Introduction
Chronic recurrent multifocal osteomyelitis (CRMO), also known as chronic non-bacterial osteomyelitis, is an autoinflammatory disease characterized by bone involvement, with flare-ups and absence of microbiological isolation.1-3) It is a rare entity, probably underdiagnosed in pediatrics. (1
It usually occurs as pain and functional impotence and, despite how disabling it can be, in the majority of cases it tends to spontaneous resolution. In 80% of cases, it courses with multifocal and symmetrical pain that fundamentally affects the metaphysis of long bones, clavicles, pelvic bones or vertebrae. 20% present recurrent monofocal pain, being more complicated in these cases to establish the diagnosis, since it is necessary to make the differential diagnosis with a wider range of pathologies such as bacterial osteomyelitis, trauma, or malignant processes. (1,2,4-6 It is a diagnosis of exclusion and it is established through the combination of clinical, radio-logical and histological findings; although the latter are not essential. However, in cases of monofocal involvement, they may be necessary. (1,2,7
The bases of treatment are NSAIDs, although in a high percentage they are insufficient for an adequate symptom control, so in some cases corticosteroids may be required. Bisphosphonates or drugs against the tumor necrosis factor, which not only allow to control the clinical symptoms, but also the remission of the disease, are used more and more frequently. (1,2,4,8
The objective of the study is to describe our experience with three girls diagnosed with CRMO in the last five years, highlighting the clinical presentation, the findings in the complementary tests, the treatment and the evolution of the disease in these patients.
Patients and methods
It was conducted a retrospective review of medical records of children diagnosed with CRMO in the last five years, fol-lowed up in pediatric rheumatology consultation in a tertiary hospital that cares for children up to 14 years of age.
For this purpose, the following variables were analyzed: gender, age, symptoms presented (in case of pain: location: foci presented and time of evolution), results of analytical studies, imaging tests and histological findings, as well as the treatment received and the evolution of the disease.
The inclusion criteria used were: diagnosis of CRMO and onset of the symptoms under 14 years of age.
Results
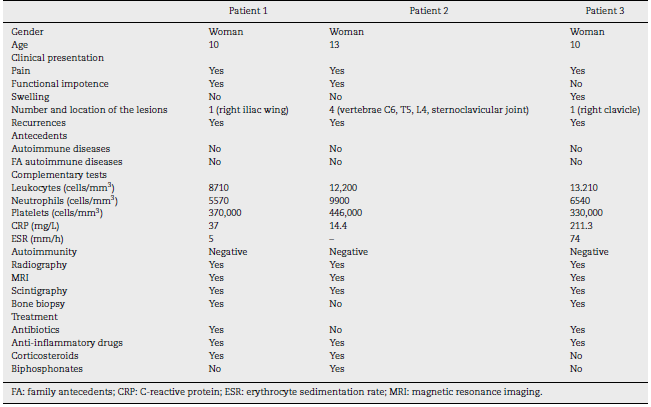
We describe three cases of adolescent girls who consulted for bone pain and with a definitive diagnosis of CRMO. In Table 1 we can see the summary of the data.
Table 1 Clinical and analytical data, imaging tests and treatment given in three patients diagnosed with CRMO.
Case 1
A 10-year-old girl followed-up by traumatology due to limp flare ups since she was seven years old. She consulted again for an episode of pain and functional impotence, referred at the level of the right hip, which worsened with rest. The patient reported an infectious process in the previous week. The physical examination shows pain in the right iliac wing, with flexion of the right hip painful in the last degrees, so it was decided to take a radiograph that showed a well-defined osteolytic lesion, with a sclerotic border around it, at the level of the right iliac wing. Hospital admission was decided to complete the study with a diagnosis of suspected osteomyelitis and intravenous antibiotic therapy was prescribed.
The blood count resulted anodyne (hemoglobin 13.3 g/dL, platelets 370,000 cells/mm3, leukocytes 8710 cells/mm3, neutrophils 5570 cells/mm3, lymphocytes 2080 cells/mm3). Acute phase reactants discretely elevated, with C-reactive protein (CRP) 37 mg/L (normal value <5mg/L) and erythrocyte sedi-mentation rate (ESR) 5mm/1sth (normal value <5mm/1sth). The study was completed with blood cultures that resulted negative, as well as negative Mantoux test and serologies for EBV, CMV, HSV, parvovirus and brucella.
A magnetic resonance imaging (MRI) scan was performed, showing signs of chronic osteomyelitis, with bone widening and findings suggestive of bone sequestration in the right iliac wing. A bone biopsy was obtained, with predominance of polymorphonuclear cells, multinucleated giant cells and histiocytic aggregates compatible with chronic osteomyelitis. The culture of the lesion for bacteria, mycobacteria and fungi resulted negative. After establishing the diagnosis and achieving an adequate pain control, the patient was discharged.
