Introduction
Inflammatory myopathies are considered rare diseases, how-ever, among them, dermatomyositis is the most common, except in elderly patients, in whom inclusion body myositis predominates.1 Dermatomyositis is the only inflammatory myopathy that is characterized by presenting skin lesions, and since dermatological manifestations may be the first findings of the disease, they must be clearly and timely recognized. (2 In the US, the estimated prevalence is 1-6 patients per 100,000 inhabitants.3 In Colombia, the incidence and prevalence are not known.
Dermatomyositis is considered a heterogeneous disease, not only due to its clinical presentation, but also because of its course and prognosis.4 In addition to the muscle and skin, it can involve different organs and systems, such as the heart, the gastrointestinal tract and the lungs, which makes it a diagnostic challenge.5 It can be associated with malignancy, and can occur concomitantly with other connective tissue diseases.4
Despite being classified within the rare diseases, it has a significant morbidity and mortality, which can be explained by its chronic and progressive course, with irreversible muscle damage. Until now, there are scarce data that allow to characterize the patients who suffer from dermatomyositis in Colombia, and in view of the importance of timely diagnosis and management, this work seeks to describe the main demographic characteristics, the dermatological and systemic manifestations, the immunological profile and the concomitance with malignancy and other connective tissue diseases, in a university hospital in Bogotá, Colombia.
Methods
It is a descriptive cross-sectional study that was conducted in a university hospital in Bogotá, Colombia. The study included patients with a diagnosis of dermatomyositis who met the Bohan and Peter classification criteria, during the period between January 2004 and December 2019.
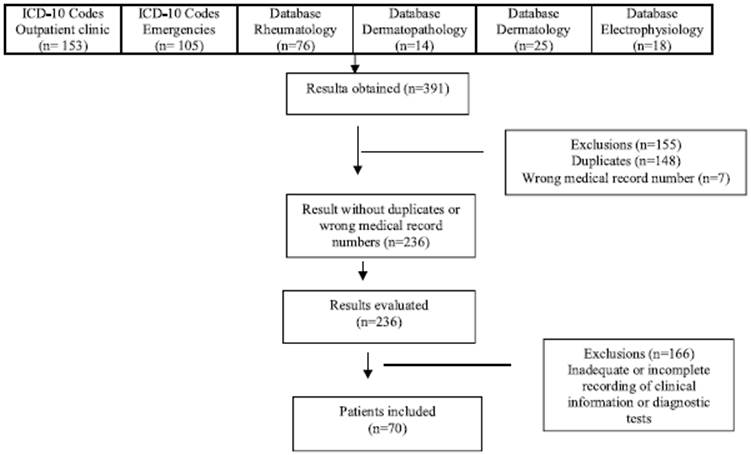
The data were obtained from different information sources, including the electronic medical record system of the hospital, in which the ICD10 diagnostic codes associated with dermatomyositis ((M33: Dermatopolymyositis, M330: Juvenile dermatomyositis, M331: Other dermatomyositis, M332: Polymyositis and M339: Dermatopolymyositis, unspecified) were searched. In addition, the databases of the units of dermatology, rheumatology, dermatopathology, and electro-physiology of our hospital were used.
Clinical and paraclinical variables were evaluated, using summary measures in frequencies and percentages for the qualitative variables, as well as central tendency measures with means and dispersion for the quantitative variables, using in this case Microsoft Excel®.
The study was approved by the Ethics and Research Committee of the Faculty of Medicine of the Pontificia Universidad Javeriana, with approval number 2019/207. The ethics commit-tee considered that since it was a retrospective study, without specific intervention or risks for the patients, it did not require the signing of an informed consent.
Results
General demographic aspects
A total of 236 results were obtained, of which 63 patients met the Bohan and Peter classification criteria, and seven had a diagnosis of amyopathic dermatomyositis. Duplicate and erroneous numbers of clinical histories were excluded, as well as patients with an intra-institutional diagnosis of dermatomyositis, but with inadequate or incomplete registration of the information related to the variables of interest, in addition to patients with an extra-institutional diagnosis who did not have a report of diagnostic tests in the clinical history that would allow to confirm the diagnosis (Fig. 1).
