Introduction
Spondyloarthritis (SpA) is a heterogeneous group of diseases that share a broad clinical and immunogenetic spectrum and that, due to the diversity of their manifestations consti tute a challenge for the diagnosis in early stages. This group of entities includes ankylosing spondylitis, reactive arthritis, psoriatic arthritis, spondyloarthritis associated with inflammatory bowel disease, juvenile-onset spondyloarthritis, and undifferentiated spondyloarthritis.1,2
The development and evolution of new classification crite ria have allowed their earlier identification, based on imaging (radiographic or magnetic resonance) or genetic (presence of HLA-B27) aspects coupled with a series of clinical and labo ratory manifestations. In addition, patients are classified into those with predominantly peripheral or axial involvement; the latter are subdivided into those forms with radiographic or non-radiographic evidence. (3
This new classification has allowed the introduction of the term «non-radiographic axial spondyloarthritis», which refers to patients with clinical, laboratory or genetic manifestations suggestive of spondyloarthritis in the absence of signs of axial involvement or sacroiliitis on the plain radiography, but evident on nuclear magnetic resonance images. This evi dence has given rise to a new taxonomy in SpAs in order to facilitate their understanding as follows: axial SpA with radio-graphic sacroiliitis, axial SpA without radiographic sacroiliitis (sacroiliitis in MRI or positive HLA-B27 with clinical mani festations); peripheral SpA with psoriasis, with inflammatory bowel disease (Crohn's disease, ulcerative colitis or undifferentiated colitis); SpA with preceding infection (reactive), without psoriasis, inflammatory bowel disease or preceding infection (undifferentiated SpA). In recent decades, it has been of great interest to improve early diagnosis and timely treat ment to stop the devastating effect that these diseases have in young people in full productive capacity. (4,5
There are immunogenetic, etiopathogenic, clinical, radio logical and treatment aspects that have aroused the interest of researchers worldwide. (6,7 However, the topics that have evolved the most in this group of diseases are genetic factors, inflammatory low back pain as a crucial cardinal sign in the classification criteria and diagnostic images, especially magnetic resonance imaging, essential for the early diagnosis and treatment of the SpAs. (8,9
Ankylosing spondylitis, the most common of all types of SpA, usually begins in the third decade of life, 5 years earlier in HLA-B27 positive patients than in those who are HLA-B27 negative. In the Spanish Regisponser registry, the average age of onset was 30 years. It occurs more frequently in men than in women, with a 2-3:1 ratio, while in patients with non-radiographic axial spondyloarthritis, the distribution by sex is equal. (10
SpAs have a high prevalence in Caucasian populations, far from the equatorial regions or from the tropics. The estimated prevalence of axial spondyloarthritis is about 0.32-1.4%, according to the population studied, while the prevalence for all types of spondyloarthritis, including the peripheral forms, varies between 0.2% in Southeast Asia and 1.6% in the North ern Arctic populations. In African-American and Japanese populations these are very rare diseases. Spain has a reported prevalence of 1.8% and in the United States is close to 1%.11-13
In Colombia there are still great questions regarding the behavior of this group of diseases, the largest cohort studies reported were conducted at the Central Military Hospital (Hos pital Militar Central) in Bogotá (139 and 218 patients) and at the Pablo Tobón Uribe Hospital (HPTU) in the city of Medellin (71 patients). (14,15
Londoño et al. (16 described the prevalence of different rheumatic diseases (osteoarthritis, fibromyalgia, rheumatoid arthritis, gout, lupus, Sjögren's syndrome, dermatomyositis, systemic sclerosis and SpAs), in addition to various musculoskeletal disorders (soft tissue rheumatism or appendicular regional pain, unspecified musculoskeletal discomfort and non-rheumatic diseases) in Colombia, based on the applica tion of a widely validated instrument: the Copcord model, and interviewed 6,693 individuals in the 6 most important capital cities of the country. The aforementioned researchers estab lished that the prevalence of ankylosing spondylitis in people over 18 years of age in cities such as Bogota was 0.08%, in Medellin 2.2% and in Cali 0.47%; more than 64% of the people interviewed were women.