In outpatient basis, it was performed a scintigraphy that only showed hyperuptake at the level of the iliac spine, with-out revealing lesions in other locations. The autoimmunity study was negative for ANA, ANCA, anti-DNA, ENAs and HLA-B27. Home treatment with ibuprofen at a dose of 10 mg/kg/8 h was started, without improvement, so it was replaced with prednisone 1 mg/kg/day for 15 days, with a descending pattern, but with a relapse when the decrease started.
She is currently maintained with adequate pain control at home, with oral naproxen, and clinical and radiological stability.
Case 2
A 13-year-old girl who consulted for low back pain of four months of evolution associated with weakness and progressive functional impotence. The patient reported intense pain radiating to the lower right limb from the beginning of the day, which woke her up at night and partially subsided with ibuprofen. On physical exam highlighted a significant decrease in strength, with inability to lift the lower limbs against resis-tance and painful gait. Dorsal paraspinal pain was associated with flexion and extension of the spine. A lumbar X-ray was performed showing an osteolytic lesion with well-defined borders in lumbar vertebra L4, and the study was completed with a MRI of the spine: bone marrow edema in the vertebral body of L4 with moderate uptake of gadolinium, preserved morphology of the vertebral body, without evidence of involvement of posterior elements or soft tissue masses.
One month later, she presented a new episode of low back pain, associated with a feeling of weakness of upper limbs and continuing with functional impotence in the lower limbs. The MRI scan of the spine was repeated and a signal alteration was observed in the body and the upper and anteroinferior plates of L4. Signal alteration of C6, T5 vertebrae and incidental involvement of the right sternoclavicular joint also appeared. All these alterations suggest the possibility of CRMO.
Given the flowery nature of the picture, it was decided to admit the patient to the hospital and complete the study with laboratory analyses (hemoglobin 14 g/dL, platelets 446,000 cells/mm3, leukocytes 12,200 cells/mm3, neutrophils 9900 cells/mm3, lymphocytes 1500 cells/mm3), acute phase reactants (CRP 14,4 mg/dL), serology (negative for toxoplasma, rubella, CMV, EBV, HSV, parvovirus, Coxiella burnetii, leishmania, rickettsia, HAV, HBV and HCV) and immunity study that resulted negative for ANA, ANCA, anti-DNA, ENAs and HLA-B27. A scintigraphy was also performed that shows diffuse uptake in the same locations described in the MRI.
Treatment with ibuprofen was started during hospitalization without achieving pain control, so it was necessary to associate intravenous dexketoprofen with partial improvement, and finally, complete response to oral naproxen. The patient was discharged four days after admission.
At home, she presented new episodes of pain and func-tional impotence, mainly at the lumbar level, without a complete response to NSAIDs and corticosteroids, so it was decided to associate treatment with bisphosphonates (pamidronate at a dose of 1 mg/kg, monthly dose for nine months), with a good evolution: resolution of the clinical symptoms in three months, without the appearance of new osteolytic lesions in the control scintigraphy performed six months after the start of treatment and with radiological sta-bility of the lesions described.
Case 3
A 10-year-old girl from Romania, who consulted for right omalgia (shoulder pain) of two weeks of evolution, without overstrain or previous trauma. It did not interfere with night rest and presented partial improvement with the administration of anti-inflammatory drugs (ibuprofen). She did not refer pain at other levels. In the week prior to admission, she presented catarrhal symptoms and fever of up 38 ° C, being a self-limited clinical picture that subsided in 48 h.
On the examination, swelling in the proximal end of the right clavicle stood out, with heat, erythema and edema in the area. The patient presented selective pain on palpation in the proximal third of the right clavicle, without limitation of movement. She did not report pain on palpation of the rest of the joints or in the contralateral limb. In the Emergency Service and due to suspicion of an acute infectious process, laboratory tests were performed, whose results showed mild leukocytosis as the only significant finding (hemoglobin 14.6 g/dL, platelets 330,000 cells/mm3, leukocytes 13,210 cells/mm3, neutrophils 6540 cells/mm3, lymphocytes 4150 cells/mm3) and important elevation of acute phase reactants: C-reactive protein 211.3 mg/L (normal value <5 mg/L) and globular sedimentation rate 74mm/1sth (normal value <5 mm/1sth).
Due to the suspicion of infectious osteomyelitis, an X-ray of the clavicle was performed, which showed no pathological findings, and a computed tomography (CAT) scan revealed a hypodense lesion at the proximal end of the right clavicle, with intense periosteal reaction at that level. After the evaluation by traumatology, it was decided surgical debridement of the lesion (the samples were sent to microbiology and pathological anatomy) and admission to the hospital ward for intravenous antibiotic therapy, follow-up and completion of the study.