The average age of diagnosis was 43 years (SD±15.3), 48 were women (68.5%), with a female: male ratio of 2.1:1. Of the total number of patients, 63 (90%) had dermatomyositis and 7 had amyopathic dermatomyositis (10%). Likewise, 59 (84.2%) patients required at least one hospitalization; on average, 1.9 hospitalizations (±2.4), with a hospital stay of 8.6 days (± 10.1) (Table 1).
Tabla 1 Características demográficas
| Clásica | Amiopática | Total | |
|---|---|---|---|
| Número de pacientes, n (%) | 63 (90) | 7 (10) | 70 |
| Edad de diagnóstico, an˜ os (DE) | 43 (± 15,3) | 47 (± 7,4) | 43 (± 15,3) |
| Dermatomiositis en adultos, n (%) | 60 (85,7) | 7 (10) | 67 (95,7) |
| Dermatomiositis juvenil, n (%) | 3 (4,2) | 3 (4,2) | |
| Género | |||
| Femenino, n (%) | 43 (61,4) | 7,1 | 48 (68,5) |
| Masculino, n (%) | 20 (28,5) | 2,8 | 22 (31,4) |
| Hospitalizaciones, n (%) | 2,0 (± 2,5) | 0,8 (± 0,3) | 1,9 (± 2,4), |
| Estancia hospitalaria, días (DE) | 8,6 (± 10,3) | 8,4 (± 8,9) | 8,6 (± 10,1) |
| Mortalidad, n (%) | 5 (7,14) | - | 5 (7,14) |
| DE: desviación estándar. | |||
Clinical characteristics
Regarding the dermatological findings found in the patients with classic dermatomyositis, 63 (100%) patients presented pathognomonic manifestations,1,6 among which Gottron papules and heliotrope erythema were the most frequent, both findings being documented in 49 (77.7%) patients.
Forty (63.4%) patients presented characteristic manifestations. The V sign, which was the most frequent, was found in 30 (47.6%) of them. Compatible manifestations were documented in 51 (80.9%) patients, while 7 cases (11.1%) corresponded to infrequent manifestations, 10 (15.8%) to rare ones and 23 (36.5%) to nonspecific (Table 2).
Table 2 Dermatological manifestations.
| Clásica | Amiopática | |
|---|---|---|
| Manifestaciones dermatológicas patognomónicas, n (%) | ||
| Pápulas de Gottron | 49 (77,7) | 7 (100) |
| Signo de Gottron | 25 (39,6) | 4 (57,1) |
| Eritema en heliotropo | 49 (77,7) | 6 (85,7) |
| Manifestaciones dermatológicas características, n (%) | ||
| Telangiectasias periungueales | 17 (26,9) | 3 (42,8) |
| Hipertrofia periungular | 16 (25,3) | 2 (28,5) |
| Infartos hemorrágicos en los pliegues | 1 (1,5) | 1 (14,2) |
| Signo del chal | 19 (30,1) | 2 (28,5) |
| Signo de la V | 30 (47,6) | 3 (42,8) |
| Placas atróficas, descamativas y eritematosas en el cuero cabelludo | 3 (4,7) | - |
| Signo de la funda de pistola | 11 (17,4) | 1 (14,2) |
| Manifestaciones dermatológicas compatibles, n (%) | ||
| Poiquilodermia | 47 (74,6) | 6 (85,7) |
| Edema periorbital y facial | 19 (30,15) | 1 (14,2) |
| Manifestaciones dermatológicas infrecuentes, n (%) | ||
| Vésico-ampollas epidérmicas | 1 (1,5) | - |
| Lesiones necróticas o erosiones superficiales | 3 (4,7) | - |
| Vasculitis cutánea | 3 (4,7) | - |
| Calcinosis cutis | 3 (4,7) | 1 (14,2) |
| Manifestaciones dermatológicas raras, n (%) | ||
| Paniculitis | - | - |
| Mucinosis | - | - |
| Eritrodermia | 1 (1,5) | - |
| Cambios en la mucosa oral | 1 (1,5) | - |
| Eritema flagelado | - | - |
| Manos de mecánico | 6 (9,5) | 1 (14,2) |
| Hiperqueratosis folicular | 2 (3,1) | 1 (14,2) |
| Manifestaciones dermatológicas inespecíficas, n (%) | ||
| Fenómeno de Raynaud | 10 (15,8) | 1 (14,2) |
| Prurito | 3 (4,7) | - |
| Fotosensibilidad | 14 (22,2) | 2 (28,5) |