Knowledge of the clinical and radiological behavior, as well as of the demographic characteristics and the burden of the disease in Colombian patients with spondyloarthritis, is important to promote timely diagnosis and treatment, in addition to planning comprehensive and correctly targeted strategies in the healthcare services. (17-19
Objective
To characterize the demographic aspects, the clinical and immunogenetic behavior of the acute phase reactants, the radiological behavior and the therapeutic requirements of the cohort of patients with SpA followed-up in the HPTU from January 1, 2005 to December 31, 2017.
Design
Descriptive cross-sectional study that follows-up a previously described cohort, which includes all patients with SpA who were diagnosed and followed-up for at least one year in the HPTU between January 2005 and December 2017.
Patients and methods
All patients over 18 years of age with spondyloarthritis who met the ASAS criteria (Ankylosing Spondilytis Assessment Study) and consulted the emergency rheumatology services, who were evaluated by a rheumatologist, from January 1, 2005 to December 31, 2017 were included. Those patients with other rheumatic diseases that could interfere with clinimetrics, such as rheumatoid arthritis, lupus, arthrosis of the spine and fibromyalgia, were excluded. Patients with autoimmune diseases, viral infections (HIV, hepatitis), and neoplasms were also excluded. The protocol was approved by the research and ethics committee of the HPTU.
The variables included in the analysis were: demographic (age, gender, age at onset of symptoms, personal and family history of SpA, psoriasis, uveitis, IBD); clinical (initial manifes tation of SpA: talalgia, uveitis, calcaneal enthesitis, dactylitis, cutaneous psoriasis, nail psoriasis, diarrhea, urethritis, arthri tis, Crohn's disease, ulcerative colitis, inflammatory low back pain, gluteal pain, morning stiffness, psoriasis, inflammatory bowel disease, and the type of spondyloarthritis); clinimetric (Basdai and Basfi score at baseline, maximum and average during the evolution of the disease and at the initiation of the tumor necrosis factor inhibitor [TNF-i]); laboratory (acute phase reactants [ESR and CRP], HLA-B27); imaging (MRI [spinal and sacroiliac joint bone marrow edema], presence of ero sions, syndesmophytes, fusion of the sacroiliac joints and plain radiographs thereof to apply the New York classification); and treatment (NSAIDs, oral steroids, COXIBS, methotrexate, sulfasalazine, TNF-i).
Methodology
Cohort study. The population was characterized by descrip tive statistics, the distribution of the continuous variables was determined with the Kolmogorov-Simirnoff method for those with n of 50 or more, and with the Shapiro-Wilk method for those with n less than 50. The parametric variables were summarized with means and standard deviations (SD) and the non-parametric variables with medians and interquartile ranges (IQR). The SPSS software, version 22, HPTU license, was used. The research was approved by the ethics committee of the institution and did not confer risk to the patients.
Results
The cohort consisted of 181 patients, 81 women (44.5%) and 100 men (54.9%), with a mean age of 45.3 years (SD = 13.39 years) and a range between 20 and 83 years. 24.2% (44) of the subjects were 35 years old or younger, 40.6% (74) between 36 and 50 years old and 35.2% (64) were older than 50 years.
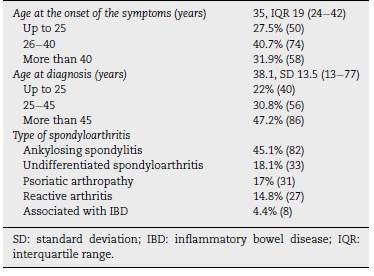
The average age at admission to the cohort was 39.31 (SD = 12.32 years), with a range between 17 and 77 years. 24.7% (45) were 30 years old or younger, 54.4% (99) between 30 and 50 years old and 20.9% (38) were older than 50 years. The median follow-up time of the patients was 5 years (IQR = 32.0-32). 46.2% (84) were followed-up for more than 6 years, 30.8% (56) between 3 and 6 years and 23.1% (42) for less than 3 years. The duration to establish the diagnosis since the onset of the symptoms was around 5 ± 7 years, similar to what happened in the different cohorts worldwide (6 years). The demographic characteristics of the population are described in Table 1.