The serology tests resulted negative for CMV, EBV, HSV, toxoplasma, rubella, parvovirus, C. burnetii, rickettsia and hep-atotropic viruses (HAV, HBV and HCV). The study of immunity was normal (negative ANA, ANCA, anti-DNA, ENAS), the blood cultures and the culture of the surgical sample of the lesion were negative and the anatomopathological analysis of the biopsy of the bone tissue was anodyne, with nonspecific findings, although not compatible with acute osteomyelitis.
Given the adequate clinical evolution and the normalization of the acute phase reactants, antibiotic therapy was discontinued after two weeks of treatment. A bone scintigraphy was performed prior to discharge, which showed increased uptake in the right clavicle exclusively, with no lesions at other levels. After two weeks of hospitalization and adequate pain control with intravenous dexketoprofen, the patient was discharged and is asymptomatic.
In the review, three months after the acute process, the patient referred two new episodes of right omalgia, related with physical exercise, which coincided with inflammation in the clavicular region that was self-limited after three or four days and subsided with ibuprofen at doses of 10mg/kg/8h. The patient was asymptomatic between the episodes of joint inflammation. A MRI scan was performed on an outpatient basis due to an antecedent of osteomyelitis, and persistence of bone hypertrophy with altered signal intensity was observed in the proximal third of the right clavicle. After the administration of the contrast media, moderate uptake was observed in the proximal third of the right clavicle and in the adjacent soft tissues, as well as slight uptake in the upper and right aspects of the sternum. All this suggests a chronic bone inflammatory process located in the proximal third of the right clavicle, suggestive of chronic osteomyelitis.
Currently, the patient is asymptomatic, without continuous treatment, and requires ibuprofen or naproxen at anti-inflammatory doses in specific processes of pain and bone inflammation. In imaging tests requested on an outpatient basis, radiological stability was observed, with improvement of inflammatory signs in the right clavicular lesion
Discussion
CRMO is a rare auto-inflammatory disease, with unknown incidence and prevalence that fundamentally affects children and young adults, with infrequent appearance in people over 20 years of age. It presents a clear predominance in the female gender, as occurs in the cases presented here, in which the three patients were school-aged women or adolescents, although it was not very significant due to the small number of patients. (1,2,4,5
In up to 25% of cases, this condition may be associated with other auto-inflammatory or autoimmune diseases such as psoriasis, arthritis, sacroiliitis or inflammatory bowel disease, and in up to 40% of cases there are first or second degree relatives affected by auto-inflammatory or autoimmune diseases, suggesting a common pathophysiology and the influence of genetic factors. (1-2-9,10 In our series, there were no relatives affected by auto-inflammatory or autoimmune diseases, although this could be due to the small sample size, as mentioned above.
Regarding the clinical presentation, the most frequent symptom is bone pain, usually with inflammatory characteristics, and which sometimes makes it difficult the nocturnal rest. In general, it is a pain of moderate intensity that does not usually show a complete response to treatment with anti-inflammatory drugs. It can also be associated with other symptoms such as functional impotence (it appears in up to 60%-80% of cases depending on the series) and other less frequent symptoms such as fever or systemic symptoms (asthenia or anorexia). (1,2,10
In most cases, the patient has several simultaneous points of musculoskeletal pain that is usually symmetric, although it is not uncommon for it to manifest as a single focus of pain that changes location throughout the course of the disease. (1,2,4,5 Its typical location is the metaphyses of longbones, being more frequently affected those of the lower limbs (femur and tibia), followed by clavicle, ribs, vertebrae and pelvic bones. (1,2,4
In the cases presented, only one of the patients presented multifocal involvement, while the other two had recurrent episodes of pain in the same location (clavicle or iliac wing). Regarding the location, none of the patients had involvement of metaphysis of the long bones. The location was: pelvic bones, vertebral involvement at several levels and clavicle, being all of them bones typically affected by this disease.
Although several diagnostic criteria have been described (Jansson, Handrick and Bristol or Roderick criteria), none of them is widely applied. The diagnosis is made by the combination of clinical, radiological and sometimes pathological findings. (1 It is a diagnosis of exclusion, especially difficult in cases of a single bone involvement, in which it is important to make the differential diagnosis with bone tumors (Ewing's sarcoma, eosinophilic granuloma or aneurysmal bone cyst) or infectious processes such as acute osteomyelitis. In these cases, it is especially indicated a bone biopsy, which, even when its findings are not specific, allows to rule out other important entities such as tumor pathology or infectious osteomyelitis. (1,2,4
Regarding imaging tests, there is no clearly established protocol on the best test to perform. Radiography is not usually helpful in the early stages of the disease, since significant demineralization is necessary to visualize the typical lytic lesions. (2,5 CT can be used to determine single lesions, although it is not an adequate imaging test due to the scant information it provides in the case of bone pathology and the irradiation that it entails. (4 MRI is the technique of choice for the differential diagnosis of bone lesions, especially useful in early stages of the disease as it allows to visualize findings that go unnoticed by radiography or CT.