| Fuente: clasificación de acuerdo con las revisiones narrativas realizadas por DeWane et al.1 y Mainetti et al.6. | ||
Among the systemic manifestations, 19 (30.15%) patients presented gastrointestinal manifestations, 12 (19.0%) pulmonary manifestations and 3 (4.7%) had cardiac manifestations. Of the 63 patients with classic dermatomyositis, 11 (17.4%) reported constitutional symptoms, 12 (19.0%) concomitantly presented other connective tissue diseases and 6 (9.5%) presented cancer, of which 3 were breast cancer, 2 lung cancer and one colorectal (Table 3).
Table 3 Systemic manifestations.
| Clásica | Amiopática | |
|---|---|---|
| Manifestaciones pulmonares, n (%) | ||
| Enfermedad pulmonar intersticial | 8 (12,6) | - |
| Neumonía por aspiración | 2 (3,1) | - |
| Hipertensión pulmonar | 6 (9,5) | - |
| Hipoventilación alveolar | 1 (1,5) | - |
| Neumotórax | - | - |
| Neumomediastino | - | - |
| Manifestaciones gastrointestinales, n (%) | ||
| Disfagia | 15 (23,8) | - |
| Reflujo gastroesofágico | 4 (6,34) | - |
| Retraso en el vaciamiento gástrico | - | - |
| Disminución de la motilidad intestinal | 3 (4,7) | - |
| Incontinencia rectal | - | - |
| Manifestaciones cardiacas, n (%) | ||
| Miocarditis | 1 (1,5) | - |
| Falla cardiaca | - | - |
| Defectos en la conducción | - | - |
| Pericarditis | - | - |
| Enfermedades valvulares | 2 (3,1) | - |
| Otras manifestaciones sistémicas, n (%) | ||
| Vasculitis retiniana | - | - |
| Lesión renal aguda | - | - |
| Compromiso del sistema nervioso central secundario a vasculitis | - | - |
| Síntomas constitucionales, n (%) | ||
| Fiebre | 3 (4,7) | - |
| Pérdida de peso | 11 (14,2) | 3 (42,8) |
| Asociación con malignidad, n (%) | 6 (9,5) | - |
| Asociación con enfermedades del tejido conectivo, n (%) | ||
| Lupus eritematoso sistémico | 5 (7,9) | - |
| Esclerodermia | 6 (9,5) | - |
| Síndrome de Sjögren | 1 (1,5) | - |
| Artritis reumatoide | 1 (1,5) | - |
Laboratory tests
Skin biopsy was performed to 25 (39.6%) patients, of whom 15 presented findings compatible with dermatomyositis; 24 patients (38.0%) underwent muscle biopsy, 18 showed findings consistent with this inflammatory myopathy (skeletal muscle with chronic perimysial inflammation, atrophy of muscle fibers, and in some cases vacuolization) and one was nonspecific; 35 (55.5%) patients had an electromyography, 25 showed decreased amplitude and velocity of the motor potentials; fasciculation and fibrillation potentials and positive sharp waves were evidenced in some cases, in addition to complex repetitive discharges. Seven patients had concomitantly muscle biopsy, skin biopsy and electromyography, and three of them presented findings suggestive of dermatomyositis in all the three examinations, of whom one presented only Gottron papules, other heliotrope erythema and poikiloderma, and the last one Gottron papules, heliotrope erythema, poikiloderma and photosensitivity. A chest CT scan was taken to 33 patients, seven had findings associated with the disease, among which it is worth highlighting interstitial infiltrates, bronchiectasis, pulmonary hypertension, fibrous tracts, organizing pneumonia, and interstitial pneumonia. An echocardiogram was taken to 16 patients, and six of them presented findings associated with this myopathy.