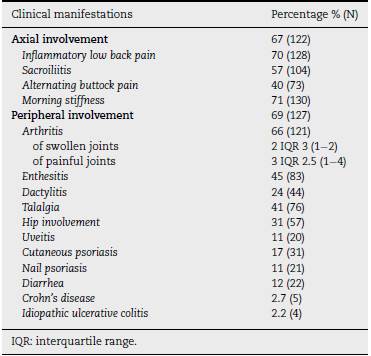
7.7% (14) of the patients with ankylosing spondylitis had a family history of SpA, which was observed in 3.8% (7) of those with psoriatic arthropathy, 1.1% (2) with reactive arthritis and in 0.5% (1) of those diagnosed with IBD or undifferentiated spondyloarthritis; 84% of the subjects (153) did not have a family history of spondyloarthritis. Table 2 shows the clinical characteristics of the population.
The median maximum value of the erythrocyte sedimen tation rate (ESR) was 21 mm/h, IQR 40 (2-75). 43.4% (79) of the patients had a normal ESR (up to 20 mm/h), 26.4% (48) between 21 and 49, and 30.2% (55) of 50 (74) mm/h, or higher. CRP was found to be elevated in 40.7% (74) of the cases (normal value1 mg/dL) and the median maximum value during the evolution was 1.7 mg/dL, IQR 5 (0.5-24).
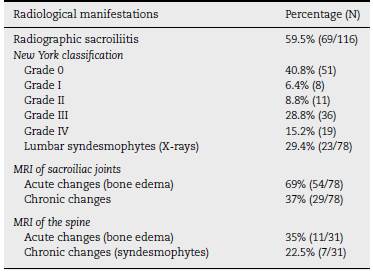
8.8% (16) of the patients had a CRP of 5 mg/dL or lower, 4.9% (9) between 5.1 and 10 mg/dL and 86.3% (157) higher than 10 mg/dL. HLA-B27 was positive in 55.6% (59/106) of the patients. Table 3 describes the radiological manifestations of the studied population, while Table 4 shows the clinical char acteristics in the different types of SpAs.
The population was characterized by having high activity both upon entry to the cohort and during the follow-up. The initial Basdai score was of 4 IQR 3 (0-8) and 89% of the patients had a score of 4 or more. During follow-up the average Basdai score was 3.3 SD 1.9 (0-8).
91.1% of the patients (164/181) were treated with NSAIDs, 60.1% (107/178) with sulfasalazine, 43.4% (76/175) with selec tive cyclo-oxygenase-2 inhibitors NSAIDs, 33.7% (59/175) with methotrexate and 20-45% (36/176) with steroids. The use of TNF-i was required in 56% of the cases (101/181). The most undifferentiated widely used biological drug was adalimumab, in 31.1% of the cases (56), followed by etanercept, in 21.7% (39), and infliximab, in 13.9% (25). 30.8% (31) of the patients required more than one TNF-i.
Discussion
SpAs are characterized by a broad clinical and immunogenetic spectrum that varies according to the study population. The present cohort includes 181 patients from Northwestern Colombia. A description of 2 cohorts had been made previ ously in Colombia, one at the Bogota Military Hospital, with 139 patients, and the other of the HPTU, with 71 patients. (14,15
There was a predominance of men in the population, and in 124 patients the onset of symptoms was before the age of 40, a finding consistent with what is described in the literature, affecting mainly young people in the productive stage. The mean age at diagnosis was 45.3, SD = 13.39 years, higher than the age of onset of the symptoms, which represents an average delay in the diagnosis of 6 years, as has been described in the different cohorts studied worldwide. (20-22 Possibly, the delay in the diagnosis is associated with multiple factors such as the sensitivity of primary care physicians in detecting patients with inflammatory low back pain, socioeconomic conditions, and access to health systems in each population23,24. Various aspects can explain the delay or the difficulty in making a timely diagnosis: in our environment, the lack of knowledge of the disease, even by health personnel or non-rheumatologist physicians, the shortage of rheumatologists nationwide, the difficulties for patients to obtain a timely specialized con sultation in rheumatology through their health provider, the difficulty in accessing imaging studies such as magnetic res onance imaging or immunogenetic such as HLA-B27, due to the cost or lack of availability. Even, more than 60% of our consultation in the HPTU corresponds to patients that attend private consultation, seeking a second option in the face of the diagnostic and therapeutic uncertainty. If the migration of the patients by the different health provider institutions is added to all the above, due to the hiring up and downs, the follow-up of this group of diseases in Colombia becomes more difficult.