The use of whole-body MRI is useful in the diagnosis of this disease as it helps to detect asymptomatic lesions. It is useful in the long-term follow-up of these patients, given that it allows to evaluate the response to treatment. (1,2,11,12 In turn, scintigraphy, another test widely used, is used in the same way than the whole-body MRI to complete the extension study and reveal asymptomatic lesions. (1,2,12 For all these reasons, the presence of multifocal pain in the absence of trauma, with a course in flare ups and with compatible findings in imaging tests, it is sufficient to establish the diagnosis of CRMO.
In the case of a monofocal lesion, it is imperative to rule out malignancy and, in addition of the clinical and radiological findings, it is necessary to perform a bone biopsy. (1,2 In all cases presented, a bone X-ray was performed due to pain at a single level, and in one of them, in which acute osteomyelitis was suspected, a CAT scan, possibly for its greater accessibility from the Emergency Service. In all cases, the study was completed with scintigraphy and MRI as an extension study. A biopsy was performed in patients with a single lesion, with results compatible with osteomyelitis.
Laboratory abnormalities are usually nonspecific and very variable depending on the patient, ranging from normal values to findings suggestive of systemic inflammation such as anemia, leukocytosis, or thrombocytosis. Another frequent finding is the elevation of acute phase reactants, which appear elevated in up to 70%-90% of cases. (1,5 In our series, all of them had normal hemoglobin levels and platelet counts. Two of them had mild leukocytosis and all had a slight increase in acute phase reactants, except in the third case, which presented a significant increase in CRP and ESR. In addition, and given the association of chronic recurrent multifocal osteomyelitis with other autoimmune pathologies, an immunity study was carried out in all cases, being negative in all of them. (1,2,9
Regarding treatment, NSAIDs are the drugs of choice because they are useful for symptomatic control. However, they have no effect on the radiological image and they do not allow to control the disease activity. (1 In cases refractory to treatment with anti-inflammatory drugs, persistence of pain despite the therapy, or frequent relapses when attempting to withdraw the drug, treatment with corticosteroids at doses of 1-2 mg/kg/day for a period of four to eight weeks can be associated, with slow and progressive reduction of the dose. (1,2,4,5
Bisphosphonates are indicated in case of no response to NSAIDs or corticosteroids, as well as in partial response to treatment with corticosteroids or recurrence when their dose is reduced. Unlike the former, they not only allow rapid pain relief due to their anti-osteoclastic action, but also to achieve remission of the disease and the normalization of the radiological findings. (1,2,13,14 Within the group of bisphosphonates, intravenous pamidronate is the most widely used in children due to the greater experience with this drug in pediatrics. (13-16
In cases refractory to pamidronate, we can resort to biological therapy, among which anti-TNFs (adalimumab, infliximab or etanercept) are indicated, which, like biphosphonates, contribute to a symptomatic and radiological improvement that can be maintained up to two years after the treatment is completed. (1,2,17,18 Methotrexate is an effective and relatively frequently used drug in this pathology.
Other drugs, although less widely used, are calcitonin, interferon or even, in some series, the usefulness of azithromycin has been described due to its anti-inflammatory and immunomodulatory effect. (4,5 In our series, one girl responded to treatment with NSAIDs; in another it was necessary to associate corticosteroids at a dose of 1 mg/kg/day and the other one, in addition to NSAIDs and corticosteroids, needed intravenous pamidronate, and presented an adequate pain control. In addition, two of the cases received initially intravenous antibiotic therapy, possibly because it was a unifocal involvement and on the suspicion of acute infectious osteomyelitis. However, the lack of effectiveness of antibiotics in the CRMO has been demonstrated.2)
Despite how disabling it can result and its course in flare ups, it is a disease with a good long-term prognosis that usually resolves between two and 10 years after its onset, with-out leaving sequelae or presenting new subsequent flare ups. However, on rare occasions, complications such as early physeal closure and secondary short stature, bone deformities and kyphoscoliosis as a result of vertebral involvement, degen-erative osteoarthritis or pathological fractures may occur, among others. (1,2 Recurrences have been related to a longer time of evolution of the disease until its diagnosis and with the presence of another concomitant autoimmune or anti-inflammatory disease. (2,19











 text in
text in 