As for the immunology laboratory tests, the most frequently found was the antinuclear antibodies (ANA), in 41(65.0%) patients, being the granular (53.6%) and homogeneous(21.9%) patterns the most documented. In the second place, there are the extractable nuclear antigens (ENA), which were positive in eight (12.6%) patients, being anti-Ro found in moreoccasions. Lastly, two (3.1%) patients had positive anti Jo-1.
Creatine kinase (CK) was requested to all patients, 50(79.3%) presented an increase thereof (reference value:55−170 U/l). Transaminases were requested to 61 patients, 40(65.5%) had elevated ALT and 46 (75.4%) had elevated AST(reference value: ALT 14−54 U/l and AST 15−41 U/l). LDH was requested to 28 patients, 26 (92.8%) had it increased (reference value: 120−246 U/l), and of the 27 patients to whom aldolase was requested, it was elevated in 13 (48.1%) (reference value:0−7.6 U/l). Regarding acute phase reactants, erythrocyte sedimentation rate (ESR) was requested to 55 patients, which was positive in 46 (83.6%) cases (reference value: 0-20 mm/h), and C-reactive protein (CRP) was requested to 47 patients (reference value: less than 10 mg/l), which was positive in only five cases (10.6%). Of the total number of patients, five (7.9%) died from respiratory failure and one due to neurological causes (Table 4).
Table 4 Diagnostic tests.
| Clásica | Amiopática | |||
|---|---|---|---|---|
| Tipo de examen | Exámenes realizados | Exámenes positivos | Exámenes realizados | Exámenes positivos |
| Anti-Jo, n (%) | 33 (52,3) | 2 (6,0) | 1 (14,2) | - |
| Anti-Mi 2, n (%) | 1 (1,5) | - | - | - |
| ANA, n (%) | 49 (77,7) | 41 (83,6) | 6 (85,7) | 4 (57,1) |
| Homogéneo, n (%) | 9 (21,9) | 1 (25) | ||
| Periférico, n (%) | - | - | ||
| Nucleolar, n (%) | 3 (7,3) | - | ||
| Centromérico, n (%) | 1 (2,4) | - | ||
| Citoplasmático, n (%) | 2 (4,8) | 3 (75) | ||
| Granular, n (%) | 22 (53,6) | - | ||
| Ribosomal, n (%) | 1 (2,4) | |||
| No especificado, n (%) | 3 (7,3) | |||
| Anti-SM, n (%) | 40 | - | 6 | - |
| Anti-RNP, n (%) | 40 | 3 (7,5) | 6 | - |
| Anti-La, n (%) | 40 | 1 (2,5) | 6 | - |
| Anti-Ro, n (%) | 40 | 6 (15) | 6 | - |
| CK total-VR 55-170 U/l, n (%) | 63 | 50 (79,3) | 7 | 2 (28,5) |
| ALT-VR 14-54 U/l, n (%) | 61 | 40 (65,5) | 5 | 3 (60) |
| AST-VR 15-41 U/l, n (%) | 61 | 46 (75,4) | 5 | 3 (60) |
| LDH-VR 120-246 U/l, n (%) | 28 | 26 (92,8) | 2 | 2 (100) |
| Aldolasa-VR 0-7,6 U/l, n (%) | 27 | 13 (48,14) | 5 | - |
| VSG-VR 0-20 mm/h, n (%) | 55 | 46 (83,6) | 6 | - |
| PCR-VR menor a 10 mg/ml, n (%) | 47 | 5 (10,6) | 6 | - |
| Electromiografía, n (%) | 35 | 25 (71,4) | - | - |
| Biopsia de piel, n (%) | 25 | 15 (60) | 7 | 7 (100) |
| Biopsia muscular | 24 | 18 (75) | 1 | - |
| TAC de tórax | 33 | 7 (21,2) | 1 | - |
| Ecocardiograma | 16 | 6 (35,7) | - | - |