Ankylosing spondylitis was the most frequent, followed by undifferentiated spondyloarthritis and psoriatic spondyloarthritis. Inflammatory low back pain, morning stiffness, enthesitis and dactylitis were the most frequent clinical man ifestations, just as we had described it in 2010. (15
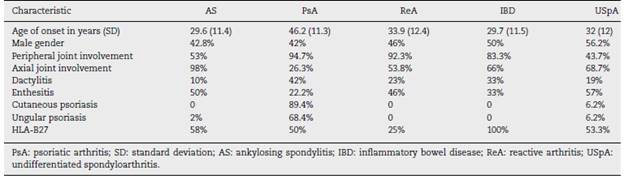
In the analysis by groups, ankylosing spondylitis begins earlier, between the second and third decades of life, unlike psoriatic arthritis that classically begins after 40 years of age. Dactylitis was more frequent in the group with psoriatic arthritis, while enthesitis was more prevalent in those with undifferentiated spondyloarthritis and ankylosing spondylitis (see Table 4).
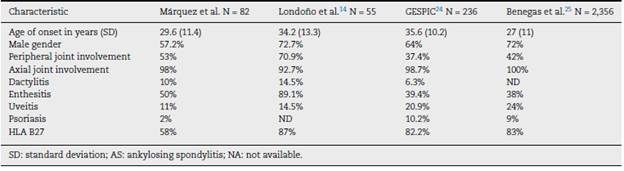
In the group of patients with ankylosing spondylitis, peripheral involvement was frequent, arthritis was present in 53%, followed by enthesitis (50%) and dactylitis (10%), similar to the other Colombian series by Londoño et al. (14 This situation differs from the European cohorts such as Gespic24 and the binational Regisponser/Aspect et al., (25 in which the peripheral manifestations were fewer. In this group, the difference in frequency between men and women was 1.3/1, in contrast to the Londoño et al. (14, Gespic26 and Regisponser/Aspect25 cohorts which showed a higher fre quency of presentation in men, with a man/woman ratio between 1.8 and 2.7/1.
The most frequent extra-articular manifestation in patients with ankylosing spondylitis was uveitis, which occurred in 11% of the population, a lower percentage com pared with the Gespic cohort which was 20.9%.23 A possible explanation for this difference is the relationship between uveitis and HLA-B27 and its higher prevalence in the European population.
In general, the behavior of SpA differs between European and Latin American countries; in the latter, peripheral involve ment predominates and patients present more enthesitis; NSAIDs, steroids and disease-modifying drugs are more fre quently used, while the patients in Europe have a higher frequency of positive HLA-B27, which may also explain the greatest axial involvement. (25,26
The differences between the group of patients with anky-losing spondylitis included in this series, together with the other Latin American cohort of Londoño et al. (14 and the Euro pean Gespic26 and Regisponser/Aspect25 are summarized in Table 5.
In the population, peripheral arthritis was present in 53% of the patients, greater than that was described in the Ger man Gespic and the Spanish Regisponser cohorts, in which it ws observed approximately in 37-42% of the subjects studied.
Like in the other studies in which Colombian patients are described, HLA-B27 is present in 50-60% of the cases, which differs from the European cohorts in which the prevalence is higher than 80%.18
Regarding acute phase reactants, CRP and ESR were ele vated in approximately 40% of the cases, and 60% of the patients had radiographic sacroiliitis. This finding is impor tant given that the elevation of the CRP has been associated with structural damage and radiographic progression. (14
The population was characterized by having high activity, both upon the entry to the cohort and during the follow-up, similar to that was described in the patients of Regisponser, who had high Basdai and Basfi indices, (10 which can explain that 56% of the cases of our population requires the use of TNF-i.
The weaknesses of the study are those inherent to descrip tive observational studies, such as the information bias determined by aspects such as incomplete information and irregular follow-up, while the main strength is the inclusion of all subjects with ASp, which allows us to generalize the findings to the population of origin.
Conclusions
A slight predominance of men was observed in the cohort, ankylosing spondylitis was the most frequent disease, axial and peripheral manifestations had a similar frequency, although inflammatory back pain and morning stiffness were the most frequent. The population was characterized by high activity and functional compromise, demonstrated by the high Basdai and Basfi scores and because 56% of the patients required TNF-i agents.











 texto em
texto em