into account in the management of this disease. New studies with larger samples and a more rigorous methodological design could identify risk factors for lack of adherence to management.











 texto em
texto em