| ALT: alanina aminotransferasa; ANA: anticuerpos antinucleares; AST: aspartato aminotransferasa; CK: creatina cinasa; LDH: deshidrogenasa láctica; PCR: proteína C reactiva; TAC: tomografía axial computarizada; VR: valor de referencia; VSG: velocidad de sedimentación globular. | ||||
Treatment
Sixty (95.2%) patients received management with glucocorticoids, 30 (50%) required pulses of methylprednisolone and continued with oral prednisolone, while 30 (47.6%) received only oral prednisolone. Regarding immunomodulators, the most frequently used were azathioprine, in 35 patients (64.8%); methotrexate in 27 (50%); and cyclophosphamide in 11 (20.3%) (Table 5).
Table 5 Treatment.
| Clásica | Amiopática | Total | |
|---|---|---|---|
| Corticoides, n (%) | 60 (95,2) | 4 (57,1) | 64 (92,8) |
| Metilprednisolona, n (%) | 30 (50) | 1 (25) | 31 (52,5) |
| Deflazacort, n (%) | 2 (3,3) | - | 2 (2,8) |
| Prednisolona, n (%) | 60 (100) | 4 (100) | 64 (91,4) |
| Inmunomoduladores, n (%) | 54 (85,7) | 4 (57,1) | 58 (82,8) |
| Azatioprina, n (%) | 35 (64,8) | 1 (25) | 36 (51,4) |
| Metotrexate, n (%) | 27 (50) | 2 (50) | 29 (41,4) |
| Ciclofosfamida, n (%) | 11 (20,3) | - | 11 (15,7) |
| Gammaglobulina, n (%) | 8 (14,8) | - | 8 (11,4) |
| Cloroquina, n (%) | 5 (9,2) | 1 (25) | 6 (8,5) |
| Rituximab, n (%) | 4 (7,4) | - | 4 (5,71) |
| Ciclosporina, n (%) | 3 (5,5) | - | 3 (4,28) |
| Micofenolato, n (%) | 2 (3,7) | - | 2 (2,8) |
| Tofacitinib, n (%) | 1 (1,8) | - | 1 (1,4) |
| Un inmunomodulador, n (%) | 27 (42,8) | 4 (57,1) | 31 (53) |
| ≥ 2 inmunomoduladores, n (%) | 27 (42,8) | 0 | 27 (46) |
Discussion
Idiopathic inflammatory myopathies are a heterogeneous group of diseases that affect the musculoskeletal system and are usually accompanied by extramuscular involvement, due to interstitial lung disease, arthritis, or malignancy.(7 They are divided into dermatomyositis, polymyositis, inclusion body myositis, and other myositis, including eosinophilic, granulomatous, focal nodular, infectious, drug-induced, orbital, macrophagic myofascitis, myositis ossificans, hereditary myopathies associated with muscle inflammation and immune-mediated necrotizing myositis, among others.1
The classic form of dermatomyositis is characterized by the presence of symmetric proximal muscle weakness and dermatological manifestations; however, there is a variety in which muscle weakness is absent, known as amyopathic dermatomyositis,7 which occurs in between 10 and 20% of the patients.8 A study published in Italy in 2014, which included 103 patients with dermatomyositis, documented the amyopathic variant in 7.7% of patients; when comparing the age at onset of the disease, the authors evidenced that those with amyopathic dermatomyositis were younger at the time of diagnosis.9 In our study, it was reported a percentage of amyopathic dermatomyositis in accordance with the reports in the literature; however, contrary to the study mentioned above, these patients were older at diagnosis, compared with those with classic dermatomyositis.
Two incidence peaks of dermatomyositis have been described, the first between 5 and 15 years of age and the second between 40 and 60 years of age. It is considered that this is a disease that predominates in women, with a female:male ratio of 2:1.1 As for the demographic characteristics, in our study the mean age at diagnosis was similar to that reported in another study, published in 2012, which was conducted in Brazil and included 139 patients, in which it was reported an average age at the time of diagnosis of 41.7 years (SD ± 14.1).
Similar findings have been published in other countries, such as Japan, 47.4 years; Mexico, 34 years (SD ±15); France, 52 years; and Malaysia, 57.8 years (SD ± 11.1).10-14 In addition, we evidenced a predominance of the disease in women, which coincides with what has been reported so far in studies carried out in Singapore, Mexico, France, Taiwan and Japan.11-13,15,16) In Colombia, a study similar to ours was carried out in 2014, which included 30 patients with dermatomyositis and 16 with polymyositis, with a slightly higher female:male ratio.17
Regarding the dermatological manifestations, it has been described in several studies that heliotrope erythema and Gottron papules are the most frequent signs, which is consistent with our results.10,16,18,19 The percentages of frequency of periungual telangiectasia and calcinosis cutis tend to be similar to those reported by us, as well as in the study published by De Souza et al.10 in Brazil, with 6.5% of patients with calcinosis cutis, and in the study conducted by Sato et al.,18 also in Brazil, with 5.3% of the patients with calcinosis cutis and 38.2% with periungual telangiectasia. However, in our study, the patients presented less photosensitivity (22.2%) and holster sign (17.4%), in addition to higher frequency of the shawl sign (30.1%) and the V sign (47.6%) with respect to what was published by De Souza et al.10 in Brazil, with 15.1% of the patients with the V sign and 14.4% with the shawl sign; by Sato et al.,18 also in Brazil, with 50.6% of the patients with photosensitivity; by Vega et al.17 in Colombia, with the shawl sign in 16% of the patients and the holster sign in 26.6%; in addition to what was published by Hoesly et al.20 in the US, with 22.1% of the patients with the shawl sign.
With regard to systemic manifestations and constitutional symptoms, dysphagia, interstitiallungdisease and weight loss were the most frequent. InaEuropeanstudypublishedin2011, interstitial lung disease was documented twice as frequently as that was found in the present study, in addition to higher associated morbidity and mortality in these patients.21 several studies coincide in that gastrointestinal and pulmonary manifestations, and weight loss are the more prevalent.18,20,22,23
As part of the variables studied, elevation of at least one of the muscle enzymes was documented in 85% of the patients, a value lower than that found in other studies.14,18 Within muscle enzymes, CK is the one that is most frequently elevated, the other results are variable in different articles.13,15,19 Generally, transaminases are elevated in similar proportions, with AST usually being higher than ALT.13,23
ANAs were positive, with a lower percentage than ours, in three Brazilian studies: the first, published by De Souza et al.,10 which included 139 patients with dermatomyositis, of whom 62.6% had positive ANAs; the second, by Sato et al.,18) which included 189 patients with juvenile dermatomyositis, of whom 41.4% had positive ANAs and, finally, a study conducted by Sallum et al.,24 which included 39 patients with juvenile dermatomyositis, of whom 40% presented positive ANAs.10,18,24 Several articles have documented a higher frequency of granular and homogeneous fluorescence pattern, which is consistent with our results.10,17
Unlike the results of a Brazilian study published in 2009, which reported findings suggestive of dermatomyositis in 93.2% of electromyographies, 91.5% of muscle biopsies, and 77.3% of skin biopsies18 we found a lower proportion of electromyographies (71.4%), which is consistent with a study conducted in Singapore, in which 79.4% of patients with electromyiographies were reported.15
As for the treatment, 95.2% of our patients were managed with oral or intravenous glucocorticoids; similar proportions have been documented so far in Asia, Mexico and Brazil.10,11,13,14 With reference to maintenance therapy, most of the patients in our study received at least one immunomodulator; among the immunomodulators, the most frequently used, according to a study carried out in Brazil that included 139 patients, are azathioprine and methotrexate,10 which coincides with our results.
In our study, concomitant connective tissue diseases were evidenced in 17% of the patients, which is consistent with data documented in Asia.15 Most of the concomitant dis-eases were lupus and systemic sclerosis; until now, no studies have been documented showing these two entities predominantly, however, in a study conducted in Brazil, published in the year 2000, which included 59 patients with dermatomyositis and 43 patients with polymyositis, in the group of patients with dermatomyositis, systemic sclerosis was documented in seven patients and rheumatoid arthritis in one.22 In addition, in a study published in Singapore, which included 40 patients with dermatomyositis and 35 with polymyositis, 10 of them presented association with systemic lupus erythematosus, four with rheumatoid arthritis, and one with systemic sclerosis; in total, 21.4% of the patients concomitantly presented another connective tissue disease. Finally, in the study published by Sato et al., which included 189 patients, eight presented rheumatoid arthritis, two presented systemic lupus erythematosus, and one had systemic sclerosis.15,18
It is estimated that approximately 15% of patients with dermatomyositis diagnosed after the age of 40 years will present a neoplasm three to five years after the diagnosis, the most common being colorectal, ovarian, lung, pancreatic, and gastric carcinomas.25 In a study conducted in Stockholm, Sweden, published in 1992, which included 392 patients with dermatomyositis, a relative risk of cancer of 2.4 (95% CI: 1.6-3.6) was documented in men and of 3.4 (95% CI: 2.4-4.7) in women.26) Our study found a percentage of patients with cancer similar to that reported in the studies conducted by Scola et al.22 in Brazil (8.4%) and by Chen et al.23 in China (11.1%). In contrast, other studies have reported higher percentages of malignancy, such as those of Hiketa et al.13 in Japan (16.5%), Fardet et al.12) in France (23%) and Hoesly et al.20 in the US. (23%).
With regard to mortality, in a study published in 2018, which included 982 patients hospitalized with a diagnosis of dermatomyositis and polymyositis in China, it was documented the death of 63 of them during hospitalization or two weeks after discharge, with a calculated mortality rate of 6.4%, being pulmonary infection and exacerbation of interstitial lung disease27 the two most frequent causes of death, which resembles our results. However, in a retrospective study conducted in the US, which included 15,407 patients (10,023 with a diagnosis of dermatomyositis and 5384 with polymyositis), a mortality rate of 4.4% was found in the group diagnosed with dermatomyositis (449 deaths), a percentage lower than ours.28
Given that our study collected the data retrospectively, within the limitations it is important to mention that it was not possible to obtain follow-up data, in order to determine the prognosis of the patients. Data were taken from electronic medical records, which may limit their collection, especially those which make reference to clinical characteristics. Not all patients underwent the same paraclinical tests, however, it is a reflection of the clinical practice, in which the request for diagnostic tests is related to the clinical picture of the patients. Finally, it should be noted that this is so far the study with the largest number of patients with dermatomyositis in Colombia.
Conclusion
The main demographic characteristics, and dermatological and systemic manifestations of a group of patients with dermatomyositis in a university hospital in Colombia are presented. The majority of the data obtained are consistent with information from other case series studies worldwide. Despite the fact that heliotrope erythema, Gottron papules, and Gottron's sign have been defined as pathognomonic manifestations, in accordance with what was proposed in the narrative reviews by Mainetti et al. and DeWane et al.,1,6 in our study we found that the most frequent manifestations were Gottron papules, heliotrope erythema and poikiloderma. The population evaluated presented a lower proportion of photo-sensitivity and holster sign, in addition to a higher frequency of the shawl sign and the V sign, compared with other studies.











 text in
text in